Case Report
Volume 3 Issue 1 - 2021
Ohvira Syndrome: A Case Report
1Specialist in obstetrics and gynaecology, General University Hospital of Elche, Alicante, Spain
2Resident in obstetrics and gynaecology, General University Hospital of Elche, Alicante, Spain
2Resident in obstetrics and gynaecology, General University Hospital of Elche, Alicante, Spain
*Corresponding Author: Begoña Navarro Díaz, Associate specialist at department of Obstetrics and Gynae, General University Hospital, of Elche. Adress: Camí de l’Almàssera 11. 03203 Elche (Alicante). Spain.
Received: August 16, 2021; Published: August 31, 2021
Abstract
OHVIRA syndrome is a rare entity characterized by the association of uterus didelphys with obstructed hemivagina and ipsilateral renal agenesis. The initial diagnosis is, in most cases, incorrect because it’s low incidence and little clinical suspicion. It is usually diagnosed after menarche with the present of dysmenorrhea, pelvic pain and a palpable abdominal mass secondary to hematocolpos. The diagnosis can only be made if the syndrome is suspected. The diagnostic techniques are ultrasound and magnetic resonance imaging, although laparoscopy can play a decisive role in some cases.
Surgical resection of the obstructed vaginal septum is the definitive treatment and prevents possible complications. We present the case of a 14-year-old girl who presented dysmenorrhea, cyclical pelvic pain and a palpable vaginal mass after menarche.
Keywords: OHVIRA syndrome; Hematocolpos; Obstructed hemivagina; Kidney agenesis
Introduction
OHVIRA syndrome (Obstructed Hemivagina and Ipsilateral Renal Anomaly), also known as Herlyn-Werner-Wunderlinch syndrome (HWW), is a rare congenital Müllerian malformation which is represented by the triad of uterine didelphys, obstructed hemivagina and ipsilateral renal agenesis [1]. The eponymous “Herlyn-Werner- Wunderlinch” first used to define this syndrome derives from the report of 4 cases with congenital anomaly of female urogenital tract in 1979. In 2007, the term OHVIRA appeared in the English literature to describe the cases of patients with obstructed hemivagina associated with an ipsilateral renal anomaly [2, 3].
Anomalies in the development of the Müllerian ducts has a variable morphological expression, depending on the time of embryological development in which the anomaly occurs. About the 40% of the cases are associated with renal malformations [4] due to the morphogenic relation of the Müllerian ducts and the mesonephric ducts (Wolff ducts) during the ninth weeks of gestation [5]. OHVIRA syndrome comprises about 2-3% of Müllerian abnormalities [1].
The initial diagnosis is, in most cases, incorrect due to its rare incident and little clinical suspicion. However, its relation with endometriosis, pelvic infection, infertility and obstetric complications create the need of a certain diagnosis [6].
The case of this syndrome in a 14-years-old girl who presented dysmenorra and chronic cyclic pelvic pain due to hematocolpos is described.
Case Report
A 14 years old girl was admitted in Gynae and Obstetrics department at the General University Hospital of Elche with lower abdominal pain of 2 weeks of evolution, associated with nauseas at the moment of menstruation.
Personal history: she weighed 3.525grs after a vaginal delivery with no perinatal complications. At the age of 9 months, after an acute urinary tract infection, she was diagnosed with right renal agenesis. She was followed at the Endocrinology department due to late menarque, which she finally had at the age of 13 years. Since then, she had regularly menstruations until date.
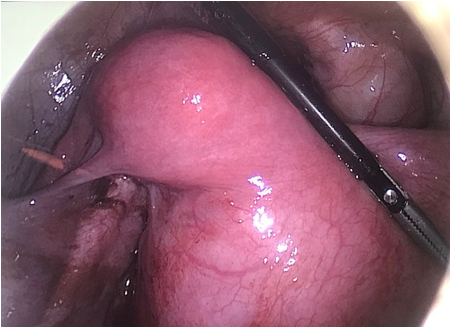
On admission, the patient was hemodynamically stable and afebrile. During the vaginal physical exploration, a mass along the right wall of the vaginal was palpable with an erased cervix lateralized to the left side of the pelvis. A high-resolution transvaginal ultrasound was done, which revealed a mixed ecorefringence mass of 10, 8x6, 5x7, 2cms with elongated appearance in contact on its upper end with two structures that converge, which could correspond with and endometrioma vs. hematometrocolpos. (Figure 1).
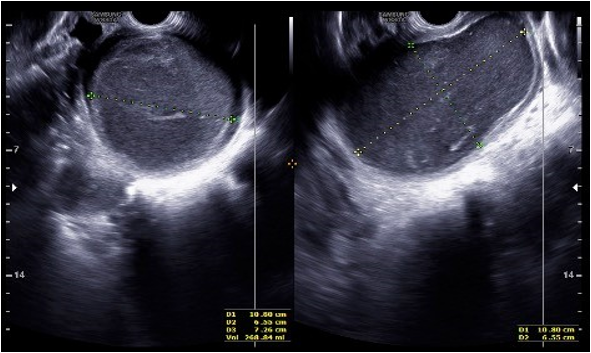
Figure 1: High resolution transvaginal ultrasound image showing a mixed ecorefringence mass which could correspond with and endometrioma vs. hematometrocolpos.
An MRI was performed, which informed of a complex uterine malformation presenting the differential diagnosis between unicornuate uterus with rudimentary non- communicating horn and normal endometrium vs uterus didelphys, associated with hematometrocolpos. Both ovaries appeared to be normal.
In light of the findings, a diagnostic hysteroscopy and laparoscopic surgery were performed. The diagnostic hysteroscopy, at first glance, was no conclusive since it showed a vagina partially bulge by a mass in the right lateral wall and a normal cervix lateralized to the left side of the pelvis which could not be pierced.
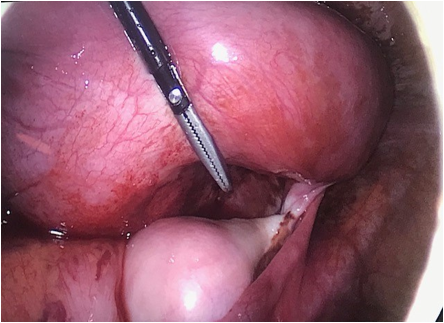
The diagnostic laparoscopy revealed two dilatated hemi-uterus that converged in one canal with a mass in the posterior wall of it. Both ovaries were seen normal.
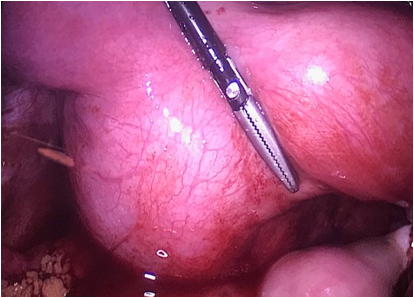
Figure 3: Laparoscopic image showing the posterior part of the mass caused by the hematocolpos in the right obstructed hemivagina, and the 2 dilatated hemiuterus.
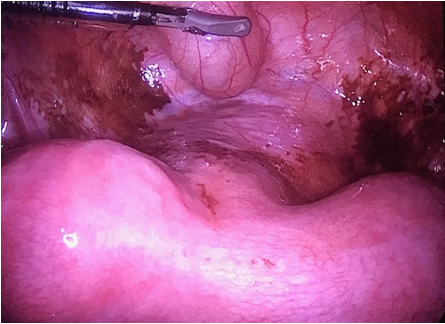
Figure 6: Laparoscopic image showing 2 dilatated hemiuterus, the anterior part of the cervix with normal appearance and 2 normal vaginas. Note the vesical balloon (on top of the hysteroscopic gripper) and hematic remains due to the retrograde menstruation.
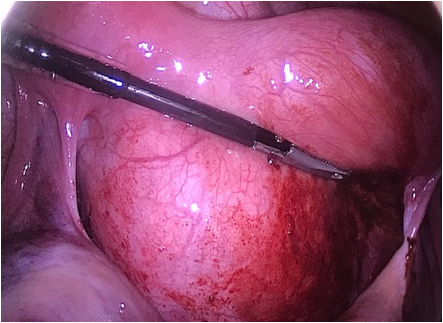
Figure 7: Laparoscopic image corresponding to the mass occasioned by the hematocolpos of the right obstructed hemivagina.
In conclusion with the laparoscopic and hysteroscopic findings, our clinical diagnosis was uterus didelphys associated with hematocolpos due to a right obstructed hemivagina that, by continuity and retrogradely, had dilatated both of the hemi-uterus.
An incision was made over the right vaginal wall where the mass was, obtaining a moderate amount of inspicited blood. In surgical exploration, a patent vaginal cavity and cervix was left in the right side. After the procedure a hysteroscopy was made, showing the presence of two hemi-vaginas, two cervix and two hemi-uterus.
Six months after surgery, an MRI was performed confirming the absence of liquid collections and the presence of a uterus didelphys-bicollis with two hemi-vaginas. (Figures 8a-b, 9a-b-c).
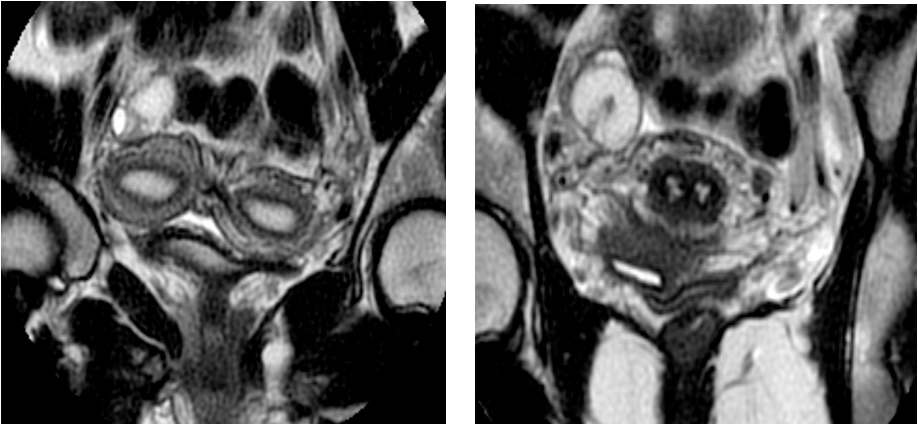
Figure 8a-8b: MRI transverse views 6 months after intervention, demonstrating 2 uterine cavities (8a) and 2 hemivaginas (8b).
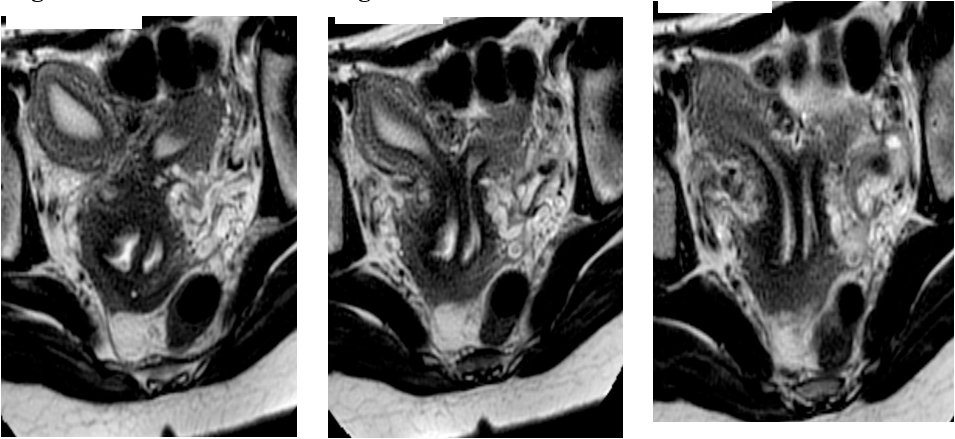
Figure 9a-9b-9c: MRI coronal views 6 months after intervention, demonstrating uterine horns with left and right vagina.
Discussion
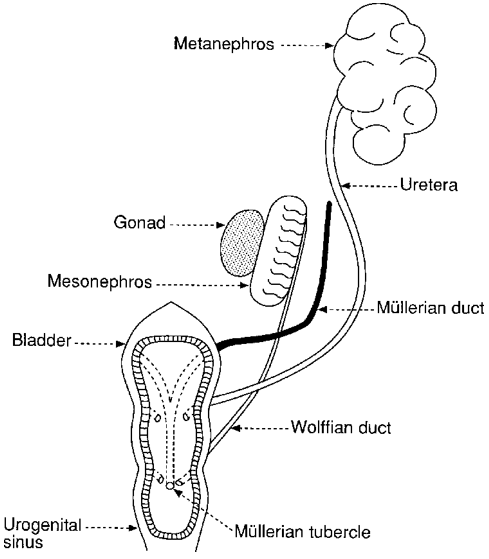
Both male and female embryos initially have two pairs of genital ducts: the mesonephric (or Wolff) ducts and the paramesonephric (or Müllerian) ducts. While the mesonephric ducts derive directly from the mesonephros (primitive kidney), the paramesonephric ducts are formed from a longitudinal invagination of the epithelium of the coelomic cavity.
The Müllerian ducts are located outside the ipsilateral Wolffian ducts, crossing them ventrally in its caudal portion to fuse with each other in the midline, reaching the urogenital sinus (Figure 10). Shortly after the end of the paramesonephric ducts has reached the urogenital sinus, 2 outflows, called synovaginal bulbs, detach from the pelvic portion of the sinus and give rise to the lower 2-thirds of the vagina. The upper third of the vagina derives from the uterine duct, of paramesonephric origin [2, 7].
The Wolffian ducts, in addition to giving rise to the kidneys, facilitate the proper fusion of the Müllerian ducts. In OHVIRA syndrome, it is considered that there is an alteration in the conformation of both paramesonephric and mesonephric ducts, with the Wolffian duct being absent on one side (in 65% of cases the involvement occurs in the right side [1, 4]). On the side where the Wolff ducts are absent, the Müllerian duct is displaced and cannot fuse with the contralateral, resulting in a didelphic uterus. The contralateral Müllerian duct gives rise to a normal hemivagina, while the dislocated one forms a blind cul-de-sac as a blind or obstructed hemivagina. For its part, the vaginal introitus is not affected due to its origin in the urogenital sinus. Renal agenesis is the consequence of the absence of the ipsilateral Wolffian duct due to premature degeneration of the ureteral bud, which is responsible for inducing the development of excretory units [2, 7].
OHVIRA syndrome is an extremely rare condition, reason why in most cases the initial diagnosis is incorrect. It would be advisable to look for an associated Mullerian anomaly in cases of prenatal or neonatal diagnosis of renal agenesis or multicystic dysplasia, but even so, most patients remain asymptomatic until menarche and are usually discovered shortly after it when they debut with dysmenorrhea, pelvic pain, mass palpable or visible on ultrasound due to associated hematocolpos [2] and / or hematometra due to retained bleeding [6], frequently confused with endometrioma or with a complex ovarian cyst [8]. The possible complications associated with this syndrome are a consequence of retrograde menstruation, such as endometriosis, pelvic adhesions, infectious collections [2] and pelvic inflammatory diseases. The diagnosis can be made only if the syndrome is suspected [6]. The technique of choice for diagnosis is ultrasound, but the magnetic resonance imaging can also contribute with the diagnosis and classification of the malformation [2]. Laparoscopy can be of great help for diagnosis in selected cases [6], as the case of our patient.
Adequate recognition of this syndrome and early surgical resection of the vaginal septum determinates the rapid clinical improvement, prevention of complications, and maintenance of fertility [6].
The number of pregnancies in patients with OHVIRA syndrome have been reported as successful, with a ratio of pregnancies up to 87% of cases, 23% of abortion, 15% of preterm deliveries and 62% of full-term pregnancy without complications [6,9].
Conclusion
OHVIRA is a rare syndrome of Mullerian and Wolffian duct abnormalities that requires the clinical suspicion of the clinician to be diagnosed. Most cases are diagnoses after menarque, with the onset of the symptoms. Due to its rarity and the lack of awareness, it is often misdiagnosed or diagnosis is delayed which leads to the appearance of gynecological complications in young women. Thus, with the finding of renal agenesia or multicystic dysplasia, other genital malformations should be suspected and ruled out.
Ultrasound and MRI play a big role in the diagnosis and surgical decision. Laparoscopic surgery can also be useful in selected cases. The final treatment requires an excision of the obstructing vaginal septum.
References
- Paz JJ, Gaitán LF, Acosta MA. (2020). Síndrome de OHVIRA, a propósito de un caso. Univ Salud. 22(3):288-291.
- Guillán C, Sánchez JM, Mández C. (2012). Síndrome OHVIRA (hemivagina obstruída y anomalía renal ipsilateral) asociado a útero didelfo. Prog Obstet Ginecol. 55(6):281-284.
- Smith N, Laufer M. (2007). Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 87:918- 22.
- Santos X, Dietrich J. (2016). Obstructed Hemivagina with Ipsilateral Renal Anomaly. J Pediatr Adolesc Gynecol. 29(1):7-10.
- Mandava A, Prabhakar R, Smitha S. (2012). OHVIRA Syndrome (obstructed hemivagina and ipsilateral renal anomaly) with Uterus Didelphys, an Unusual Presentation. J Pediatr Adolesc Gynecol. 25(2):e23-5.
- Villagómez C, Cordero L, Uscanga MC, Espínola C. (2013). Síndrome OHVIRA (Útero didelfo con hemovagina obstruida y agenesia renal ipsilateral). Un caso inusual de infertilidad. Rev Sanid Milit Mex 67(6):297-300.
- Sadler TW, editor. Langman. Embriología médica. Buenos Aires: Editorial Médica Panamericana SA; 1987.
- Boria F, Lucas J, Álvarez C, Poza J. (2019). Síndrome de Herlyn-Wernwe-Wünderlich y diagnóstico tardío; a propósito de un caso. Rev Peru Ginecol Obstet. 65(3):337-340.
- Candiani GB, Fedele L, Candiani M. (1997). Double uterus, blind hemivagina, and ipsilateral renal agenesis: 3 cases and longterm followup. Obstet Gynecol 90:26-32.
Citation: Begoña Navarro Díaz, Natalia Siverio Colomina and Elena Moreno Pérez. (2021). Ohvira Syndrome: A Case Report. Journal of Gynaecology and Paediatric Care 3(1).
Copyright: © 2021 Begoña Navarro Díaz. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.