Case Report
Volume 2 Issue 1 - 2020
The UBM Characteristics of Late Capsular Block Syndrome before and After Treatment: A Case Report
Department of Ophthalmology, Shijiazhuang First Hospital, Shijiazhuang, Hebei, China, No. 12 Pingan North Street, Shijiazhuang
*Corresponding Author: Guangxian Tang, Department of Ophthalmology, Shijiazhuang First Hospital, Shijiazhuang, Hebei, China, No. 12 Pingan North Street, Shijiazhuang.
Received: January 07, 2020; Published: January 14, 2020
Abstract
To explore the characteristics of Capsular block syndrome (CBS) by ultrasound biomieroseopy (UBM) technique and to discuss the diagnosis of CBS through the application of UBM. A 78-year-old man who had phacoemulsification and intraocular lens implantation developed CBS with secondary glaucoma 18 years after surgery. UBM technique could explore the characteristics and the diagnosis of CBS. The glaucoma was resolved and IOP was declined after the performance of neodymium: YAG laser anterior capsulotomy and glaucoma drainage valve implantation surgery. The atypical CBS secondary to glaucoma that could not be diagnosed by slit lamp examination may be diagnosed by UBM examination.
A 78-year-old man complainted of intermittent distending pain, blurred vision in the right eye for 1 years and aggravated for 1 months at the first visit. He had a history of the right and left eye phacoemulsification and intraocular lens implantation 18 years and 10 years ago, respectively. The intraocular pressure (IOP) in the right and left eye was 37 mm Hg and 14 mm Hg, respectively; visual acuity were 20/80. On slit lamp examination, the central anterior chamber depth (ACD) and the peripheral anterior chamber (PAC) depth were asymmetry, ACD in the right and left eye was 4CT and 6CT, PAC in the right and left eye was 1/5CT and 1CT, respectively. No obvious abnormality was found. UBM showed: in the right eye anterior chamber angle was narrow, peripheral anterior synechiae (PAS) were acquired adhesions between the corneoscleral coat and the peripheral iris.
The IOL and iris were attached to the anterior capsule. The cyst around the periphery of the capsule formed a capsular bag, and the envelope expanded to the periphery. The volume of the bag was highly expanded, which is full of uneven moderate reflection signals (Figure 1). A neodymium: YAG (Nd:YAG) laser peripheral anterior capsulotomy was performed immediately. As soon as the capsulotomy was made, the distended capsule collapsed and the opacified contents gushed into the vitreous body. UBM showed: in the right eye, the capsule and the anterior communicating, anterior membrane opening unobstructed, anterior chamber small gray haze floating, the average depth of anterior chamber deepened, posterior capsule and intraocular lens after surface mount (Figure 2). After the Nd:YAG capsulotomy, Slit lamp examination showed a deep anterior chamber; the IOL was adherent to the anterior capsule opening, the anterior chamber depth had increased to 2.78mm, but IOP did not decrease because of the adhesions between the corneoscleral coat and the peripheral iris, the IOP declined after glaucoma drainage valve implantation surgery were performed.
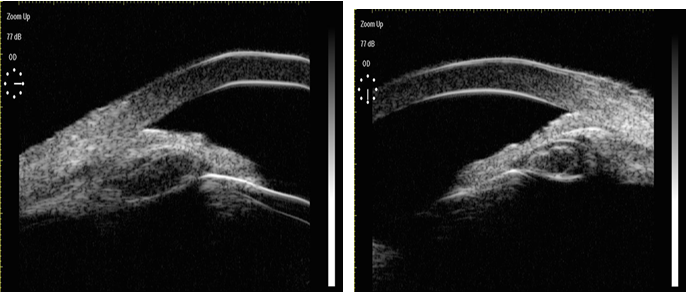
Figure 1: In the right eye,anterior chamber angle was narrow, The cyst around the periphery of the capsule forms a capsular bag, and the envelope expands to the periphery. The volume of the bag is highly expanded, which is full of uneven moderate reflection signals.
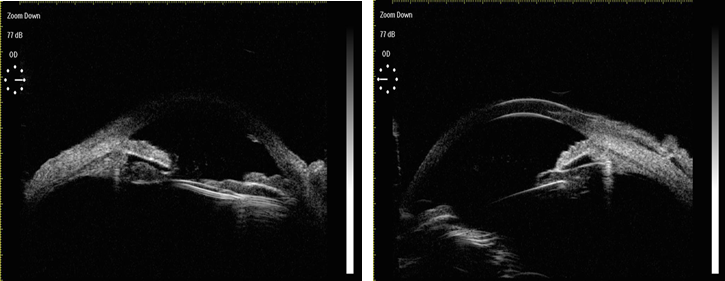
Figure 2: The capsule and the anterior communicating, anterior membrane opening unobstructed, anterior chamber small gray haze floating, the average depth of anterior chamber deepened.
Discussion
CBS is a class of postoperative complications associated with continuous curvilinear capsulorhexis. Miyake et al. [1] classified CBS into 3 groups: intraoperative, early postoperative, and late postoperative. Although each group has a different pathogenic mechanism, they share the feature that the capsulorhexis diameter is less than IOL optical diameter. When the lens nucleus or IOL optical surface mechanical obstruction leads to the formation of capsular liquid cavity closure, residual viscoelastic material, lens epithelial cells, undergo metaplasia and proliferation, producing numerous types of collagen and extracellular substances that eventually accumulated in the capsule, These substances form a cross penetration capsule pressure gradient so that the aqueous humor is absorbed into the bag until the osmotic pressure inside and outside reaches a balance, the final liquid substance clouding of the lens capsular bag back into the expansion of the anterior vitreous cavity [1] It is also possible that the aqueous humor can be inserted into the pouch of the lens in the eye when the eyeball is sopping up, due to the flap like structure formed by the IOL optical part and the edge of the capsulorhexis [2].
The result is a series of ocular changes, shallow anterior chamber, increasing IOP, posterior capsular rupture, lens nucleus sinking, iris posterior synechia, after-cataract, diopter change (myopia) and secondary glaucoma [3]. With the understanding of CBS and the application of UBM, CBS is not rare complication of capsulorhexis. Therefore, according to the diameter of the lens nucleus and the IOL optical surface, we should determine the suitable diameter of the circular capsulorhexis, meticulously, gently and thoroughly remove the viscoelastic agents, and provide effective anti-inflammatory treatment after operation, so as to prevent CBS. The use of Nd: YAG laser treatment methods is safe and effective according to the time and clinical characteristics of CBS after cataract surgery [4].
The right eye of the patient was performed phacoemulsification and intraocular lens implantation of 18 years ago. It is easy to misdiagnose if the slit lamp examination did not check into the capsular swelling, backward, posterior to the intravitreal bulging CBS typical symptoms. But the UBM examination can be diagnosed clearly. Therefore, UMB can be used as an important auxiliary examination for the CBS. It can be help to clinical diagnose and evaluate the therapeutic effect.
References
- Miyake K, Ota I, Ichihashi S, et al. (1998). New classification of capsular block syndrome. J Cataract Rafract Surg, 24.9: 1230-1234.
- Zacharias J. (2000). Early post operative capsular block syndrome related to saccadic-eye-movement-induced f luid flow into the capsular bag. J Cataract Refract Surg, 26: 415-419.
- Davison JA. (1990). Capsular bag distensi on aft er endophacoemulsification and posterior chamber in traocular lens implan tation. J Cataract Refract Surg 16: 99-108.
- Wang YZ, Xu JJ. (2012). Efficacy analysis on Nd: YAG laser treatment of capsular block syndrome after cataract surgery. Guoji Yanke Zazhi Int Eye Sci, 12,2: 339-340.
Citation: Xiaowei Yan, Guangxian Tang, Hengli Zhang and Fan Li. (2020). The UBM Characteristics of Late Capsular Block Syndrome before and After Treatment: A Case Report. Journal of Ophthalmology and Vision Research 2(1).
Copyright: © 2020 Guangxian Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
