Research Article
Volume 1 Issue 1 - 2019
Nasal Superior Versus Nasal Inferior Implantation of the XEN45 Gel Stent – One Year Results
1Department of Ophthalmology, Bürgerhospital und Clementine Kinderhospital gemeinnützige GmbH Frankfurt/Main, Germany
2International Vision Correction Research Center (IVCRC), University of Heidelberg, Germany
3Department of Ophthalmology, Ruprecht-Karls-University Heidelberg, Germany
2International Vision Correction Research Center (IVCRC), University of Heidelberg, Germany
3Department of Ophthalmology, Ruprecht-Karls-University Heidelberg, Germany
*Corresponding Author: Fritz H. Hengerer MD, PhD, Bürgerhospital und Clementine Kinderhospital gemeinnützige GmbH Nibelungenallee 37-41, 60318 Frankfurt am Main, Germany.
Received: March 15, 2019; Published: March 27, 2019
Abstract
Purpose: To assess effectiveness of the XEN45 gel stent after nasal superior implantation compared to nasal inferior implantation.
Methods: Retrospektive analysis of 152 eyes with XEN45 gel stent implantation in the nasal superior quadrant (Group A, n=56) or in the nasal inferior quadrant (Group B, n=96).
Results: Mean IOP decreased from 33.6± 8.8 mmHg preoperatively to 14.6± 3.2 mmHg at Month 12 in Group A (p < 0.05) and from 32.6± 10.1 mmHg to 14.1± 4.3 mmHg in Group B (p < 0.05). Medication usage reduced from 3.2± 0.9 medications at baseline to 0.3± 0.7 medications at Month 12 in Group A (p < 0.05) and from 3.1± 1.0 to 0.3± 0.7 in Group B (p < 0.05). At Month 3, a significantly lower mean IOP (p=0.023; Mann-Whitney-U-test) and medication usage (p=0.021; Welch`s t-test) were observed in Group A. At all other visits no significant differences were observed (p>0.05). Needling was required in 45% of eyes in Group A and in 27% of Group B (p=0.031; Fisher`s exact test). A second XEN45 gel stent was implanted in 4 eyes of Group A and 7 eyes of Group B. Hypotony (IOP ≤ 6 mmHg) was observed in 3 eyes of Group A and 4 eyes of Group B. All cases resolved spontanously.
Conclusion: Overall, the 1-year results of our retrospective analysis show that implantation of the XEN45 gel stents in the nasally inferior quadrant is as effective as implantation in the superior nasal quadrant and results in significantly reduced IOP and medication usage in glaucoma patients.
Keywords: Glaucoma; XEN45 gel implant; Minimally invasive glaucoma surgery; Implantation site
Introduction
Glaucoma is one of the main causes of blindness, affecting more than 64 million people worldwide.[1] Reduction oft he intraocular pressure (IOP) is the only recognized treatment strategy to prevent further damage to the optic nerve and stop or at least slow the progression of the disease.[2] Therapy options include hypotensive medication, laser procedures and glaucoma drainage surgery.[3,4] Despite the proven efficacy and safety of hypotensive drugs, local and systemic side effects as well as complex treatment regimens can adversely affect adherence and thus limit their efficacy.[5,6] In patients whose IOP is not sufficiently controllable with two medications, surgical options may be taken into account.[4] Trabeculectomy, still the gold standard of surgical glaucoma treatment, demonstrates excellent efficacy but requires a strict postoperative follow-up and has a less than ideal risk profile.[7] Several minimally invasive glaucoma surgery (MIGS) devices which can be implanted ab interno have been developed with the aim to offer a safer, less invasive means of reducing IOP than traditional surgery.[8] Of these, the XEN45 gel implant (XEN45) (Allergan, Dublin, Ireland) creates a permanent drainage path from the anterior chamber into the subconjunctival space, thus bypassing the natural drainage pathways often obstructed in glaucoma patients.[9-11] It consists of hydrophilic gelatine glutaraldehyde, has good biocompatibility and tolerability and is not degradable.[10, 12] The dimensions of the tube (6 mm length; 45 µm inner diameter) were chosen in accordance with Hagen Pouiselle's law to maximize long-term drainage of aqueous humor while minimizing the risk of hypotension.[10, 12-14] Clinical studies have shown that the XEN45 leads to an effective IOP and drug reduction and is associated with a good safety profile.[15-22]
The XEN45 gel stent is commonly implanted in the superonasal quadrant in order to spare the superior area which is usually chosen for trabeculectomy. Even if this approach is usually successful, in some cases the filtering bleb may extend into the superior region possibly leading to changes in the conjunctiva that might impede future trabeculectomy. An implantation of the XEN45 gel stent in the nasally inferior quadrant might therefore be advantageous for several reasons. First of all, the entire superior area would remain completely untouched, thus facilitating future trabeculectomies. Second, the inferior quadrant is more easily accessible during surgery, especially in high cheekbones, which in some cases can impede access with the injector to the superior quadrant. Finally, implantation in the inferior quadrant is conveniently possible without adapting the typical set-up of most operating room with the surgeon sitting at 12 o'clock. However, to the best of out knowledge, no comparative analysis has yet been published clarifying whether the location of the implant affects the effectiveness of the XEN45 gel stent.
The aim of this retrospective study was to evaluate the IOP lowering and medication reduction effect after nasal superior implantation of the XEN45 gel stent implant compared to a nasal inferior implantation. Our hypothesis was that nasal inferior implantation of the XEN45 gel stent is non-inferior to nasal superior implantation in terms of sucess rate, IOP decrease and medication reduction.
Methods
This is a retrospective analysis of consecutive glaucoma patients who received a XEN45 gel implant between March 2014 and June 2015 at the Department of Ophthalmology, Goethe-University, Frankfurt, Germany. The data documentation and retrospective analysis was approved by the local Ethics Committee and adhered to the tenets of the Declaration of Helsinki.
Patients and assessments
Medical records of 152 glaucoma patients with available 12 months follow-up data were included in this analysis. Patients had suffered from an inadequately controlled IOP and had been referred to our Department with a request for surgical glaucoma therapy. In case of a healthy, free and mobile conjunctiva in the target quadrant and lack of active inflammation, patients were considered eligible for XEN45 gel stent implantation. Patients with angle-closure glaucoma, active neovascular glaucoma, conjunctival scarring, or other conjunctival pathologies in the target quadrant, pregnancy, age < 18 years, condition after pars plana vitrectomy, flat anterior chamber and narrow chamber angle were not considered eligible. Prior to XEN45 implantation a complete ophthalmic examination including gonioscopy had been performed. At day 1, week 1, and months 1, 3, 6, and 12 postoperative examinations were performed. At each visit, slit-lamp examination, gonioscopy, and IOP assessment by Goldmann applanation tonometry were carried out. Moreover, the number of medications, needling, second filtrating surgery and adverse events were documented.
Medical records of 152 glaucoma patients with available 12 months follow-up data were included in this analysis. Patients had suffered from an inadequately controlled IOP and had been referred to our Department with a request for surgical glaucoma therapy. In case of a healthy, free and mobile conjunctiva in the target quadrant and lack of active inflammation, patients were considered eligible for XEN45 gel stent implantation. Patients with angle-closure glaucoma, active neovascular glaucoma, conjunctival scarring, or other conjunctival pathologies in the target quadrant, pregnancy, age < 18 years, condition after pars plana vitrectomy, flat anterior chamber and narrow chamber angle were not considered eligible. Prior to XEN45 implantation a complete ophthalmic examination including gonioscopy had been performed. At day 1, week 1, and months 1, 3, 6, and 12 postoperative examinations were performed. At each visit, slit-lamp examination, gonioscopy, and IOP assessment by Goldmann applanation tonometry were carried out. Moreover, the number of medications, needling, second filtrating surgery and adverse events were documented.
Surgical procedure
All implantations were performed as a stand-alone procedure by one single surgeon (FHH) following a standardized implantation technique which has been described in detail in a recent publication.[20] In brief, the XEN45 was implanted under peribulbar anesthesia using an ab interno approach. At first, a volume of 0.1 ml of MMC solution (0.01% mitomycin C, a total dose of 10µg) was injected subconjunctivally in the nasal superior quadrant to prevent further scarring of the conjunctiva. After the anterior chamber was filled with a medium grade viscoelastic device, the preloaded injector needle was then inserted through a 1.2 mm corneal paracentesis incision opposite the site of desired implantation. The needle was then directed across the anterior chamber and the injector tip was used to penetrate through the chamber angle above trabecular meshwork and the sclera at least 3 mm in length in order to place the implant properly. After careful removal of viscoelastic and hydration of paracenteses the eye was covered with a patch.
All implantations were performed as a stand-alone procedure by one single surgeon (FHH) following a standardized implantation technique which has been described in detail in a recent publication.[20] In brief, the XEN45 was implanted under peribulbar anesthesia using an ab interno approach. At first, a volume of 0.1 ml of MMC solution (0.01% mitomycin C, a total dose of 10µg) was injected subconjunctivally in the nasal superior quadrant to prevent further scarring of the conjunctiva. After the anterior chamber was filled with a medium grade viscoelastic device, the preloaded injector needle was then inserted through a 1.2 mm corneal paracentesis incision opposite the site of desired implantation. The needle was then directed across the anterior chamber and the injector tip was used to penetrate through the chamber angle above trabecular meshwork and the sclera at least 3 mm in length in order to place the implant properly. After careful removal of viscoelastic and hydration of paracenteses the eye was covered with a patch.
Postoperatively, topical antibiotics were given 4 times daily for 10 days in combination with steroids 6 times daily and tapered out over 6 weeks. Anti-glaucoma medication was given until surgery and was completely stopped after the implantation of the gel implant; there was no wash-out phase. At every visit, IOP was assessed and if IOP was elevated, additional anti-glaucoma medication or secondary intervention were given at the discretion of the surgeon. In case of conjunctival scarring and bleb failure due to Tenon’s cyst formation, a needling procedure was performed under microscopic view in the operating room. The needling technique has recently been described in detail.[20] The administration of additional drugs during the needling was considered on a case-by-case basis. Only in cases of pronounced fibrosis (approx. 10% of cases) 10 µg mitomycin C was injected during needling, while in eyes with cystic fibroses no additional drugs were used.
Statistical methods
Data was statistically analysed using SPSS Statistics Version 24.0. (IBM 2016).[23] For the comparative analysis, two groups according to the implantation site (Group A: superior nasal; Group B: inferior nasal) were defined. Effectiveness variables were mean IOP, mean number of hypotensive medication and needling rate at each follow-up visit as well the proportion of patients achieving a target IOP of ≤ 18 mmHg, ≤ 15 mmHg, and ≤ 13 mmHg at 12 months. Moreover success rates after one year were calculated according to the following definitions: „qualified success“ was defined as IOP reduction of at least 20% and an IOP value below 18 mmHg with and without medication. Complete success” was defined as an IOP reduction of at least 20% and an IOP value below 18 mmHg without medication. Safety outcomes included hypotony rate (IOP ≤ 6 mmHg) as well as intra- and postoperative complications. Data were presented as mean and standard deviation, unless otherwise indicated. Baseline IOP was the IOP measured at the preoperative visit on medications and the IOP measured at each visit was then used to calculate the change from baseline. In order to compare pre- and postoperative values, the t-test was used. Also, the Wilcoxon sign rank test was used for determining statistical significance within a group (p < 0.05 considered statistically significant). For determining statistical significance between both groups, t-test for two independent samples (p < 0.05 considered statistically significant). Chi-square tests were performed in all other cases (p < 0.05 considered statistically significant).
Data was statistically analysed using SPSS Statistics Version 24.0. (IBM 2016).[23] For the comparative analysis, two groups according to the implantation site (Group A: superior nasal; Group B: inferior nasal) were defined. Effectiveness variables were mean IOP, mean number of hypotensive medication and needling rate at each follow-up visit as well the proportion of patients achieving a target IOP of ≤ 18 mmHg, ≤ 15 mmHg, and ≤ 13 mmHg at 12 months. Moreover success rates after one year were calculated according to the following definitions: „qualified success“ was defined as IOP reduction of at least 20% and an IOP value below 18 mmHg with and without medication. Complete success” was defined as an IOP reduction of at least 20% and an IOP value below 18 mmHg without medication. Safety outcomes included hypotony rate (IOP ≤ 6 mmHg) as well as intra- and postoperative complications. Data were presented as mean and standard deviation, unless otherwise indicated. Baseline IOP was the IOP measured at the preoperative visit on medications and the IOP measured at each visit was then used to calculate the change from baseline. In order to compare pre- and postoperative values, the t-test was used. Also, the Wilcoxon sign rank test was used for determining statistical significance within a group (p < 0.05 considered statistically significant). For determining statistical significance between both groups, t-test for two independent samples (p < 0.05 considered statistically significant). Chi-square tests were performed in all other cases (p < 0.05 considered statistically significant).
Results
Overall, medical records of 152 glaucoma eyes with a mean age of 68.7 ± 14.5 years were analysed. The XEN45 gel stent was implanted in the nasal superior quadrant in 56 eyes (Group A) and in the nasal inferior quadrant in 96 eyes (Group B). Demographics and baseline ocular parameters of both groups are presented in Table 1, with no statistically significant differences being observed between both groups.
| Group A (Nasal superior) (n = 56) | Group B (Nasal inferior) (n = 96) | P-value§ | |
| Age (years), mean ± SD (range) |
67.8 ± 15.6 | 69.2 ± 13.9 | p = 0.76 |
| (28-91) | (28 - 91) | ||
| Gender, n (%)* Male |
27 (48.1) | 34 (35.1) | p = 0.16 |
| Female | 29 (51.9) | 62 (64.9) | |
| Operated Eye, n (%)* OD (right eye) |
27 (48.1) | 48 (50.0) | p = 0.87 |
| OS (left eye) | 29 (51.9) | 48 (50.0) | |
| Cup to Disc Ratio, mean ± SD (range) |
0.8 ±0.1 | 0.8 ± 0.1 | p = 0.93 |
| (0.4-1.0) | (0.5-1.0) | ||
| IOP (mmHg), mean ± SD (range) |
33.6 ± 8.8 | 32.6 ± 10.1 | p = 0.57 |
| (20-55) | (18–65) | ||
| Number of medication, mean ± SD (range) |
3.2 ± 0.9 | 3.1 ± 1.1 | p = 0.87 |
| (1 - 5) | (0 - 5) |
Table 1: Demographics and baseline ocular parameters.
IOP: intraocular pressure; SD: standard deviation; *percentages refer to the respective group (with/without prior intervention); § Fisher`s exact test was performed to compare both groups; P-value < 0.05 was determined to be statistically significant.
From the first postoperative day until the end of the one-year follow-up period, at each visit the mean IOP was significantly reduced from baseline in both groups (Figure 1). In Group A (nasal superior implantation), the mean IOP decreased significantly by 55% from preoperatively 33.6 ± 8.8 mmHg to 14.6 ± 3.2 mmHg at 12 months postoperatively (p= 0.000; Wilcoxon test), while in Group B (nasal inferior implantation) a mean IOP reduction by 54% from 32.6 ± 10.1 mmHg at baseline to 14.1 ± 4.3 mmHg at one year postoperatively was observed (p= 0.000; Wilcoxon test). The t-test analysis revealed a statistically significant difference between both groups at Week 1 (p=0.009) and Month 3 (p=0.031). Non-parametric tests confirmed a statistically significant lower IOP in eyes with nasal inferior XEN gel stent implantation as compared to eyes with superonasally located implants at Month 3 (p=0.023; Mann-Whitney-U-test). At all other visits, no significant differences in mean IOP were found between the two groups (p > 0.05; Mann-Whitney-U-test) (Figure 1). Regarding the proportion of eyes achieving target pressure values of 18 mmHg, 15 mmHg and 13 mmHg at one year postoperatively no significant differences were observed between both groups (p > 0.05; Chi square test) (Figure 2).
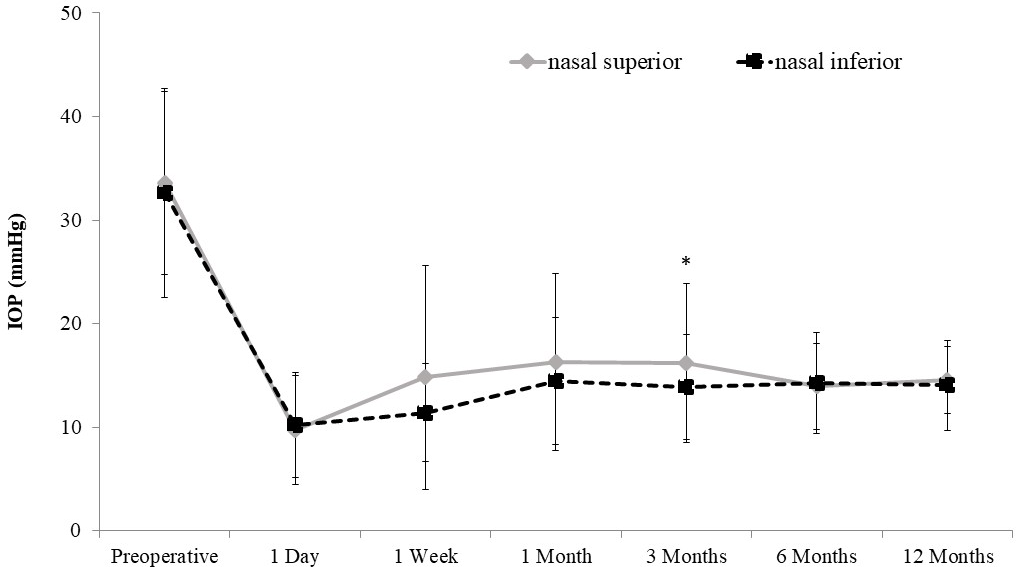
Figure 1: Mean IOP of eyes with XEN45 gel stent implantation in the nasal superior quadrant (n=56) and in the nasal inferior quadrant (n=96) at each study visit. Error bars indicate SD for the mean. Within each group, the mean IOP was significantly reduced from baseline at any visit during the follow-up period (p= 0.000; Wilcoxon test). While at month 3 a significant difference in mean IOP was detected between both groups (p=0.023; Mann-Whitney-U-test), no significant differences were observed at any other study visit (p > 0.05; Mann-Whitney-U-test).
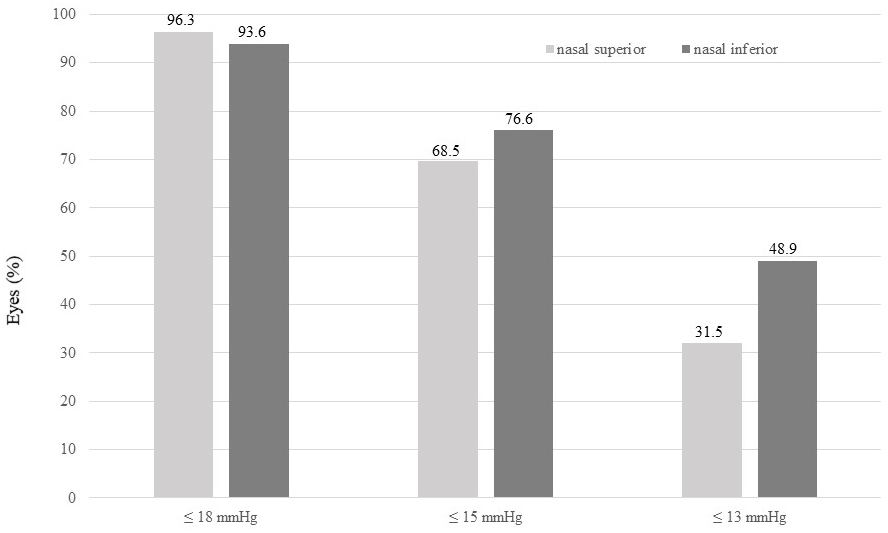
Figure 2: Proportion of eyes reaching a certain target pressure at 12 months postoperatively. Comparison of eyes with nasally superior (n=56) or nasally inferior implantation site (n=96). No significant differences were detected between groups.
Also, mean number of hypotensive medications was significantly reduced at every visit from the first postoperative day until Month 12 in both groups (Figure 3). While in Group A (nasal superior implantation) a significant reduction was observed from in mean 3.2 ± 0.9 medications at baseline to 0.3 ± 0.7 medications at 12 months postoperatively (p= 0.000; Wilcoxon test), in Group B (nasal inferior implantation) the mean number of medications had decreased from 3.1 ± 1.0 to 0.3 ± 0.7 (p= 0.000; Wilcoxon test). At Month 3, the required mean number of medications was significant lower in Group A as compared to Group B (p=0.021; Welch`s t-test), while at all other visits no significant differences between the groups were observed (p > 0.05; Welch`s t-test) (Figure 3).
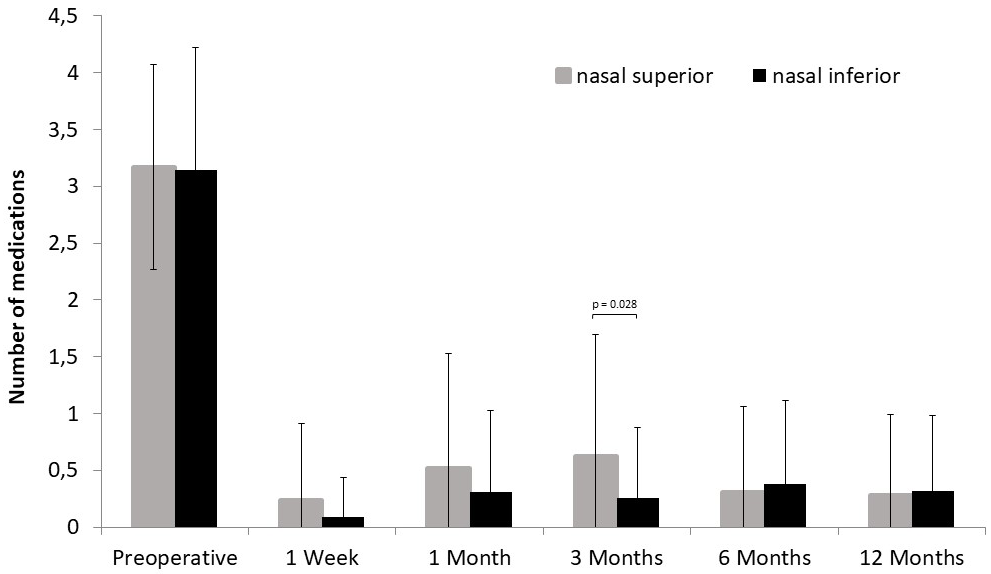
Figure 3: Mean number of anti-glaucoma medications of eyes with XEN45 gel stent implantation in the nasal superior quadrant (n=56) and in the nasal inferior quadrant (n=96) at each study visit. In each group the mean number of medication was significantly reduced from baseline at all visits (p= 0.000; Wilcoxon test). Between groups, significant differences were observed at Month 3 (p=0.021; Welch`s t-test). Error bars indicate SD for the mean.
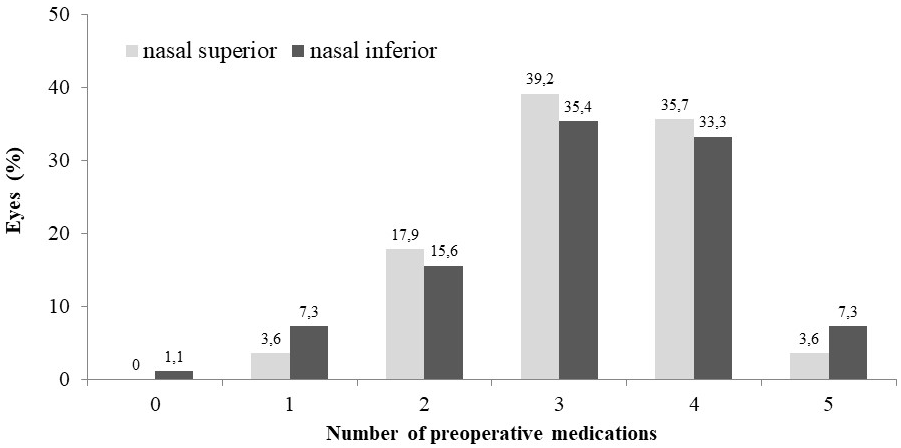
While in Group A (nasal superior implantation) 79% of eyes (44/56) had been on three or more hypotensive medications at baseline, this was the case in one eye at 12 months postoperatively. In Group B (nasal inferior implantation), three or more medications were required in 76% of eyes (73/96) preoperatively and in no eye at the end of the follow-up period (Figure 4 a, b). One year after XEN45 gel stent implantation, 86% of eyes (48/56) in Group A and 79% of eyes (76/96) in Group B were completely off drops (Figure 4b).
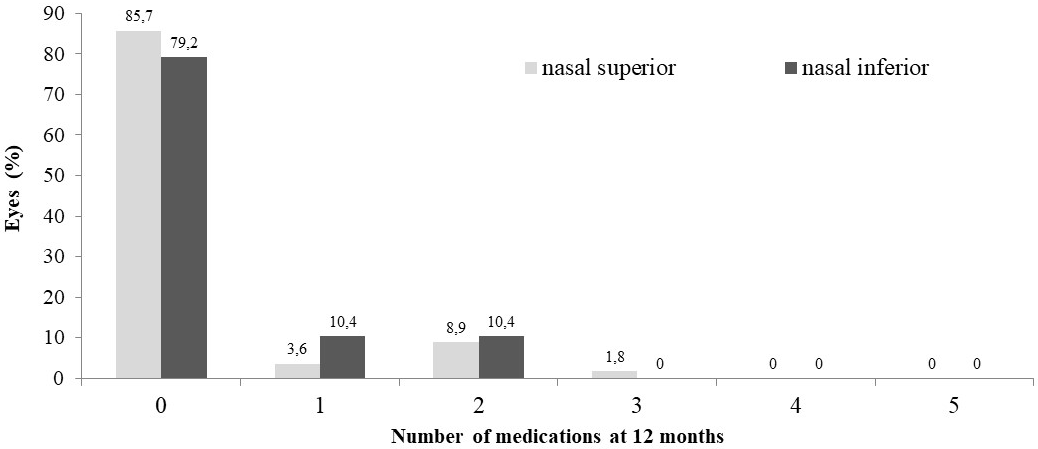
Figure 4: Proportion of eyes requiring 0 - 5 anti-glaucoma medications at a) baseline and b) at 12 months postoperatively. Comparison of eyes with XEN45 gel stent implantation in the nasal superior quadrant (n=56) and in the nasal inferior quadrant (n=96).
Qualified success, i.e. IOP reduction of at least 20% and an IOP value below 18 mmHg without or with medication was achieved in 64% (36/56) of eyes in Group A and 77% (74/96) of eyes in Group B at 12 months postoperatively. Complete success, i.e. an IOP reduction of at least 20% and an IOP value below 18 mmHg without medication, was experienced by 46% (26/56) of eyes in Group A and by 60% (58/96) of eyes in Group B one year after XEN45 implantation. However, the differences between the two groups regarding qualified and complete success were statistically not significant (p=0,095 and p=0.077; Log Rank).
In order to enhance outflow, needling of the bleb was required in 45% (25/56) of eyes in Group A (nasal superior implantation) and 27% (26/96) of eyes in Group B (nasal inferior implantation) within 12 months (p=0.031; Fisher`s exact test), with most needlings being performed beetween Week 1 and Month 3 in both groups. During the follow-up phase, 4 eyes of Group A (7.2%) and 7 eyes of Group B (7.3%) presented with uncontrollable IOP and received a second XEN45 gel stent implant.
Hypotony (IOP ≤ 6 mmHg) was observed in 3 eyes of Group A (5.3%) and 4 eyes of Group B (4.2%) at Month 1 postoperatively (p > 0.05). At Month 3, all hypotony cases of Group B had spontanously resolved, while in Group A two cases were still present but were resolved until Month 6. Visual acuity threatening complications related to hypotony such as choroidal effusion or hemorrhage, choroidal detachment, or macular folds were not observed in either group. In addition, no cases of corneal alteration, migration or exposure of the implant, wound leakage or endophthalmitis occurred in either group.
Discussion
Several studies have shown that ab-interno placement of the XEN45 gel stent offers a minimally invasive, effective surgical treatment option for open angle glaucoma.[15-22] Usually, the XEN45 gel stent is implanted superionasally, however, its positioning in the nasally inferior quadrant might completely spare the superior area for future trabeculectomies and might facilitate the implantation process. The results of our retrospective comparative analysis confirmed our hypothesis that nasal inferior implantation of the XEN45 gel stent is non-inferior to nasal superior implantation in terms of sucess rate, IOP decrease and medication reduction.
One-year after XEN45 gel stent implantation, success rates were statistically not significantly different between both groups, with 64% of eyes with nasal superior implantation and 77% of eyes with nasal inferior implantation reaching qualified success (i.e. IOP reduction of at least 20% and an IOP value below 18 mmHg without and with medication). Regardless of the implantation site, mean IOP was effectively reduced from over 30 mmHg at baseline to under 15 mmHg at 12 months and dependance on hypotensive medication was effectively reduced from at least 3 medications to 0.3 medications. While preoperatively the vast majority of eyes were on three or more medications, one year postoperatively 86% of eyes with nasal superior implantation and 79% of eyes with nasal inferior implantation were completely off drops. These results are consistent with those of other studies and show that the XEN45 stent IOP can effectively reduce and hypotensive drugs in glaucoma patients regardless of its implantation site. In view of these data, it seems reasonable to consider XEN45 gel stent implantation at an earlier point in glaucoma therapy in order to ensure long-term therapeutic success in glaucoma patients with insufficient adherence or side effects of medication. It is well known that topical and systemic side effects, difficulties in administering the drug, and the complexity of drug regimens can considerably affect patients` adherence with their therapy. In this context is also noteworthy a recent study showing that about one third of prescriptions in Germany remain unfulfilled.[6, 24, 25]
However, even though one year after XEN implantation there were no statistically significant differences regarding IOP decrease and medication reduction between the two groups, we observed significant differences in the early course of the follow-up period. At Month 3, both the mean IOP and the required mean medication were significantly lower in eyes with a nasally inferior implantation site. At the same time, needling, which was usually performed within the first three months, was significantly more frequently required in eyes with a superior nasally implanted XEN gel stent. This may suggest that in eyes with nasal inferior XEN45 gel stent implantation the resulting bleb allows a more pronounced aqueous humor outflow without further enhancement within the early postoperative period. At the same time, hypotension occurred only numerically and to a comparable extent in both groups indicating that the XEN45 stent, following the principles of the Hagen-Poiseuille law, is associated with a low risk of hypotony.
We do not yet have a reliable explanation why in the group of nasally inferior implanted XEN45 implants IOP and medication usage were lower at Month 3 and at the same time needling was required less often. One possible explanation would be that in our analysis such eyes were incidentally treated with a nasally inferior implanted XEN45 gel stent, which would not have required needling anyway. In this case, the implantation site would have no effect on the early postoperative response. In this context, it has to be mentioned that in a retrospective analysis by Tan et al in which the XEN45 stent was superonasally implanted in 39 eyes, no needling was required in half of the cases.[22] However, no baseline parameter could be determined to which a higher needling rate might be attributable. Another explanation would be that possibly the lower tension of the lower lid could be a reason for a more pronounced outflow after nasal inferior implantation of the XEN45 gel stent and a reduced needling rate. We postulate that the increased tension of the upper eyelid might lead to a greater flattening during the healing process resulting in a more pronounced fibrosis of the bleb in the early postoperative phase. If this were the case, a nasally inferior implantation of the XEN gel stent could be advantageous especially in eyes with high tension of the upper eyelid or in deep-set eyes. However, this assumption will have to be further investigated in studies also examining bleb anatomy.
Limitations of the current study include a retrospective design and a limited duration of follow up. Data were collected from a single center and there might be a a certain degree of selection bias as the decision to offer XEN45 gel stent implantation was determined by one surgeon, without strict inclusion or exclusion criteria. A prospective study with longer follow-up and including anatomically examination of the bleb would be required to assess whether a nasally inferior is advantageous to nasally superior implantation of the XEN45 gel implant.
Conclusion
Overall, the 1-year results of our retrospective analysis show that implantation of the XEN45 gel stents in the nasally inferior quadrant is at least as effective in reducing IOP and medication usage as implantation in the superior nasal quadrant. Nasally inferior implantation may be associated with a lower needling rate.
References
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. (2014). Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121(11): 2081–2090.
- Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M. (2002). Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 120: 1268–79.
- Weinreb RN, Aung T, Medeiros FA. (2014). The pathophysiology and treatment of glaucoma. JAMA 311(18): 1901–11.
- EGS. European Glaucoma Society guidelines, 4th ed. EGS; 2014.. Accessed November 2018.
- Lemij HG, Hoevenaars JG, van der Windt C, Baudouin C. (2015). Patient satisfaction with glaucoma therapy: reality or myth?. Clin Ophthalmol 9: 785–93.
- Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. (2003). Compliance barriers in glaucoma: a systematic classification. J Glaucoma12(5): 393–398.
- Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ, Schiffman JC; Tube Versus Trabeculectomy Study Group. (2012). Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol153(5): 804–814.
- Ansari, E. (2017). An Update on Implants for Minimally Invasive Glaucoma Surgery (MIGS). Ophthalmol Ther 6: 233–241.
- Vera VI, Horvath C. (2014). XEN Gel stent: the solution Designed by Aquesys. In: Samples JR, Ahmed IIK, eds. Surgical Innovations in Glaucoma. New York, Springer Science + Business Media NY 189-198.
- Lewis RA. (2014). Ab interno approach to the subconjunctival space using a collagen glaucoma stent. J Cat Refract Surg. 40:1301-1306.
- Fellman RL, Feuer WJ, Grover DS. (2015). Episcleral venous fluid wave correlates with trabectome outcomes: intraoperative evaluation of the trabecular outflow pathway. Ophthalmology. 122(12): 2385-2391.
- Sheybani A, Dick B, Ahmed IIK. (2016). Early Clinical Results of a Novel Ab Interno Gel Stent for the Surgical Treatment of Open-angle Glaucoma. J Glaucoma 25(7): e691-6.
- Yu DY, Morgan WH, Sun X, et al. (2009). The critical role of the conjunctiva in glaucoma filtration surgery. Prog Retin Eye Res 28(5): 303–328.
- Sheybani A, Reitsamer H, Ahmed IIK. (2015). Fluid Dynamics of a Novel Micro-Fistula Implant for the Surgical Treatment of Glaucoma. Invest Ophthalmol Vis Sci. 56(8): 4789–4795.
- Stalmans I, Fea A, Reitsamer H, Lavin C. (2015). A minimally invasive approach to sub?conjunctival outflow: 1 year results of an ab?interno gelatin stent in combination with preoperative MMC injection for the treatment of primary open angle glaucoma. Acta Ophthalmol 93.
- Grover DS, Flynn WJ, Bashford KP, et al. (2017). Performance and Safety of a New Ab Interno Gelatin Stent in Refractory Glaucoma at 12 Months. Am J Ophthalmol. 183: 25-36.
- Galal A, Bilgic A, Eltanamly R, Osman A. (2017). XEN Glaucoma Implant with Mitomycin C 1-Year Follow-Up: Result and Complications. J Ophthalmol. 2017: 5457246.
- De Gregorio A, Pedrotti E, Russo L, Morselli S. (2018). Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. Jun 38: 1129-1134.
- Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, et al. (2016). Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 91: 415–421.
- Hengerer FH, Kohnen T, Mueller M, Conrad-Hengerer I. (2017). Ab Interno Gel Implant for the Treatment of Glaucoma Patients With or Without Prior Glaucoma Surgery - One Year Results. J Glaucoma. 26(12): 1130-1136.
- Chaudhary A, Salinas L, Guidotti J, Mermoud A, Mansouri K. (2018). XEN Gel Implant: a new surgical approach in glaucoma. Expert Rev Med Devices. 15:47-59.
- Tan SZ, Walkden A, Au L. (2018). One-year result of XEN45 implant for glaucoma: efficacy, safety, and postoperative management. Eye (Lond). Feb 32: 324-332.
- IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.
- Quaranta L, Riva I, Gerardi C, et al. (2016). Quality of Life in Glaucoma: A Review of the Literature. Adv Ther 33(6): 959–981.
- Frech S, Kreft D, Guthoff RF, Doblhammer G. (2018). Pharmacoepidemiological assessment of adherence and influencing co-factors among primary open-angle glaucoma patients. An observational cohort study. PLoS ONE 13(1): e0191185.
Citation: Fritz H. Hengerer, Gerd Auffarth and Ina Conrad-Hengerer. (2019). Nasal Superior Versus Nasal Inferior Implantation of the Xen45 Gel Stent – One Year Results. Journal of Ophthalmology and Vision Research 1(1). DOI: 10.5281/zenodo.3373285
Copyright: © 2019 Fritz H. Hengerer. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.