Research Article
Volume 1 Issue 1 - 2019
Nutritional Status and their Associated Factors of Under-five year’s Children in Nepal: A Statistical Analysis of Nepal Demographic and Health Survey 2016
1Lecturer of Tribhuvan University, Department of Statistics, Birendra Multiple Campus
2ChitwanSakriya Women’s foundation, Bharatpur, Chitwan, Nepal
3Senior staff Nurse, Chitwan Medical College
2ChitwanSakriya Women’s foundation, Bharatpur, Chitwan, Nepal
3Senior staff Nurse, Chitwan Medical College
*Corresponding Author: Govinda Prasad Dhungana, Lecturer of Tribhuvan University, Department of Statistics, Birendra Multiple Campus, Nepal.
Received: July 11, 2019; Published: July 20, 2019
Abstract
Background: Poor nutrition in early childhood often leads to the majority of deaths and morbidity of children. Most of the developing nations have been affected by poverty and its effect on children, particularly under the age of 5. The aim of this research was therefore to determine the nutritional status of children under 5 years of age and their associated factors.
Method: Quantitative population-based study design was used on data from the 2016 Nepal Demographic and Health Survey. A total of 2135 children under 5 years of age (study populations) were included in this research.
Results: The prevalence of stunting in children under 5 year of age was discovered to be 35.9 % (95% CI: 33.9-37.9), whereas the prevalence of underweight and wasted was found to be 31.5% (95% CI: 29.5-33.5) and 10.1% (95% CI: 8.8-11.4) respectively. In comparison with the male, female children under 5 years of age were more stunted and underweight. On wasted, male children have been slightly high as compared to female child.
The main factor affected by nutrition is province, place of residence, mother's education, wealth index, birth weight, ecological zones, place of delivery and ethnicity.
Conclusions: The prevalence of malnourished is still high in Nepal, which is the issue of public health in developing countries. Various factors are explored about malnutrition, that why government take action must be directed towards short-term nutritional supplements and long-term economic empowerment of disadvantaged groups to reduce child malnutrition. Government focuses in school education on the effects and consequences of malnutrition that boost understanding and help reduce malnutrition in future generations.
Keywords: Nutrition; Stunting; Underweight; Wasting; Nepal
Introduction
Nutrition can be defined as the sum of the complete cycle of providing and receiving nutrients necessary for health and development. It is the organic process whereby an organism assimilates food and utilizes it further to increase and maintain it. Nutrition is the use of food in order to grow, repair and maintain our bodies and to ensure that healthy foods combine the correct amounts of nutrients. A strong health and wellbeing factor is an optimum nutrition for our bodies [1].
The child's health, growth, development and academic achievement are essential to their nutritional status. The most significant challenge facing the current 21st century is the securing of adequate and significant nutrient food [2]. In most developing countries such as Nepal, malnutrition was regarded as a significant public health problem in children and women. Around 45% of deaths are related to under-nutrition among children under the age of 5, usually found in low and middle incomes countries. At the same moment, childhood overweight and obesity levels are increasing in these same nations [3]. Every year 7.6 million children die as a result of preventable malnutrition and its associated causes. Similarly, low birth weight was also seen as the next preventable cause of infant and child mortality due to the intergeneration cycle of malnutrition, particularly in females [4].
In particular, the WHO classifies under nutritional conditions: stunning (acute malnourished), wasted (chronic malnourished) and underweight (acute as well as chronic malnourished). Globally, around 155 million children under the age of 5 suffer from stunting, nearly 52 million children under the age of 5 have been wasted and 17 million have been severely wasted, while 462 million have been underweight [5]. The developmental, economic, social and physical effects of the global malnutrition burden are serious and prolonged for people and families, communities and countries [3].
Malnutrition rates stay flat: stunting declines too slowly while overweight continues to increase. Africa and Asia share the greater burden of all types of malnutrition. While less than half of all under-5 children live in low-middle-income countries, two-thirds of all stunted children and three-quarters of all wasted children live there [5]. According to the Nepal Demographic and Health Survey 2011, stunting was revealed to be 41.0% in Nepal, underweight was reported to be 29.0% and wasting was reported to be 11.0 % [6].
Not only are medical problems, the nutritional problems are multifactorial, with origins in many other sectors, including education, bad environment, bad socio-cultural beliefs and practices such as: less consideration of supplementary feeding for children, late weaning, and poverty [4].
The current prevalence of stunted, underweight and wasted had 36.0%, 27.0% and 10.0% respectively of Nepal [6], but SDG's goal at the end of 2025 will be 12.4%, 10.1% and 4.2% respectively [7]. It has the gap between the objective of SDG and the present nutrition status of children under the age of 5 in Nepal. In addition, nutritional well-being remains a vast resource for achieving many of the sustainable development goals quickly, but it can be a huge barrier to achieving national, economic and social goals of reducing child morbidity and mortality [8]. Therefore, multiple factors lead to malnutrition, so there should be multifaceted approaches in place to tackle it. That’ why it is essential to determine its causative factors before it is possible to implement suitable action. Thus, this research attempts to evaluate nutritional status among children under the age of five and associate predictors.
Materials and Methods
Nepal Demographic and Health Survey 2016 data sets conducted a quantitative population-based study design. The data set download from https://www dhsprogram com/data/dataset_admin. The sampling technique was stratified for two stages in rural areas and stratified for three stages in urban area used, covering all over the nation [6]. Study was completed from 19 June 2016 to 31 January 2017, a total of 2135 under 5 year’ of age children under 5 were taken.
Variables
In the research, the nutritional status was dependent variable. Three variables were used to assess the nutritional status: children's age, height, and weight. All children under 5 years of age were registered anthropometric measurements in WHO Anthro software. WHO Anthro software calculated the deviations of the actual height and weight measurements from the respective age-specific median values in the reference population and converted to Z-scores. The malnourished, according to WHO, is described on the grounds of anthropometric indices as:
In the research, the nutritional status was dependent variable. Three variables were used to assess the nutritional status: children's age, height, and weight. All children under 5 years of age were registered anthropometric measurements in WHO Anthro software. WHO Anthro software calculated the deviations of the actual height and weight measurements from the respective age-specific median values in the reference population and converted to Z-scores. The malnourished, according to WHO, is described on the grounds of anthropometric indices as:
Stunted: Height for age
Wasted: Weight for height
Underweight: Weight for age
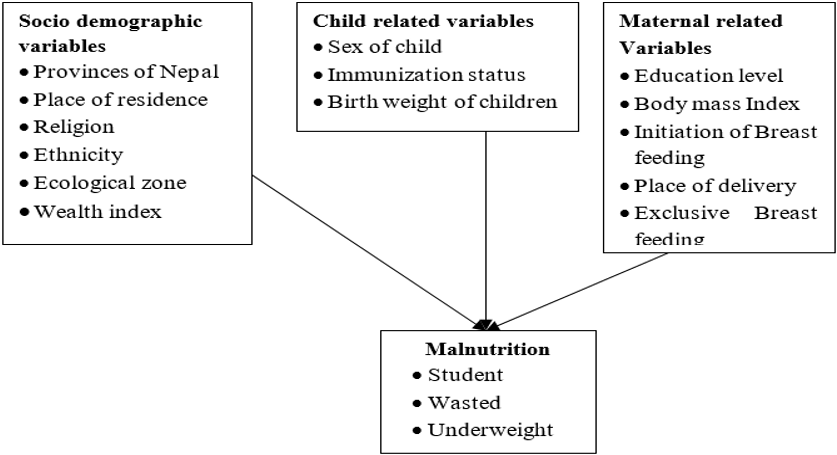
To determine the predictors of under-nutrition among children under 5 years of age were categories in three parts (a) Socio-demographic factors (b) Child-related factors (c) Maternal-related factors shown in Figure 1.
Data analysis
Data were checked, edited and coded before the analysis, then after data was imported into WHO Anthro software to convert Z score. After calculating the Z score, data was analyzed by IBM SPSS version 20 software after exporting data from WHO Anthro. The data were analyzed on the basis of objects, i.e. determining the prevalence of under nutrition (stunted, wasted and underweight) and explored the predictors of malnutrition. To determine the predictors, bi-variate and multivariate were accomplished in inferential statistics. In bivariate, odds ratio and its confidence interval have been calculated for assessing the significance of a relationship between nutrition status (dependent variable) and related factors (independent variables). Only for those variables with p-value < 0.10 in bivariate analysis, multivariate binary logistic regression was performed to examine the net effect of nutritional status on each of independent variables. The statistical significant was consider as p-value < 0. 05, as demonstration in multivariate table. Model adequacy test was done by Negalkerke R2 and Hosmer and Lemeshow test. Further, residual analysis was done through the scatter plot and multicollinearity checked by Variance Inflation Factor, (VIF) < 10 which was acceptable.
Data were checked, edited and coded before the analysis, then after data was imported into WHO Anthro software to convert Z score. After calculating the Z score, data was analyzed by IBM SPSS version 20 software after exporting data from WHO Anthro. The data were analyzed on the basis of objects, i.e. determining the prevalence of under nutrition (stunted, wasted and underweight) and explored the predictors of malnutrition. To determine the predictors, bi-variate and multivariate were accomplished in inferential statistics. In bivariate, odds ratio and its confidence interval have been calculated for assessing the significance of a relationship between nutrition status (dependent variable) and related factors (independent variables). Only for those variables with p-value < 0.10 in bivariate analysis, multivariate binary logistic regression was performed to examine the net effect of nutritional status on each of independent variables. The statistical significant was consider as p-value < 0. 05, as demonstration in multivariate table. Model adequacy test was done by Negalkerke R2 and Hosmer and Lemeshow test. Further, residual analysis was done through the scatter plot and multicollinearity checked by Variance Inflation Factor, (VIF) < 10 which was acceptable.
Results
Background Characteristics
Female children (52.6%) were slightly more compared to male (47.4%). More than one fifth (22.1%) of the children were from province two. Most of the children belong to Hindu religion (87.2%) and Brahmin/Chhetri were more in number as compared to other castes. More than half (55.7%) of the children were from urban area and nearly one fourth (24.1%) were from poorest wealth index category. A total of 463 under five years children (23.1%) were from age group 36 to 47 months. More than two fifth (44.5%) delivered their baby in public health facilities. About 10% of the under five children have low birth weight and more than a half have received complete immunization. Nearly three fifth (57.0%) of the children initiated breastfeeding within one hour of birth.
Female children (52.6%) were slightly more compared to male (47.4%). More than one fifth (22.1%) of the children were from province two. Most of the children belong to Hindu religion (87.2%) and Brahmin/Chhetri were more in number as compared to other castes. More than half (55.7%) of the children were from urban area and nearly one fourth (24.1%) were from poorest wealth index category. A total of 463 under five years children (23.1%) were from age group 36 to 47 months. More than two fifth (44.5%) delivered their baby in public health facilities. About 10% of the under five children have low birth weight and more than a half have received complete immunization. Nearly three fifth (57.0%) of the children initiated breastfeeding within one hour of birth.
Prevalence of under nutrition
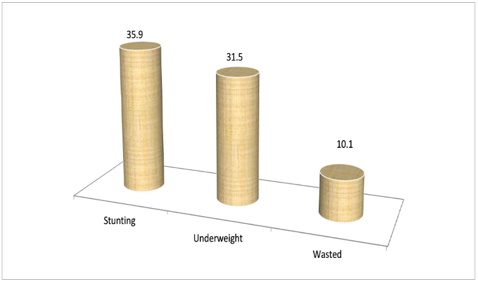
The prevalence of stunting in under 5 years children was found to be 35.9% (95% CI: 33.9-37.9) whereas the prevalence of wasting and underweight in under 5 years children was found to be 10.1% (95% CI: 8.8-11.4) and 31.5% (95% CI: 29.5-33.5) respectively (Figure 2)
The prevalence of stunting in under 5 years children was found to be 35.9% (95% CI: 33.9-37.9) whereas the prevalence of wasting and underweight in under 5 years children was found to be 10.1% (95% CI: 8.8-11.4) and 31.5% (95% CI: 29.5-33.5) respectively (Figure 2)
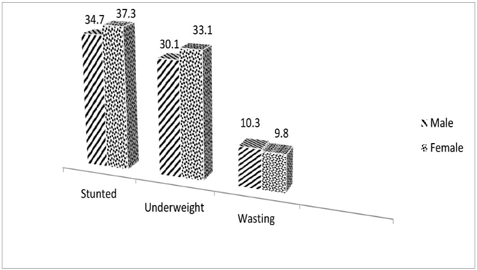
Females of under 5 were found to be more stunted and underweight compared to the male. A total of 37.3% and 33.1% of females were found to be stunted and underweight respectively compared to 34.7% and 30.1% of males. Males were slightly high on wasting (Figure 3).
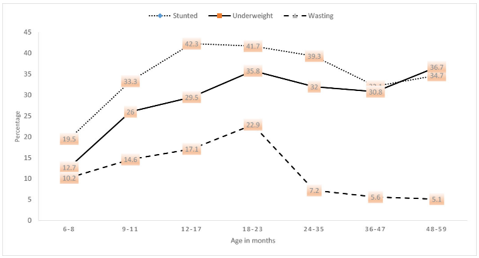
The prevalence of stunting, underweight and wasting were found to be in increasing trend till the age group 18-23 months. The peak of under nutrition was found to be in age group 18-23 months (Figure 4)
Explore the associated factors of stunting by multivariate analysis
Province was found to be significantly associated with stunted. Those U5 children who were from province 6 were 2 times (AOR=2.115, 95% CI= 1.355-3.301) more likely and children from province 1 were 1.6 times (AOR=1.618, 95% CI: 1.015-2.578) to be stunted than those children from province 1. Education level of the mother was also found to be significantly associated with the stunting of the children. Those children from mothers with no education and primary education were 2 times (AOR= 1. 998, 95% CI= 1. 386-2. 880) and 1. 5 times (AOR=1. 510, 95% CI=1. 029-2. 215) more likely to be stunted respectively compared to those children from mother of higher education. Those children from poorer wealth index were 1. 6 times (AOR=1. 599, 95% CI=1. 214-2. 108) more likely to be stunted compared to children from richer wealth index. Those children residing in the Terai region were 1.6 times (AOR=1.639, 95% CI=1.192-2.255) more likely to be stunted compared to those residing in Hilly region. Those children who were born with low weight were 2 times (AOR=2. 007, 95% CI=1. 428-2. 820) more likely to be stunted compared to those children who were born with normal weight. Those children who were given birth in home were 1. 6 times (AOR=1 .626, 95% CI=1. 089-2. 428) more likely to be stunted compared to those who were given birth in private hospital (table 1).
Province was found to be significantly associated with stunted. Those U5 children who were from province 6 were 2 times (AOR=2.115, 95% CI= 1.355-3.301) more likely and children from province 1 were 1.6 times (AOR=1.618, 95% CI: 1.015-2.578) to be stunted than those children from province 1. Education level of the mother was also found to be significantly associated with the stunting of the children. Those children from mothers with no education and primary education were 2 times (AOR= 1. 998, 95% CI= 1. 386-2. 880) and 1. 5 times (AOR=1. 510, 95% CI=1. 029-2. 215) more likely to be stunted respectively compared to those children from mother of higher education. Those children from poorer wealth index were 1. 6 times (AOR=1. 599, 95% CI=1. 214-2. 108) more likely to be stunted compared to children from richer wealth index. Those children residing in the Terai region were 1.6 times (AOR=1.639, 95% CI=1.192-2.255) more likely to be stunted compared to those residing in Hilly region. Those children who were born with low weight were 2 times (AOR=2. 007, 95% CI=1. 428-2. 820) more likely to be stunted compared to those children who were born with normal weight. Those children who were given birth in home were 1. 6 times (AOR=1 .626, 95% CI=1. 089-2. 428) more likely to be stunted compared to those who were given birth in private hospital (table 1).
| Variables | P-value | UOR | Adjusted OR (95% CI) |
| Province of Nepal | |||
| Province 4 | 1 | ||
| Province 1 | 0.043 | 1.934 | 1.618 (1.015-2.578) |
| Province 2 | 0.394 | 2.818 | 1.243 (0.754-2.050) |
| Province 3 | 0.679 | 0.980 | 1.111 (0.674-1.831) |
| Province 5 | 0.363 | 2.020 | 1.238 (0.781-1.962) |
| Province 6 | 0.001 | 2.997 | 2.115 (1.355-3.301) |
| Province 7 | 0.887 | 1.882 | 1.035 (0.644-1.665) |
| Educational level of mother | |||
| Higher | 1 | ||
| No education | <0.001 | 2.833 | 1.998 (1.386-2.880) |
| Primary | 0.035 | 1.967 | 1.510 (1.029-2.215) |
| Secondary | 0.072 | 1.468 | 1.369 (0.972-1.926) |
| Wealth Index | |||
| Richera | 1 | ||
| Poorerb | 0.001 | 1.794 | 1.599(1.214-2.108) |
| Middle | 0.363 | 1.569 | 1.139(0.861-1.506) |
| Ecological zone | |||
| Hill | 1 | ||
| Mountain | 0.099 | 1.741 | 1.382 (0.941-2.030) |
| Terai | 0.002 | 1.532 | 1.639 (1.192-2.255) |
| Birth weight | |||
| Normal | 1 | ||
| Low birth weight | <0.001 | 1.851 | 2.007 (1.428-2.820) |
| Place of delivery | |||
| Private hospitalc | |||
| Home | 0.017 | 2.266 | 1.626 (1.089-2.428) |
| Public hospitald | 0.138 | 1.381 | 1.338 (0.911-1.966) |
| Otherse | 0.111 | 2.064 | 1.578 (0.901-2.763) |
Table 1: Predictors of stunting by multivariate analysis.
1-Reference Category, Cox and snell R square = 0.109, Nagelkerke R Square = 0.150, Hosmer and Lemeshow test =13.239 (p value=0.104), -2log likelihood=2517.141, OR= odds ratio, UOR= Unadjusted odd ratio, CI= Confidence interval, aincludes richer and richest, bincludes poorer and poorest, cprivate hospital/nursing home, private clinic, other private sector, NGO sector, FPAN, maries topes, other NGO facilities, dincludes public sector, government hospital, primary health care center, health post/sub health post, primary health care outreach clinic, other public sector , eincludes India and others
Explore the associated factors of wasting by multivariate analysis
Those children from province 3 were 93.8% (AOR=0.062, 95% CI=0.008-0.478) and those from province 4 were 88.1% (AOR= 0.119, 95% CI=0.027-0.526) to be protect from malnourished (wasted) as compare to those children who live in province 1. Likewise, those children from Tarai were around 4 time (AOR=3.762, 95% CI=1.366-10.365) more likely to be wasted than those children who were live in Mountain. Other religion (Muslim, Terai and other) religion were around 2 time (AOR=1.917, 95% CI=1.133-3.242) more likely to be wasted as compare to Hindu. Those children who had low birth weight were 2.63 times (AOR=2.626, 95% CI=1.556-4.432) more likely to be wasted as compared to those children who were normal (table 2).
Those children from province 3 were 93.8% (AOR=0.062, 95% CI=0.008-0.478) and those from province 4 were 88.1% (AOR= 0.119, 95% CI=0.027-0.526) to be protect from malnourished (wasted) as compare to those children who live in province 1. Likewise, those children from Tarai were around 4 time (AOR=3.762, 95% CI=1.366-10.365) more likely to be wasted than those children who were live in Mountain. Other religion (Muslim, Terai and other) religion were around 2 time (AOR=1.917, 95% CI=1.133-3.242) more likely to be wasted as compare to Hindu. Those children who had low birth weight were 2.63 times (AOR=2.626, 95% CI=1.556-4.432) more likely to be wasted as compared to those children who were normal (table 2).
| Variables | P Value | UOR | Adjusted OR (95% C.I) |
| Province | |||
| Province-1 | 1 | ||
| Province -2 | 0.793 | 1.199 | 0.926 (0.521-1.66) |
| Province-3 | 0.008 | 0.043 | 0.062 (0.008-0.478) |
| Province-4 | 0.005 | 0.089 | 0.119 (0.027-0.526) |
| Province-5 | 0.118 | 0.706 | 0.627 (0.349-1.127) |
| Province-6 | 0.898 | 0.644 | 0.953 (0.456-1.989) |
| Province-7 | 0.983 | 0.734 | 0.993 (0.532-1.856) |
| Ecological zone | |||
| Mountain | 1 | ||
| Hill | 0.084 | 1.625 | 2.369 (0.889-6.454) |
| Terai | 0.010 | 3.992 | 3.762 (1.366-10.365) |
| Religion | |||
| Hindu | 1 | ||
| Buddhist | 0.477 | 0.342 | 0.580 (0.129-2.600) |
| Othersf | 0.015 | 2.422 | 1.917 (1.133-3.242) |
| Birth weight | |||
| Normal | 1 | ||
| Low birth weight | <0.001 | 2.616 | 2.626 (1.556-4.432) |
Table 2: Predictors of wasted by multivariate analysis.
1-Reference Category, Cox and snell R square=0.051, Nagelkerke R Square=0.112, Hosmer and Lemeshow test=8.146 (p value=0.419), -2log likelihood=958.42, OR= odds ratio, UOR= Unadjusted odd ratio, CI= Confidence intervals,
fincludes Muslim, Terai and other religion
fincludes Muslim, Terai and other religion
Explore the associated factors of Underweight by multivariate analysis
With the new federal state, province was found to be significantly associated with underweight. Those U5 Children who were from province 6 were 2 times (AOR=2.076, 95% CI=1.356-3.176) more likely to be underweight than those children from province 1. Regarding the place of residence, rural children were 1.2 times (AOR=1.286, 95% CI= 1.042-1.588) more likely to be underweight compared to children residing in urban areas. Likewise, education level of the mother was also found to be significantly associated with the underweight. Those children from mothers with no education and primary education were 2 times (AOR= 2.016, 95% CI= 1.371-2.964) and 1.5 times (AOR= 1.3535, 95% CI=1.026-2.294) more likely to be underweight respectively compared to those children from mother of higher education. Regarding wealth index, those children from poorer wealth index were nearly 2 times (AOR= 1.757, 95% CI=1.321-2.336) more likely to be underweight compared to children from richer wealth index. Birth weight was also found to be strong predictor for underweight. Those children who were born with low weight were nearly 2 times (AOR=1.976, 95% CI= 1.397-2.796) more likely to be underweight compared to those children who were born with normal weight. From the ethnicity, those children from Brahmin/Chhetri were 1.3 times (AOR=1.383, 95% CI=1.027-1.864) and children from other castes such as Muslim, other Terai caste were almost 2 times (AOR=1.995, 95% CI= 1.356-2.936) more likely to be underweight respectively compared to Janajaties (table 3).
With the new federal state, province was found to be significantly associated with underweight. Those U5 Children who were from province 6 were 2 times (AOR=2.076, 95% CI=1.356-3.176) more likely to be underweight than those children from province 1. Regarding the place of residence, rural children were 1.2 times (AOR=1.286, 95% CI= 1.042-1.588) more likely to be underweight compared to children residing in urban areas. Likewise, education level of the mother was also found to be significantly associated with the underweight. Those children from mothers with no education and primary education were 2 times (AOR= 2.016, 95% CI= 1.371-2.964) and 1.5 times (AOR= 1.3535, 95% CI=1.026-2.294) more likely to be underweight respectively compared to those children from mother of higher education. Regarding wealth index, those children from poorer wealth index were nearly 2 times (AOR= 1.757, 95% CI=1.321-2.336) more likely to be underweight compared to children from richer wealth index. Birth weight was also found to be strong predictor for underweight. Those children who were born with low weight were nearly 2 times (AOR=1.976, 95% CI= 1.397-2.796) more likely to be underweight compared to those children who were born with normal weight. From the ethnicity, those children from Brahmin/Chhetri were 1.3 times (AOR=1.383, 95% CI=1.027-1.864) and children from other castes such as Muslim, other Terai caste were almost 2 times (AOR=1.995, 95% CI= 1.356-2.936) more likely to be underweight respectively compared to Janajaties (table 3).
| Variables | P Value | UOR | Adjusted OR (95% CI) |
| Province of Nepal | |||
| Province1 | 1 | ||
| Province 2 | 0.062 | 1.345 | 0.673 (0.444-1.020) |
| Province 3 | 0.221 | 1.051 | 1.338 (0.840-2.133) |
| Province 4 | 0.110 | 1.101 | 1.458 (0.918-2.317) |
| Province 5 | 0.523 | 1.456 | 1.132 (0.773-1.660) |
| Province 6 | 0.001 | 2.679 | 2.076 (1.356-3.176) |
| Province 7 | 0.257 | 1.152 | 0.781 (0.510-1.197) |
| Place of residence | |||
| Urban | 1 | ||
| Rural | 0.019 | 1.693 | 1.286 (1.042-1.588) |
| Educational level of mother | |||
| Higher | 1 | ||
| No education | <0.001 | 2.939 | 2.016 (1.371-2.964) |
| Primary | 0.037 | 2.083 | 1.535 (1.026-2.294) |
| Secondary | 0.146 | 1.454 | 1.310 (0.910-1.885) |
| Wealth Index | |||
| Richera | 1 | ||
| Poorerb | <0.001 | 2.433 | 1.757 (1.321-2.336) |
| Middle | 0.491 | 1.419 | 1.111 (0.824-1.497) |
| Birth weight of baby | |||
| Normal | 1 | ||
| Low birth weight | <0.001 | 1.575 | 1.976 (1.397-2.796) |
| Ethnicity | |||
| Janajatig | 1 | ||
| Brahman/Chhetrih | 0.033 | 1.487 | 1.383 (1.027-1.864) |
| Daliti | 0.159 | 1.686 | 1.269 (0.911-1.767) |
| Othersj | <0.001 | 1.717 | 1.995 (1.356-2.936) |
Table 3: Predictors of underweight by multivariate analysis.
1-Reference Category, Cox and snell R square=0.104, Nagelkerke R Square=0.147, Hosmer and Lemeshow test=8.549 (p value=0.382), -2log likelihood=2396.137, OR= odds ratio, UOR= Unadjusted odd ratio, CI= Confidence interval,
aincludes richer and richest, bincludes poorer and poorest, gincludes hill janajaties, terai janajaties, Newar, hincludes hill Brahmin, hill chhtetri, terai Brahmin/chhetri, iincludes hill dalit and terai dalit, jincludes others,muslim and terai caste
aincludes richer and richest, bincludes poorer and poorest, gincludes hill janajaties, terai janajaties, Newar, hincludes hill Brahmin, hill chhtetri, terai Brahmin/chhetri, iincludes hill dalit and terai dalit, jincludes others,muslim and terai caste
Discussion
Malnutrition has been a major public health concern in developing countries like Nepal. Many developing countries are still living below the poverty line and children of under-five have been more prone to malnutrition like Nepal [9]. This study showed that 35.9% were stunted, 31.5% were underweight and 10.1% were wasted. A meta-analysis conducted in Ethiopia in 2017 revealed that stunting, underweight and wasting was 42.0%, 33.0% and 15.0% respectively [2]. The analysis of the study conducted in Oromia region by Mengistu., et al. revealed that, 47.6%, 30.9% and 16.7% of children were stunted, underweight and wasted, respectively [10]. This might be difference due to study period, study area, economic condition of different countries and their socio economic development. This shows that the condition of under nutrition was slightly more as compared to Nepal. This reason might be that, Ethiopia being an African country and as data reveals that African countries are more affected in terms of nutritional status. A study of nutritional status and associated factors of under-five years children in Nepal conducted by Dhungana GP in 2018 revealed that the prevalence of stunting was 51.9%, underweight was 23.3% and that of wasting was 11.2% (1). The present study had low under nutrition as compare to this study because decreasing trend of under nutrition all over the country [6]. Parents are more aware about the under nutrition and its consequences of under 5 years children. A study conducted in Siraha district in 2016 revealed that the prevalence of stunting, underweight and wasting was 47%, 36% and 21% respectively which is quite higher that the present study [11]. One of the reason for it might be the difference in the sample size and study area of the study conducted in Siraha was just a representative of Musahar children however the present study is the representative of all over the country.
Province, place of residence, educational level of mother, wealth index, birth weight, ecological zone, place of delivery and ethnicity were significantly associated factors of under nutrition specially stunting, wasting and underweight. These all factors are almost similar to the factor of these studies [1, 3, 4, 6, 8 and 12].
Province place of residence and ecological region was found to be strong predictor of under nutrition which was consistent finding with [1, 3, 6, 8, 12 and 13] because majority of provinces lies in rural area. Majority of residence area of Nepal located in rural areas. The reason for this might be that the people in rural areas still have the problem of accessibility in terms of nutritious food and also health services.
Education of mother is one of the most important resources that enable women to provide appropriate care for their children. Education of women is believed to exert an impact on health and nutritional status of children since it provides the mother with the necessary skills for child care, increase awareness of nutritional needs and preference of modern health facilities as well as change of traditional beliefs about diseases causation, and use of contraceptives for birth spacing. In this study result, children of mothers who can’t read and write showed higher prevalence of stunting and underweight. Educational status was found to be significantly associated with under nutrition with [1, 6, 8 and 13]. However the educational status of mother was not found to be associated with the study conducted in Bara district of Nepal [14] and also educational level was not found to be significantly associated with stunting, underweight and wasting in the study conducted in Pakistan [15].
Wealth index was significantly associated with underweight and stunting of the under five children. Similar finding was revealed in the study conducted in Statistical Analysis on Nutritional Status in 2017 where wealth index was found to be associated with stunting and underweight [12] and is also consistent with other studies [1,6,9,14,16 and 17]. Children belonging to the low-income group were at a higher risk of being wasted, underweight and stunted than children of better income families. Although the economic differentials seem to be silent in rural society it appears to be an important predictor of childhood nutritional status. Low income levels of developing nation limits the kinds and the amounts of food available for consumption. Low income also increases the likelihood of infection through such mechanisms as inadequate personal and environmental hygiene.
Low birth weight was found to be strong predictor of the nutritional status in this study which was similar to the findings of various studies [1, 6 and 12]. Those children with low birth weight were more prone to be undernourished. Those children with between LBW may have increased vulnerability to infections, such as, diarrheal and lower respiratory infections and the increased risk of complications including sleep apnea, jaundice, anemia, chronic lung disorders, fatigue and loss of appetite compared to children with normal birth weights which may lead to under-nutrition. Low birth weight is caused by poor maternal nutrition during conception or pregnancy. Studies show that interventions such as micronutrient supplementation among pregnant women helps in reducing the risk of low birth weight [6].
Place of delivery was found to be associated with stunting which is consistent with the study conducted in Lamjung, Tanahun and Gorkha district [8]. Differences in lifestyle, nutritional status of pregnant women prior to delivery, and other covert or overt morbid conditions may have accounted for the observed variation.
Conclusion
In this study the prevalence of nutritional status of children under 5 years of age is identify. The research results show that the prevalence of stunted, wasted, and underweight in our country is high. Province, place of residence, mother education level, wealth indices, birth weight, ecological region, place of delivery and ethnicity are predictors of malnutrition.
Action needs to target short-term dietary supplements and long-term economic empowerment in poor communities to help reduce child malnutrition in developing countries such as Nepal. Government focuses in school education on the effects and consequences of malnutrition that boost understanding and help reduce malnutrition in future generations.
Ethical Statement
Ethics approval The 2016 Nepal Demographic Health Survey (NDHS) survey was approved by the Nepal Health Research Council.
Ethics approval The 2016 Nepal Demographic Health Survey (NDHS) survey was approved by the Nepal Health Research Council.
Limitations
This study was carried out through the use of secondary data
This study was carried out through the use of secondary data
Transparency Declaration
The lead author affirms that this manuscript is an honest, accurate and transparent account of the study being reported. The lead author affirms that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
The lead author affirms that this manuscript is an honest, accurate and transparent account of the study being reported. The lead author affirms that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
References
- Dhungana GP. (2018). Nutritional Status and its Associated Factors of under Five Years Children of Nepal: Multi-disciplinary peer-reviewed. journal vibek 34 (11): 136-147
- Abdulahi, A , Shab-Bidar, S , Rezaei, S and Djafarian, K , (2017). Nutritional status of under five children in Ethiopia: a systematic review and meta-analysis. Ethiopian journal of health sciences 27(2): 175-188
- World Health Organization (WHO), key facts, 6 February 2018, Retriveed from
- Bhandari, TR and Chhetri M. (2013). Nutritional status of under five year children and factors associated in Kapilvastu District, Nepal. J Nutr Health Food Sci, 1(1): 1-6
- Hayashi, C , Krasevec, J , Kumapley, R , Mehra, V , de Onis, M , Borghi, E , Blössner, M , Urrutia, M F , Prydz, E B and Serajuddin, U. (2017). Levels and trends in child malnutrition UNICEF/WHO/World Bank Group joint child malnutrition estimates: key findings of the 2017 edition
- Ministry of Health, Nepal; New ERA; and ICF 2017 Nepal Demographic and Health Survey 2016 Kathmandu, Nepal: Ministry of Health, Nepal
- National Planning Commission. Sustainable Development Goals 2016–2030: National (Preliminary) Report. Kathmandu: National Planning Commission. (2015)
- Dhungana, G P. (2017). Nutritional Status and the Associated Factors in Under Five Years Children of Lamjung, Gorkha and Tanahun Districts of Nepal. Nepalese Journal of Statistics 1: 15-18
- Smith LC, Haddad LJ. (2000). Explaining child malnutrition in developing countries: A cross-country analysis. Intl Food Policy Res Inst
- Mengistu K, Alemu K, Destaw B. (2013). Prevalence of malnutrition and associated factors among children aged 6-59 months at Hidabu Abote District, North Shewa, Oromia Regional State. J nutr disorders ther 1: 1-15
- Shah, S K , Shetty, S K , Shingh, D R , Mathias, J , Upadhyay, A and Pandit, R. (2016). Prevalence of Undernutrition among Musahar Children Aged Between 12 To 59 Months in Urban Siraha District, Nepal. MOJ Public Health, 4(5): 00093
- Upadhyay, H P and Bhusal, M K. (2017). Statistical Analysis on Nutritional Status and its Associated Factors of Under Five Years Children in Nepal. Advanced Journal Of Graduate Research, 2(1): 12-24
- Ruwali, D. (2011). Nutritional status of children under five years of age and factors associated in Padampur VDC, Chitwan Health Prospect, 10: 14-18
- Pravana, N K , Piryani, S , Chaurasiya, S P , Kawan, R , Thapa, R K and Shrestha, S. (2017). Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case–control study. BMJ open 7(8): e017084
- Khan, G N , Turab, A , Khan, M I , Rizvi, A , Shaheen, F , Ullah, A , Hussain, A , Hussain, I , Ahmed, I , Yaqoob, M and Ariff, S. (2016). Prevalence and associated factors of malnutrition among children under-five years in Sindh, Pakistan: a cross-sectional study BMC nutrition, 2(1): 69
- García Cruz, L , Gonzalez Azpeitia, G , Reyes Suarez, D , Santana Rodríguez, A , Loro Ferrer, J and Serra-Majem, L. (2017). Factors associated with stunting among children aged 0 to 59 months from the central region of Mozambique. Nutrients, 9(5): 491
- Mgongo, M, Chotta, N, Hashim, T, Uriyo, J, Damian, D, Stray-Pedersen, B, Msuya, S, Wandel, M and Vangen, S. (2017). Underweight, stunting and wasting among children in Kilimanjaro Region, Tanzania; a population-based cross-sectional study. International journal of environmental research and public health, 14(5): 509.
Citation: Govinda Prasad Dhungana, Sujan Neupane and Manisha Sapkota. (2019). Nutritional Status and their Associated Factors of Under-five year’s Children in Nepal: A Statistical Analysis of Nepal Demographic and Health Survey 2016. Archives of Nutrition and Public Health 1(1).
Copyright: © 2019 Govinda Prasad Dhungana. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.