Case Report
Volume 1 Issue 1 - 2019
Rarely reported- Wandering intravitreal worm of Brugia malayi from Central India
MGM Eye Institute, Raipur, 5th Mile, Vidhan Sabha Road, Raipur(C.G) -493111
*Corresponding Author: Gitumoni Sharma, MGM Eye Institute, Raipur, 5th Mile, Vidhan Sabha Road, Raipur(C.G) -493111.
Received: August 29, 2019; Published: September 10, 2019
Abstract
Aim: To report a case of live extraction of a intravitreal worm.
Methods and Result: Intravitreal worms are rarely reported. Central India is endemic for filariasis, we don't see such cases.We saw two such cases in 14 yrs. The parasites route of entry into the vitreous is unknown, may occur via choriocapillaries, retinal vessels or optic nerve. There was no systemic filariasis in this case. Presence of parasite in the vitreous causes structural retinal damage with vitritis and posterior uveitis which was present in this case. The definitive treatment is removal of the parasite. This report of live intravitreal worm, which is extracted live, the procedure explained and identified by morphogy and microscopy as Brugia malayi. The PO prognosis is good when patient is dewormed along with treatment for uveitis.
Conclusion: This case of intravitreal Brugia malayi is the third one reported from India. From this place this is the second reported case. Elimination of filariasis by 2020 under NHM will be possible with timely diagnosis and proper management.
Keywords: Intravitreal filariasis; Brugia malayi; Filarial endemicity
Introduction
Intraocular infestation by the filarial worm is a rare occurrence in humans. Most of the published reports are from south-east Asia. [1] Recently, photo essay of Retina journal in August 2016 had showed an intravitreal case. [2] India had reported one case of intravitreal filariasis in 2008. [3] Here we report a case of wandering worm in the vitreous cavity which was identified as Brugia malayi after examination following its live removal from the vitreous.
Case Report
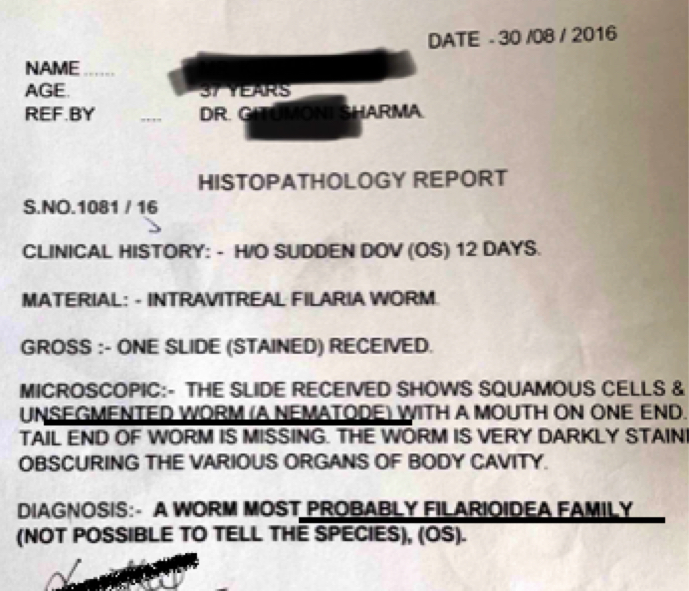
A 37year old male who is a farmer residing in central India presented to us with complaints of sudden painless decrease in vision in left eye since 12 days. His vision was 20/300 < N36 in the left eye. He had left exotropia 15°. Slit lamp examination showed +1 cells and flare in the anterior chamber with grade IV AC depth. Pupil was 3mm round and regular reacting to light. Dilated fundus examination showed vitritis ++ with multifocal retinochoroiditis with live worm seen wandering in the mid vitreous cavity. Figure 1 & Figure 2.
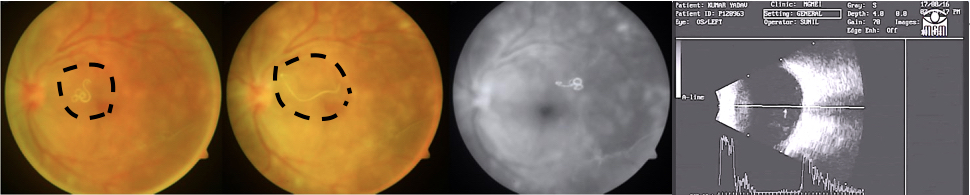
Figure 1: Wandering intravitreal worm in fundus camera.
Figure 2: B-Scan showing wandering parasite in the mid vitreous cavity
Figure 2: B-Scan showing wandering parasite in the mid vitreous cavity
Patient underwent 25 guage micro incision vitrectomy. Limited vitrectomy was done and the vitreous strands surrounding the white thread like glistening cylindrical worm was utilized for grasping it with forcep. Figure 3. The parasite is then transferred to formalin vial and sent for morphological and microscopic examination. Figure 4.

Figure 3: Intraoperative photograph, the parasite is being removed with micro forcep.
Figure 4: Worm measuring 6.05mm after removal transferred to formalin and sent for HPE.
Figure 4: Worm measuring 6.05mm after removal transferred to formalin and sent for HPE.
It was stained with lacto phenol blue and observed under coverslip and 40X illumination in the light microscope. It measured 6.05cm against a ruler. The body had twisted curves appeared non- segmented smooth with irregular kinks at places, with cuticle around, which was coming out at places due to handling probably during processing and slightly swollen head with oral opening with double style. The cephalic space length to width ratio is 2:1. Ventrally coiled tail was grasp opened and seen under microscope as pointed with the excretory and secretory pores. Figure 5.
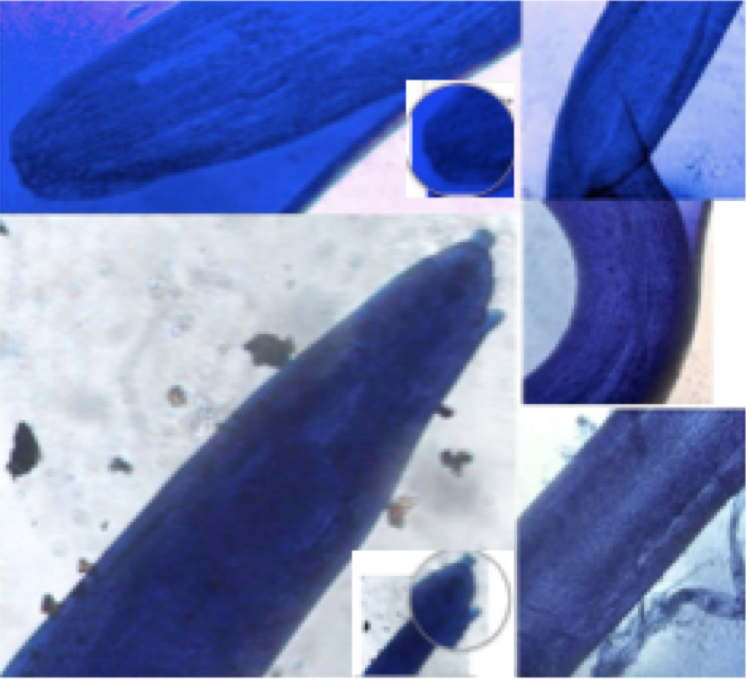
Figure 5: Swollen head end with 2 stylets, pointed caudal end showing the excretory and secretory pore. body of the worm with irregular kinks and body of the worm with cuticle coming out.
By this the worm can be diagnosed as adult Brugian filarial worm and most probably Brugia malayi as this is the only other filarial worm found in the Indian subcontinent according to the literature. [4] The worm was sent for HPE further examination which confirmed it to be of Filaroidea family. Figure 6. Post operatively patient had BCVA of 20/126, N24 vision with other parameters normal. OCT -macula was normal contour with mild foveal thinning. The right eye was normal all throughout.
Discussion
Brugia malayi is a helminth of class Nematodes (roundworm), one of the threecausative agents of lymphatic filariasis also called elephantiasis in humans. The two other filarial causes of lymphatic filariasis are Wurcheria bancrofti and Brugia timori, which both differ from B.malayi morphologically, symptomatically, and in geographical extent. [4] B. malayi is transmitted by Mansonia mosquitoes and is restricted to South and Southeast Asia. Central India is also endemic.
The most common clinical presentation of ocular filarial infestation is chemosis, lid edema orbital cellulitis, anterior uveitis or worm in the anterior chamber. But, only one case of intravitreal adult Brugian filarial worm has been found by Medline search. Rarely, microfilarae move out of lymphatics or blood circulation and can come to extravascular sites like the eye (vitreous cavity). The exact mode of entry of such helminths into the vitreous cavity is not known. The possible modes may be from choriocapillaries through the retinal layers as in a few reported cases of intravitreal Gnathostomiasis or through the optic nerve head. [5] Once a parasite is identified in the vitreous cavity it should be removed immediately, live and intact.
Live nematodes that have been found to affect the eye include Loa loa, Onchocerca, Gnathostoma, Angiostrongylus, Toxocara (visceral larva migrans), Wuchereria bancrofti, Ascaris, Brugia malayi, and Thelazia. Intraocular filariasis also there is approximately 100 cases reported. [6] Intravitreal filariasis reported till now are few with one or two case series also.7 Intravitreal Wurcheria reported are 1 or 2. [8] The first recorded case of B.malayi microfilaria in a patient with uveitis in the anterior chamber was reported by Anandakanan and Gupta in 1977 in India. [9] Rao et al reported first intravitreal live adult Brugian filarisis from Orissa which was removed by pars plana vitrectomy and identified by light microscopy and immunochromatrographic test. [10] Here is the second report of intravitreal Brugia malayi infestation where the live removal of the parasite was done by 25 gauge pars plana vitrectomy and identified by light microscopy and diagnosed by exclusion.
The color of the parasite was white, excluded is Gnathostoma which will be transparent. How it was differentiated from Wurcheria as it will be larger, transparent, smoothly curved, with single stylet with not so swollen head and a pointed tail. Brugia timori is not found in India.
It is to be mentioned that we saw similar case of intravitreal worm also in 2011. However, we could not do further microscopic evaluation for definitive diagnosis by seeing the different body parts and also tell the sex of the worm. There is no proper microscopic intraocular instrument available to safely remove the worm because while removal, it was moving vigorously and was difficult to grasp for continuous slipping. Inspite of cautious transfer to the formalin vial, it would have been lost intraoperatively for want of proper forcep. While removal and processing also probably, few of the parts must have been torned as is reported by the microbiologist. We did not do Giemsa staining which would have identified the sheath distinctly and the nuclei also. PCRbased study, Immunochromatographic rapid dipstick test or ELISA based assay was not available.Recently, LAMP (loop mediated isothermal amplification) assay has also been described.
The drug of choice for lymphatic filariasis is diethylcarbamazine (DEC). This regimen clears microfilariae from the blood and has a limited but definite effect on adult parasites. Use of ivermectin, in trials for therapy for lymphatic filariasis, in a single dose, appears to be as effective as DEC at clearing microfilariae. Combined treatment using albendazole plus ivermectin or albendazole plus diethylcarbamazine has resulted in near-zero microfilaremia levels for at least one year. Based on these new developments, the World Health Assembly adopted a resolution calling on member states to work for the elimination of lymphatic filariasis as a public health problem. It is one of the tropical diseases targeted for elimination by the year 2020 by the WHO. One of the control measures is mosquito eradication. Mansonia species are the major vectors in rural areas. Control of mansonia mosquitoes is by destruction or removal of the aquatic vegetation.
Conclusion
This is a rarely reported intravitreal worm of Brugia malayi showing that they reaches the vitreous to cause visual problems.If removed on time the post operative prognosis is usually good.
References
- Dissanaike AS, Bandara CD, Padmini HH, Ihalamulla RL, Naotunne TS. (2000). Recovery of a species of Brugia, probably B. ceylonensis, from the conjunctiva of a patient in Sri Lanka. Ann Trop Med Parasitol. 94: 83–6.
- Georgalas, Illias, Paraskevopoulus, Theodore, Rouvas, Alexandros. (2016). Intravitreal Filariasis: The Accidental Traveller. Retina. 36(8): e73-e74.
- Rao NG, Mahapatra SK, Pattnayak S, Pattnaik K. (2008). Intravitreal live adult Brugian filariasis. Indian J Ophthalmol. Jan-Feb; 56(1): 76-8
- Orihel TC, Eberhard ML. (1998). Zoonotic filariasis. Clin Microbiol Rev.11: 366-81.
- Harsha Bhattacharjee, Dipankar Das, Jnanankar Medhi. (2007). Intravitreal gnathostomiasis and review of literatures. Retina 27: 67-73.
- Beaver PC. (1989). Intraocular filariasis: a brief review. Am J Trop Hyg. 40(1):
- Kalogeropoulos CD, Stefaniotou MI, Gorgoli KE, et al. (2014). Ocular dirofilariasis: a case series of 8 patients. Middle East Afr J Ophthalmol. Oct-Dec 21(4): 312-6
- El-Baha SM1, Hemeida TS, Omar HT, El-Fiki SA. Wandering nematodes in the vitreous cavity. Retina Cases Brief Rep. 2009 Winter 3(1): 68-9.
- Anandakannan K, Gupta CP. (1977). Microfilaria malayi in uveitis: case report. Br J Ophthalmol. 61(4): 263-4.
Citation: Gitumoni Sharma and Deepshikha Agrawal. (2019). Rarely reported- Wandering intravitreal worm of Brugia malayi from Central India. Journal of Ophthalmology and Vision Research 1(1).
Copyright: © 2019 Gitumoni Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.