Mini Review
Volume 4 Issue 1 - 2022
The Detained Diaphoresis- Fox-Fordyce Disease
A.B. Diagnostics A-1, Rajouri Garden, New Delhi 110027 India
*Corresponding Author: Anubha Bajaj, A.B. Diagnostics A-1, Rajouri Garden, New Delhi 110027 India.
Received: October 21, 2021; Published: Febraury 04, 2022
Preface Fox-Fordyce is an exceptional, chronic, gradually progressive, inflammatory cutaneous disorder demonstrating a pruritic, papular eruption confined to apocrine gland predominant zones as the axillae, areolae or anogenital region. Fox-Fordyce disease was initially scripted by George Fox and John Fordyce in 1902.
Fox-Fordyce disease is additionally denominated as apocrine miliaria, apocrine duct occlusion, chronic pruritic papular eruption or sweat retention disease. Obstruction of apocrine gland duct on account of accumulated keratin within the follicular infundibulum is preeminent, where entrapped, apocrine gland induced sweat engenders inflammation [1].
Disease Characteristics Post pubertal females between 13 years to 35 years are commonly implicated although the disease is exceptionally discerned in children, male subjects, pre-pubertal or postmenopausal subjects [2,3].
Lesions may mitigate or undergo remission within the pre-pubertal or postmenopausal phase. Premenstrual disease exacerbation and amelioration with pregnancy, menopause or with oral contraceptive pills may be observed [2,3].
Typically, Fox-Fordyce disease is a sporadic disorder. Infrequently, the disorder may appear as a familial condition within sisters, monozygotic female subjects, male twins or father- daughter combination [2,3]. Commonly, lesions are discerned in areas with predominant apocrine glands as the axilla, pubic or anogenital regions. Besides, lesions within the thoracic or abdominal region, lips, umbilicus, perineum, nipple, areola, medial upper thigh or lower limbs may appear infrequently. Bilateral cutaneous lesions are characteristic [2,3].
Of obscure aetiology, Fox-Fordyce disease is engendered when apocrine gland induced sweat is entrapped due to a keratotic spigot within the hair follicle. Ruptured, seeping, epidermis-lined, apocrine gland sweat ducts initiate inflammation with accompanying intense pruritus [2,3]. Fox-Fordyce disease may be engendered due to altered or increased sweating, emotional or hormonal factors, hair eradication or genetic inheritance. Aforesaid factors may contribute to obstruction of apocrine glands, retention of sweat and consequent inflammation [3,4].
Comedogenic acne upon the face or trunk, menstrual alterations, amenorrhea or polycystic ovaries may coexist with Fox-Fordyce disease. Androgens may alter keratinocyte adhesion, composition of sweat and may influence associated factors [3,4].
Factors such as elevated environmental temperature, humidity, physical activity, stress, excitement, friction with clothing, laser hair removal and exposure to intense pulsed light may contribute to disease emergence [3,4].
Disease Pathogenesis Of obscure pathogenesis, occlusion of apocrine gland ducts with accumulated keratin within the follicular infundibulum is pivotal. Hyperkeratotic epithelial cores disrupt follicular infundibula within incriminated cutaneous surfaces, a feature which appears fundamental to aforesaid hypothesis [3,4].
Ruptured apocrine gland ducts may engender inflammation. Laser hair reduction appears to initiate identical modifications [3,4].
Fox-Fordyce disease comprises of obstructed apocrine gland ducts as discerned upon histology of occluded intra-epidermal sweat ducts with detached apocrine secretory cells [3,4]. Hormonal, physical, environmental factors, hyperhidrosis with exercise, humid climate, occlusive clothing, sexual activity or emotional stress induces disease exacerbation [3,4].
Retained secretions with consequent rupture of glandular structures and secondary inflammation within the dermis is encountered. Extravasation of glandular secretions induces pruritus and commonly precedes the emergence of papules [5,6].
Clinical Elucidation Fox-Fordyce disease characteristically displays multiple, skin coloured, pruritic, dome- shaped papules or nodules circumscribing hair follicles. Incriminated individuals may manifest hyperhidrosis and bilateral, multiple, mildly or intensely pruritic, axillary or ano-genital papules [5,6]. Localized, bilateral, asymmetric, yellowish brown, follicular, punctate, papules with a smooth, uniform surface may be observed within specified zones. Hair bearing regions as the axilla or genitalia may display a follicular distribution of skin coloured, punctate, crusted papules of around one millimetre to two millimetre diameter [5,6].
The condition is associated with intense, sleep disturbing pruritus although asymptomatic instances may be discerned [5,6].
Fox-Fordyce disease depicts bilateral, dome- shaped, flesh coloured or reddish, miniature papules comprehensively incriminating hair follicles of the diseased area [5,6].
Characteristic cutaneous eruption associated with Fox-Fordyce disease exemplifies extensive pruritus which exacerbates with sweating, hyperhidrosis, stress or anxiety [5,6].
Lichenified or hyper-pigmented, inspissated, shrivelled, pruritus induced cutaneous surfaces with decimated or absent sweating may be observed [5,6].
Chronic lesions of Fox-Fordyce disease may manifest as lichenified, thickened, coarse, hyper-pigmented cutaneous surface, consequent to scratching induced by severe pruritus. Severe instances are associated with localized anhidrosis and brittle, sparse or absent hair due to eradication of apocrine glands and associated hair follicles [5,6].
Primary lesions appear as dome-shaped, flesh coloured, yellowish, reddish or violaceous, follicular or perifollicular papules of 2 millimetres to 3 millimetres magnitude. The aggregated papules or nodules circumscribe dense, linear, apocrine gland predominant zones as axillary, areolar, perianal or genital region. Hypotrichosis, hyperkeratosis and excoriation due to pruritus may be observed [5,6].
Histological Elucidation Upon microscopy, a keratotic spigot appears where apocrine duct merges with the hair follicle. Spongiosis and vesicle configuration occurs within the follicular infundibulum and superimposed epidermis. Additionally, a mild to moderate perifollicular inflammatory infiltrate comprised predominantly of neutrophils and chronic inflammatory cells is discerned which is admixed with xanthomatous, foamy macrophages [7,8].
A distended follicular infundibulum obstructed with keratin and enmeshed within a chronic inflammatory lymphocytic and histiocytic infiltrate along with xanthomatous or foamy macrophages is discerned.
Dilated follicular infundibula, hyperkeratotic superficial stratified squamous epithelial layer, perifollicular distribution of xanthomatous histiocytes and a discrete, chronic inflammatory infiltrate of lymphocytes may be observed along with intra-follicular mucin accumulation [7,8].
Nonspecific histological features as intra-follicular corneal plug, hyperkeratosis and spongiosis of superimposed stratified squamous epithelium, retention vesicles, dilated apocrine glands with accumulated mucin and perifollicular lymphocytic and histiocytic inflammatory infiltrate are exemplified(7,8).
Additionally, infundibular dyskeratotic epithelial cells, vacuolar alterations and significant parakeratosis may be observed. Nevertheless, foamy or xanthomatous histiocytes with perifollicular xanthomatosis is a distinctive and consistent feature of Fox-Fordyce disease [7,8].
A spigot of hyperkeratotic stratified squamous epithelium occludes follicular infundibulum and excretory duct of incriminated apocrine gland. Spongiotic vesicles appear upon the site of accumulated apocrine secretions proximal to keratotic spigot within the distended excretory duct with consequent rupture [7,8].
Fox-Fordyce disease typically enunciates perifollicular infiltration of lymphocytes and foamy histiocytes with resultant hair loss. Commonly, lymphocytes invade the ductal epithelium and circumscribing ductal tissue. Obstruction of apocrine gland ducts within the intra-epidermal portion of apocrine sweat duct may be observed [7,8].
Peri-ductal lymphocytic and histiocytic inflammatory infiltrate frequently demonstrates a component of mast cells. Perifollicular fibrosis and dyskeratotic cells may appear within the follicular infundibulum [7,8]. Perifollicular foamy macrophages or xanthomatous cells are pathognomonic of Fox-Fordyce disease [7,8].
Periodic acid Schiff’s (PAS) stain demonstrates a similarity between apocrine gland secretions and cytoplasm of foamy macrophages [7,8]. Upon Alcian-blue or mucin staining, intra-follicular or apocrine gland mucin accumulates may be discerned [7,8].
Peripheral or perifollicular xanthomatous histiocytes are intensely immune reactive to CD68 [7,8]. However, xanthomatous cells are immune non reactive to carcinoembryonic antigen (CEA) and epithelial membrane antigen (EMA) [7,8].

Figure 1: Fox-Fordyce disease demonstrating dome-shaped, flesh coloured, miniature papules within apocrine gland zones [12].

Figure 2: Fox-Fordyce disease exhibiting a layer of stratified squamous epithelium with hyperkeratosis, acanthosis and spongiosis with a subjacent inflammatory infiltrate of lymphocytes and xanthomatous histiocytes [13].
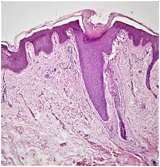
Figure 3: Fox-Fordyce disease exemplifying a layer of stratified squamous epithelium with acanthosis, hyperkeratosis and an underlying chronic inflammatory infiltrate surrounding apocrine glands [14].
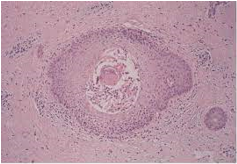
Figure 4: Fox-Fordyce disease enunciating an apocrine gland plugged with secretions circumscribed by acanthotic, hyperkeratotic stratified squamous epithelium and an intermingled chronic inflammatory infiltrate [15].
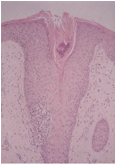
Figure 5: Fox- Fordyce disease delineating an apocrine gland plugged with secretions along with a lining of acanthotic stratified squamous epithelium and commingled chronic inflammatory infiltrate [16].
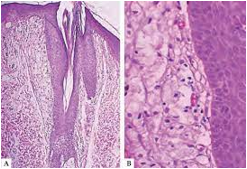
Figure 6: Fox-Fordyce disease depicting obstructed apocrine gland layered with stratified squamous epithelium with acanthosis and hyperkeratosis and an admixture of small lymphocytes with xanthomatous histiocytes [17].
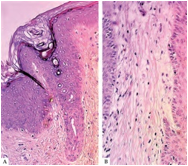
Figure 7: Fox- Fordyce disease demonstrating occlusion of apocrine gland lined with acanthotic, hyperkeratotic stratified squamous epithelium and intermixed lymphocytes with xanthomatous cells [17].
Differential Diagnosis Fox-Fordyce disease requires a segregation from conditions such as folliculitis, pseudo-folliculitis, miliaria rubra or profunda, milia, granular parakeratosis, syringoma, acanthosis nigricans, Graham-Little-Piccardi-Lasseur syndrome, Darier's disease, Hailey-Hailey disease, trichostasis spinulosa, lichen nitidus, lichen amyloid or papular mucinosis(8,9).
Investigative Assay Fox-Fordyce disease can be appropriately discerned with a comprehensive clinical history and cogent physical examination of the rash(8,9).
Upon dermoscopy, Fox-Fordyce disease delineates folliculo-centric papules, multiple light brown to darkish structure-less zones which are devoid of pigment network and a centric, hyperkeratotic spigot obstructing the papules. Papules circumscribing hair follicles, traumatized terminal hair or blackheads may be discerned [8,9].
Cutaneous tissue sampling necessitates serial sectioning wherein characteristic histological features may be observed besides a pathognomonic morphology with perifollicular foamy macrophages [8,9]. High-definition optical coherence tomography (HD-OCT) with axial or slice imaging exhibits distinct epidermal lesions extending into upper dermis. Intra-lesional, distended, ductal articulations appear enmeshed within fluid levels [9,10].
Therapeutic Options Fox-Fordyce disease is unresponsive to pertinent therapies. Treatment strategies are inadequate or partially efficacious as clinical symptoms persist and lesion reoccurrence is frequent [10,11]. Treatment methodologies pertain to decimation of inflammation, sweating, circumventing ductal occlusion and adoption of procedures which eradicate sweat glands [10,11]. Efficacious topical medication remains the initial, preferred mode of therapy [10,11]. Diverse treatment methodologies adopted are topical or oral retinoids, topical benzoyl peroxide, topical calcineurin inhibitors (CNIs), topical or intralesional corticosteroids, topical or oral antibiotics or topical clindamycin and oral contraceptives which induces a comprehensive resolution of lesions. Topical clindamycin may be moderately beneficial with amelioration of clinical symptoms [10,11]. Response to therapy may be partial and lesions with pertinent clinical symptoms may reappear or persist [10,11].
Alternative, contemporary, novel therapeutic modalities which may be adopted in severe instances are surgical extermination of the lesion, botulinum toxin, phototherapy, electrocoagulation, fractional laser therapy as 1550 nm erbium glass pulsed dye laser, carbon dioxide (CO2) laser, copper vapour, liposuction-assisted curettage and microwave technology [10,11].
Fox-Fordyce disease may persist for several years. The condition may be alleviated in pregnancy or menopause or manifest a disease continuum. Reoccurrence of lesions may ensue following cessation of therapy [10,11].
References
- Barber HW. (1922). “Case of Fox-Fordyce Disease”. Proc R Soc Med 15: 44-5.
- Litchman G, Sonthalia S. (2021). “Apocrine Miliaria”. Stat Pearls International Treasure Island, Florida.
- Vega-Memije ME, Pérez-Rojas DO et al. (2018) “Fox-Fordyce disease: report of two cases with perifollicular xanthomatosis on histological image”. An Bras Dermatol 93(4): 562-565.
- Sammour R, Nasser S et al. (2016). “Fox-Fordyce Disease: An under-diagnosed adverse event of laser hair removal?” J Eur Acad Dermatol Venereol 30(9): 1578-82.
- Bernad I, Gil P et al. (2014). “Fox Fordyce disease as a secondary effect of laser hair removal”. J Cosmet Laser Ther 16(3):141-3.
- Blasco-Morente G, Naranjo-Díaz MJ et al. (2016). “Fox-Fordyce Disease”. Sultan Qaboos Univ Med J 16(1): e119-20.
- Liu WC, Cao T et al. (2016). “In vivo features of Fox-Fordyce disease in high-definition optical coherence tomography”. J Dtsch Dermatol Ges 14(1): 62-3.
- Kaya Erdo?an H, Bulur I et al. (2015). “Clinical Effects of Topical Tacrolimus on Fox-Fordyce Disease”. Case Rep Dermatol Med 2015: 205418.
- Han HH, Lee JY et al. (2016). “Successful treatment of areolar Fox-Fordyce disease with surgical excision and 1550-nm fractionated erbium glass laser”. Int Wound J 13(5): 1016-9.
- Uzuncakmak TK, Karadag AS et al. (2016). Effective treatment of Fox-Fordyce disease with pulsed dye laser”. Photodermatol Photoimmunol Photomed 32(5-6): 311-313.
- González-Ramos J, Alonso-Pacheco ML et al. (2016). “Successful treatment of refractory pruritic Fox-Fordyce disease with botulinum toxin type A” Br J Dermatol 174(2): 458-9.
- Image 1 Courtesy: Health jade
- Image 2 Courtesy: Semantic scholar
- Image 3 Courtesy: Karger publisher
- Image 4 Courtesy: JAAD.com
- Image 5 Courtesy: Science direct
- Image 6 and 7 Courtesy: Scielo Brasil.com
Citation: Anubha Bajaj. (2022). The Detained Diaphoresis- Fox-Fordyce Disease. Journal of Biotechnology and Immunology 4(1).
Copyright: © 2022 Anubha Bajaj. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
