Case Report
Volume 3 Issue 1 - 2021
Macrodystrophia Lipomatosa Extending into the Abdominal Wall and Breast: A Case report
1Department of Plastic Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
2Wuhan Clinical Research Center for Superficial Organ Reconstruction, Wuhan, 430022, China
2Wuhan Clinical Research Center for Superficial Organ Reconstruction, Wuhan, 430022, China
*Corresponding Author: Nengqiang Guo, 1277 Jiefang Avenue, Wuhan, 430022, China.
Received: February 20, 2021; Published: March 13, 2021
Abstract
We report a 32-years-old woman diagnosed with macrodystrophia lipomatosa. In addition to the typical abnormality of the limb (right lower extremity), lesions were seen in the abdominal wall and breast. This is a rare case in which the hypertrophied lipomatous tissue extends into the abdominal wall and breast. Thus, our case adds to the understanding and diagnosis of this disease.
Keywords: Macrodystrophia lipomatosa; Macromelia; Abdominal wall; Breast
Introduction
Macrodystrophia lipomatosa is a rare nonhereditary developmental malformation that mainly affects fibro-adipose tissue. Clinically, it manifests as gigantism affecting one or more digits of the hand or foot. [1] In 1925, it was first described by Feriz as the localized gigantism of the lower limb. [2] Here, we report a case of macrodystrophia lipomatosa affecting the entire right lower limb with extension of hypertrophied fatty tissue into the abdominal wall and breast. This is the first time such a case has been documented worldwide.
Case Presentation
A 32-years-old woman was born with an abnormally elongated and thickened right leg, a condition that progressively worsened. The patient complained that she was unable to walk and her knee was flexed. Physical examination revealed that in addition to the right leg, there was a palpable mass in the right abdominal wall and the left breast (Figure 1A). X-ray examination showed that pelvis was deflected, cortex of femur, fibula and tibia of the right leg was rough and hypertrophied. Moreover, osseous prominences were seen on the proximal ends, and the patella was not visible. The bones of the right foot were irregular, and the joints were obscured (Figure 1B).
Computed tomography angiography (CTA) showed that the vessels of right leg were smooth but abnormally elongated and thickened, without malformed vessel cluster. Muscles of right leg were atrophied with obviously thicken adipose tissue (Figure 1C). Based on the above clinical manifestations and examination results, a primary diagnosis of macrodystrophia lipomatosa was made. Amputation, volume reduction and liposuction were performed to manage the lesions. During operation, extremely thickened subcutaneous adipose tissue and many thickened vessels were seen, and part of the muscles presented with fat degeneration. Histological examination revealed hyperplastic fibro-adipose tissue, which was similar between the left breast and right abdominal wall. Part of the muscles were infiltrated by adipocytes, with intramuscular fatty hyperplasia, muscle fiber degeneration and loss of striation (Figure 1D). Combined with the pathological results, she was diagnosed with macrodystrophia lipomatosa, which extended into the abdominal wall and breast. No adverse events were observed post-operation, and the patient was satisfied with the operation outcomes.
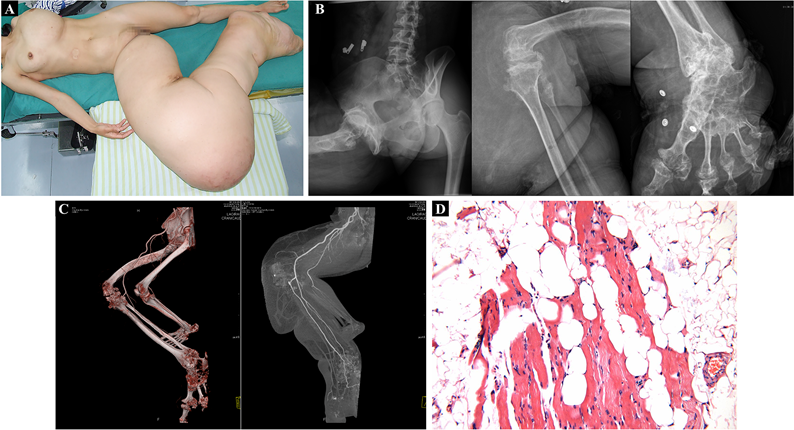
Figure 1: (A) Clinical photographs of the patient. (B) X-ray of right lower limb. (C) CTA of right lower limb. (D) Representative histology image of the specimens of all the lesions.
Discussion
Unilateral macromelia occurs in many cases such as lymphedema, lymphangioma, neuro?bromatosis, and Klippel-Trenaunay-Weber syndrome.[3] In general, the clinical history and a thorough physical examination can help distinguish these entities. The above diseases cause thickening of local or total unilateral limb but elongation of limb. The present case is most likely to be macrodystrophia lipomatosa based on the clinical presentation. Histopathologically, macrodystrophia lipomatosa is characterized with benign fibro-fatty infiltration involving the soft tissues of the distal arm of leg, similar to this case. However, unlike previous reports, the present case manifested with extensive and huge lesions. In addition, the abdominal wall and breast were also involved, which is different from former studies.[4] Histopathological features of this case are similar to those of congenital infiltrating lipomatosis (CIL), a rare congenital disease diagnosed during infancy, while CIL always involves the face but not limbs. [5] It is worth mentioning that, so far, none has reported cases of macrodystrophia lipomatosa involving the abdominal wall and breast. Therefore, our case adds to the understanding and diagnosis of this disease.
Funding: This study was funded by the National Key R&D Program of China (2019YFA0110500).
Conflicts of interest: None.
Referances
- Gao B, Zheng L P, Cai Z D. (2010). Limb salvage surgery in a patient with macrodystrophia lipomatosa involving an entire upper extremity. Chin Med J (Engl). 123: 2744-7.
- Feriz H. (1926). Makrodystrophia lipomatosa progressiva. Virchows Archiv: an international journal of pathology. 260: 308-68.
- Berchiolli R, Marconi M. (2018). Klippel-Trenaunay Syndrome: A Dramatic Presentation. Eur J Vasc Endovasc Surg. 56: 299.
- Fritz TR, Swischuk LE. (2007). Macrodystrophia lipomatosa extending into the upper abdomen. Pediatr Radiol. 37: 1275-7.
- Li Y, Chang G, Si L, Zhang H, Chang X, Chen Z, et al. (2017). Congenital Infiltrating Lipomatosis of the Face. Ann Plast Surg. 80(1): 83–89.
Citation: Jian Liu, Jiaming Sun, Liang Guo, Zhenxing Wang and Nengqiang Guo. (2021). Macrodystrophia Lipomatosa Extending into the Abdominal Wall and Breast: A Case report. Journal of Gynaecology and Paediatric Care 3(1). DOI: 10.5281/zenodo.4616363
Copyright: © 2021 Nengqiang Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
