Research Article
Volume 1 Issue 2 - 2019
Laser Blended Vision versus PresbyLASIK for Correction of Presbyopia and Myopic Astigmatism
From the State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Centre, Sun Yat-sen University, Guangzhou, People’s Republic of China
*Corresponding Author: Fang Liu MD, From the State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Centre, Sun Yat-sen University, Guangzhou, People’s Republic of China.
Received: October 31, 2019; Published: November 16, 2019
Abstract
Purpose: To compare the efficacy and safety of aspheric micro-monovision LASIK (LBV) and hybrid bi-aspheric multifocal central presbyLASIK (PresbyMAX) treatments for correction of presbyopia and myopic astigmatism.
Methods: Forty-eight eyes of 24 patients with presbyopia and myopic astigmatism had consecutively bilaterally treated with aspheric micro-monovision LASIK (LBV) and hybrid bi-aspheric multifocal central presbyLASIK (PresbyMAX) were assessed. The mean age of the patients was 45.33±3.0 years with a mean spherical equivalent refraction of -6.18±1.69 diopters (D) and mean astigmatism of -0.79±0.54D. Visual acuity, manifest refraction, contrast sensitivity, binocular sensorial function and patients’ subjective rating were evaluated pre- and postoperatively.
Results: At 6 months postoperatively, the mean uncorrected distance visual acuity (UDVA), uncorrected intermediate visual acuity (UIVA) and uncorrected near visual acuity (UNVA) improved significantly in both groups. Seventeen percent (4/24) eyes in both groups lost 1 line and no eyes lost 2 lines of CDVA. For both groups, the changes in binocular contrast sensitivity (CS) in all test conditions were not significantly different at any frequency. A more severe drop of CS threshold for PresbyMAX was observed, especially under mesopic condition. Near stereo acuity improved but distance stereo acuity decreased significantly in both groups. Night visions were not compromised in both groups. The overall satisfaction score for surgery were 93.33±5.53 in LBV group and 91.25±6.50 in PresbyMAX group.
Conclusions: LBV and PrebyMAX were equally effective and safe for myopia patients with presbyopia, showing that choosing one of them is a safe alternative when another is not available.
Introduction
Effectively and safely correction for presbyopia with myopic astigmatism using laser in situ keratomileusis (LASIK) remains a challenge due to lack of perfect option with no compromised occurring (e.g. night vision, monocular distance vision or stereopsis). [1] Although there is no perfect solution, different surgical methods are currently available (monovision, multifocality, asphericity modification) and appear to be efficacious for myopic presbyopes. [2]
Using an aspheric ablation profile, Reinstein et al. successfully combined monovision and extended depth of field in a so-called micro-monovision or laser blended vision (LBV) in 2009. [3] The dominant eye was targeted for exactly Plano. However, the non-dominant eye was targeted for slight myopia with an ideal target of -1.50 D. In addition, this proprietary non-linear aspheric ablation profile induces a controlled amount of spherical aberration to extend the binocular depth of focus to yield adequate distance and near vision and provide a blend zone to enable continuous distance to intermediate to near vision between the two eyes.
The term presbyLASIK, first was introduced by Ruiz et al, represents a surgical procedure to create a multifocal corneal surface based on traditional LASIK. [4] This technique reshapes corneal asphericity by creating a central steeper (named central presbyLASIK) or peripheral steeper (named peripheral presbyLASIK) corneal surface to induce an amount of spherical aberration, and as a result extends depth of focus to yield adequate distance and near vision. [1] As one kind of central presbyLASIK, the hybrid bi-aspheric multifocal central presbyLASIK approach exists which has a central area for near vision correction and is surrounded by a pericentral area where ablation is calculated for distance emmetropia. Besides, the hybrid surgical technique also combines micro-monovision which treats the dominant eye toward distance vision (target refraction-0.13D) and the nondominant eye toward near vision (target refraction -0.89 D). A hybrid bi-spheric multifocal central presbyLASIK concept was used in this study which has also been known as PresbyMAX Hybrid. [5-7]
The efficacy, safety, predictability and stability of LBV and PrebyMAX have been demonstrated in several reports, respectively. However, to our knowledge, there is no study which has compared the efficacy and safety of LBV and PresbyMAX treatments for correction of presbyopia and myopic astigmatism. Both of these two techniques combine micro-monovision and spherical aberration induced, so it’s interesting to compare their efficacy and safety for presbyopia correction. This prospective, randomized controlled study analyzed and compared the efficacy and safety of aspheric micro-monovision LASIK (LBV) and hybrid bi-aspheric multifocal central presbyLASIK treatments for correction of presbyopia and myopic astigmatism.
Materials and Methods
Patient Population and Examinations
This study was a prospective, randomized controlled study. Forty-eight eyes of 24 patients with presbyopia and myopic astigmatism undergoing bilateral laser in situ keratomileusis (LASIK) for refractive presbyopic corrections were enrolled from Zhongshan Ophthalmic Center in Guangzhou, People’s Republic of China. Inclusion criteria were medically suitable for LASIK, presbyopic with a corrected distance visual acuity of 20/25 or better in both eyes and tolerance of at least -0.75 D anisometropia, photopic pupil diameter smaller than 3.5 mm and mesopic pupil diameter lager than 4.5mm (photopic pupil diameter from topography (offset) information but mesopic/scotopic from pupillometry). Patients who suffered from systemic illness, had previous ocular surgery, or had abnormal corneal topography were excluded from the study. Additional exclusion criteria were clinically relevant lens opacity (evaluated using slit lamp), any signs of binocular vision anomalies at distance and near and a pupil offset of 0.7 mm or more. This study followed the tenets of the Declaration of Helsinki. The study was approved by the Medical Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-Sen University.
This study was a prospective, randomized controlled study. Forty-eight eyes of 24 patients with presbyopia and myopic astigmatism undergoing bilateral laser in situ keratomileusis (LASIK) for refractive presbyopic corrections were enrolled from Zhongshan Ophthalmic Center in Guangzhou, People’s Republic of China. Inclusion criteria were medically suitable for LASIK, presbyopic with a corrected distance visual acuity of 20/25 or better in both eyes and tolerance of at least -0.75 D anisometropia, photopic pupil diameter smaller than 3.5 mm and mesopic pupil diameter lager than 4.5mm (photopic pupil diameter from topography (offset) information but mesopic/scotopic from pupillometry). Patients who suffered from systemic illness, had previous ocular surgery, or had abnormal corneal topography were excluded from the study. Additional exclusion criteria were clinically relevant lens opacity (evaluated using slit lamp), any signs of binocular vision anomalies at distance and near and a pupil offset of 0.7 mm or more. This study followed the tenets of the Declaration of Helsinki. The study was approved by the Medical Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-Sen University.
Baseline examinations included measurement of manifest refraction, corrected and uncorrected distance visual acuity, uncorrected near visual acuity, uncorrected intermediate visual acuity, presbyopic addition, contrast sensitivity, corneal topography, ultrasound corneal pachymetry, pupillometry and subjective rating questionnaires. Postoperative follow-up visits were scheduled at 1 week, 1 month, 3 months and 6 months after surgery.
Near acuity and intermediate acuity were measured under the same lighting conditions in one optometry room using the Sloan Letter Near Vision Card-729000 which was designed such that the card is 40 cm away from the patient’s eye when a bead on a 40-cm cord is placed at the patient’s lateral canthus and using the COLENBRANDER MIXED CONTRAST CARD SET which was designed such that the card is 63cm or 100cm away from the patient’s eye when a bead on a 63 or 100-cm cord is placed at the patient’s lateral canthus.
The main refractive outcome measures included safety, efficacy and predictability. Safety was evaluated by changes of lines of corrected distance visual acuity pre- to post-operation, while the safety index was the mean postoperative corrected distance visual acuity divided by the mean preoperative corrected distance visual acuity (expressed in decimal notation). Efficacy was evaluated by the change of preoperative corrected distance visual acuity and the uncorrected distance visual acuity 6 months postoperatively, and the efficacy index was the uncorrected distance visual acuity 6 months postoperatively divided by the corrected distance visual acuity preoperatively (expressed in decimal notation).
Contrast sensitivity with distance correction in photopic and mesopic conditions was measured at 3, 6, 12, and 18 cycles per degree using the CSV-1000.
Stereo acuity was evaluated using the near and distance random dot test. The random dot stereo acuity was measured at 40 cm for near and 3 m for distance. It was tested with best spectacle correction preoperatively and without correction postoperatively. If the patient could not appreciate even the maximum disparity plate nor had nil stereopsis, then an arbitrary value of 1000 seconds of arc was recorded as the result.
Subjective patient-reported outcomes were assessed using questionnaire: The questionnaire included 6 items about satisfaction of (1) near vision, (2) distance vision, (3) intermediate vision, (4) night vision, (5) dependence on glasses and (6) overall satisfaction with correction. (Table 1 shown the questionnaire items) Each scale ranged from 0 to 100, where 0 indi¬cated not at all satisfied (or has no need glasses) and 100 indicated completely satisfied (or completely need glasses).
| 1. Evaluate your near vision (eg.reading book or cellphone) before/after treatment, the satisfaction score is: Score (0-100): 0 indicated not at all satisfied and 100 indicated completely satisfied. |
| 2. Evaluate your distance vision before/after treatment, the satisfaction score is: Score (0-100): 0 indicated not at all satisfied and 100 indicated completely satisfied. |
| 3. Evaluate your intermediate vision (eg.using computer/playing mahjong/cooking) before/after treatment, the satisfaction score is: Score (0-100): 0 indicated not at all satisfied and 100 indicated completely satisfied. |
| 4. Evaluate your night vision before/after treatment, the satisfaction score is: Score (0-100): 0 indicated not at all satisfied and 100 indicated completely satisfied. |
| 5. Do you still depend on glasses after the treatment? Score (0-100): 0 indicated have no need glasses and 100 indicated completely depend on glasses. |
| 6. Considering all the items related to the treatment, the overall satisfaction score is: Score (0-100): 0 indicated not at all satisfied and 100 indicated completely satisfied. |
Table 1: Questionnaire of Patients’ Satisfaction.
Treatment Plan
After a full ophthalmologic examination was performed on all patients prior to surgery, patients were tested to determine their dominant eye by the “hole test.” [3] Then patient’s tolerance was measured by simulating the intended postoperative refraction using a phoroptor and using trial frames as previous described. [3,8]. For LBV treatment group, ocular wavefront data from the WASCA aberrometer were imported into CRS-Master software platform to plan the aspheric ablation profile. For PresbyLASIK treatment group: The PresbyMAX treatment planning module in hybrid mode was used to generate the ablation profiles. The sphere and cylinder values in both group entered into the laser were based on the manifest refraction without nomogram adjustment. A target of -1.50 D was used for all non-dominant eyes in LBV group and which was -0.89D used in PresbyMAX group.
After a full ophthalmologic examination was performed on all patients prior to surgery, patients were tested to determine their dominant eye by the “hole test.” [3] Then patient’s tolerance was measured by simulating the intended postoperative refraction using a phoroptor and using trial frames as previous described. [3,8]. For LBV treatment group, ocular wavefront data from the WASCA aberrometer were imported into CRS-Master software platform to plan the aspheric ablation profile. For PresbyLASIK treatment group: The PresbyMAX treatment planning module in hybrid mode was used to generate the ablation profiles. The sphere and cylinder values in both group entered into the laser were based on the manifest refraction without nomogram adjustment. A target of -1.50 D was used for all non-dominant eyes in LBV group and which was -0.89D used in PresbyMAX group.
Excimer Laser
All surgeries were performed by one experienced surgeon (Q.L.). All eyes underwent LBV using the MEL 80 excimer laser, and underwent presbyLASIK with a biaspheric multifocal ablation profile in aberration-free mode using an AMARIS 750S excimer laser. LASIK flaps in both groups were all cut using Carl Zeiss VisuMax femtosecond laser platform with superior hinge, 100-μm intended flap thickness. Topical eye drops of proparacaine were instilled as anesthetic.
All surgeries were performed by one experienced surgeon (Q.L.). All eyes underwent LBV using the MEL 80 excimer laser, and underwent presbyLASIK with a biaspheric multifocal ablation profile in aberration-free mode using an AMARIS 750S excimer laser. LASIK flaps in both groups were all cut using Carl Zeiss VisuMax femtosecond laser platform with superior hinge, 100-μm intended flap thickness. Topical eye drops of proparacaine were instilled as anesthetic.
Data Analysis
Outcome measures were calculated and plotted according to the standardized guidelines set out by Waring. [9] Visual acuity exams and calculations used the logarithm of minimum angle of resolution (logMAR) and the reading acuity determination (logRAD) and were converted to Snellen or revised Jaeger acuities for data reporting purposes only. Patient data were entered into an Excel spreadsheet and statistical analysis was performed using the SPSS statistical package. Paired Student’s t tests were performed for uncorrected distance visual acuity, uncorrected near visual acuity, corrected distance visual acuity, uncorrected intermediate visual acuity and contrast sensitivities. The Wilcoxon signed-rank test was performed to determine the changes in stereo acuity. A P value less than .05 was considered statistically significant.
Outcome measures were calculated and plotted according to the standardized guidelines set out by Waring. [9] Visual acuity exams and calculations used the logarithm of minimum angle of resolution (logMAR) and the reading acuity determination (logRAD) and were converted to Snellen or revised Jaeger acuities for data reporting purposes only. Patient data were entered into an Excel spreadsheet and statistical analysis was performed using the SPSS statistical package. Paired Student’s t tests were performed for uncorrected distance visual acuity, uncorrected near visual acuity, corrected distance visual acuity, uncorrected intermediate visual acuity and contrast sensitivities. The Wilcoxon signed-rank test was performed to determine the changes in stereo acuity. A P value less than .05 was considered statistically significant.
Results
The average age of the 24 patients (11 male and 13 female) was 45.33±3.0 years (range 41 to51 years). The mean preoperative spherical equivalent was -6.18 ±1.69 D (-2.50 to -9.375), with mean preoperative astigmatism -0.79 ±0.54 D (up to -2.25) and mean spectacle near addition +1.75±0.43D (+0.75 to +2.00D).Baseline data of two groups was shown in Table 2.
| LBV Group | PresbyMAX Group | P | |
| No. | 12 Patients (24 eyes) | 12 Patients (24 eyes) | - |
| Gender ratio(M/F) | 0.71 (5/7) | 1(6/6) | .70 |
| Age(years) | 45±2.74 (41 to 50) | 45.67±3.22 (41 to 51) | .79 |
| Monocular UDVA (LogMAR) | 0.62±0.21 (0.30 to 1) | 0.64±0.21 (0.40 to 1) | .87 |
| Monocular CDVA (LogMAR) | -0.04±0.06 (-0.18 to 0) | -0.04±0.05 (-0.18 to 0) | .92 |
| Binocular DCIVA (LogMAR)-63cm | 0.29±0.10 (0.15 to 0.40) | 0.28±0.10 (0.10 to 0.40) | .89 |
| Binocular DCIVA (LogMAR)-100cm | 0.30±0.12 (0.15 to 0.40) | 0.31±0.12 (0.15 to 0.40 ) | .86 |
| Binocular DCNVA (LogRAD) | 0.42±0.13 (0.22 to 0.70) | 0.40±0.19 (0.22 to 0.52) | .94 |
| Spherical equivalent (D) | -6.19±1.55 (-2.75 to -9.38) | -6.16±1.81 (-2.5 to -9.25) | .76 |
| Astigmatism (D) | -0.97±0.61 D (0 to -2.25) | -0.61±0.0.40 (0 to -1.50) | .45 |
| Pupil diameter (mm) | |||
| Photopic pupil | 2.74±0.10 (2.00 to 3.40 ) | 2.70±0.13 (2.00 to 3.50 ) | .98 |
| Mesopic pupil | 5.21±0.21 (4.50 to 6.60 ) | 5.30±0.19 (4.50 to 6.70 ) | .95 |
| Scotopic pupil | 6.11± 0.25 (5.50 to 7.40 ) | 6.30±0.35 (5.70 to 7.30 ) | .96 |
| All values are presented as mean ± standard deviation (range); UDVA=Uncorrected Distance Visual Acuity; CDVA=Corrected Distance Visual Acuity; DCIVA=Distance Corrected Intermediate Visual Acuity, represents distance corrected without spectacle near addition; DCNVA=Distance Corrected Near Visual Acuity, represents distance corrected without spectacle near addition; D=Diopter. LBV group: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser, PresbyMAX group:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser. | |||
Table 2: Summary of the Preoperative data in two groups.
Efficacy: The mean monocular uncorrected distance visual acuity and corrected distance visual acuity of dominant eyes and non-dominant eyes, and binocular 63-cm uncorrected intermediate visual acuity, 100-cm uncorrected intermediate visual acuity and uncorrected near visual acuity were shown in Table 3. At 6 months after surgery, in both groups, the mean monocular uncorrected distance visual acuity, corrected distance visual acuity and binocular uncorrected near visual acuity improved significantly. The mean monocular uncorrected near visual acuity of dominant eyes in PresbyMAX group better than LBV group postoperatively (P=.01). The mean uncorrected intermediate visual acuity at 63 cm and 100 cm binocularly increased in both groups but have no significant difference. Efficacy index were 1.00±0.14 and 0.95±0.12 in LBV group and PresbyMAX group, respectively. There was no significant difference in efficacy index between the 2 groups.
| LBV Group | PresbyMAX Group | P | |
| No. | 12 Patients (24 eyes) | 12 Patients (24 eyes) | - |
| Binocular UDVA (LogMAR) | -0.03±0.05 (-0.08 to 0.1) | -0.02±0.06 (-0.08 to 0.1) | .85 |
| Binocular CDVA (LogMAR) | -0.03±0.05 (-0.18 to 0) | -0.03±0.05 (-0.18 to 0) | .68 |
| Binocular UIVA (LogMAR)-63cm | 0.06±0.07 (0 to 0.22) | 0.07±0.07 (0 to 0.22) | .92 |
| Binocular UIVA (LogMAR)-100cm | 0.13±0.09 (0 to 0.22) | 0.15±0.07 (0 to 0.22) | .58 |
| Binocular UNVA (LogRAD) | 0.04±0.05 (0 to 0.10) | 0.04±0.05 (0 to 0.10) | .76 |
| Monocular UDVA (LogMAR) | |||
| Dominant eyes | -0.01±0.05 (-0.08 to 0) | 0.02±0.04 (0 to 0.10) | .13 |
| Non-dominant eyes | 0.37±0.10 (0.22 to 0.52) | 0.41±0.15 (0.22 to 0.70) | .29 |
| Monocular UNVA (LogMAR) | |||
| Dominant eyes | 0.37±0.11 (0.22 to 0.52) | 0.25±0.07 (0.15 to 0.40) | .01 |
| Non-dominant eyes | 0.05±0.07 (0 to 0.22) | 0.06±0.07 (0 to 0.22) | .29 |
| Spherical equivalent (D) | |||
| Dominant eyes | -0.14±0.21 (-0.5 to 0.125) | -0.11±0.35 (-0.5 to 0.625) | .83 |
| Non-dominant eyes | -1.49±0.23 (-1.875 to -1.00) | -0.91±0.40 (-1.625 to -0.125) | .001 |
| Astigmatism (D) | |||
| Dominant eyes | -0.19±0.21 D (-0.5 to 0) | -0.21±0.39 D (-1.00 to 0.50) | .88 |
| Non-dominant eyes | -0.23±0.24 D (-0.75 to 0) | -0.125±0.22 D (-0.75 to 0) | .50 |
| Efficacy index | 1.00±0.14 | 0.95±0.12 | .37 |
| Safety index | 1.00±0.08 | 0.99±0.09 | .70 |
| All values are presented as mean ± standard deviation (range); UDVA=Uncorrected Distance Visual Acuity; CDVA=Corrected Distance Visual Acuity; UIVA=Uncorrected Intermediate Visual Acuity; UNVA=Uncorrected Near Visual Acuity; D=Diopter. LBV group: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser, PresbyMAX group:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser. | |||
Table 3: Summary of the Postoperative data in two groups.
Safety: All eyes achieved corrected distance visual acuity of 20/25 or better postop¬eratively. There was a binocularly loss of one line corrected distance visual acuity after surgery for 17% ( 4/24) eyes and no eyes lost 2 lines (Figure 1). No intraoperative complications occurred. In the LBV group, 21% ( 5/24) eyes gained one line of corrected distance visual acuity and which was 8 %( 2/24) in the PresbyMAX group. Safety index were 1.00±0.08 and 0.99±0.09 in LBV group and PresbyMAX group, respectively. There was no significant difference in safety index between the 2 groups (Table 3)
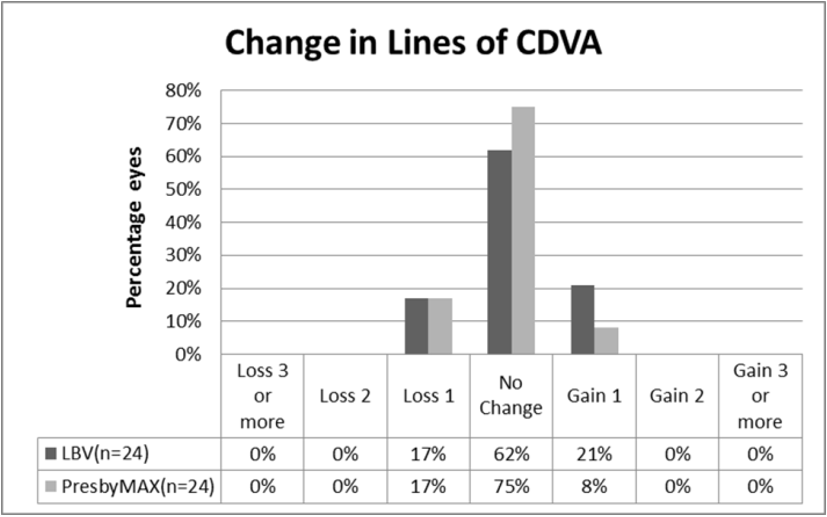
Figure 1: Changes in corrected distance visual acuity (CDVA) at 6 month follow-up after treatment in both groups.Loss, gain or no change represent the changes of lines of corrected distance visual acuity pre- to post-operation;LBV : underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser,PresbyMAX :underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser.
Accuracy: Figure 2 shows the scatterplot and linear regression analyses of the attempted correction of spherical equivalent against the achieved correction of spherical equivalent at 6 months postoperatively. The relationship between the attempted correction and achieved correction was strong in both groups, which correlation coefficient was 0.977 and 0.958, respectively (P <.05). Although the relationship between the attempted correction and achieved correction was strong (correlation coefficient=0.977, P <.01), there is a slight under correction in the achieved spherical equivalent refraction in LBV group.
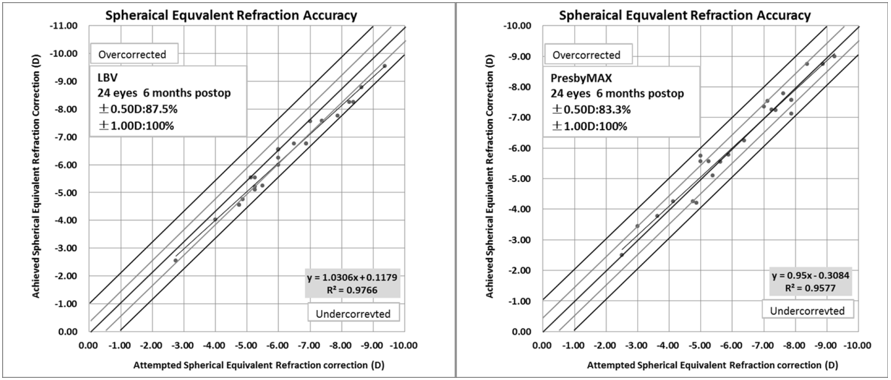
Figure 2: Linear regression analysis of the spherical equivalent attempted correction against the spherical equivalent achieved correction 6 months postoperatively in both groups.±0.50 D (±1.00D): within ±0.50 D (±1.00D) of target correction of spherical equivalent. LBV: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser,PresbyMAX:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser.
Binocular Sensorial Function: Baseline near and distance stereo acuity in two groups has no significant differences (P=.94 and .93, respectively); at 6 months after treatment, the near stereo acuity significantly improved in both groups (P=.04 and .03, respectively), but between groups there is no significant difference(P=.88); the distance stereo acuity significantly decreased in both groups after 6 months postoperatively (P=.000 and .001, respectively), but there is also no significant difference between two groups (P=.36). (Table 4)
| Preop | LBV Group (n=12) | PresbyMAX Group (n=12) | *P (between groups) |
| Anisometropia (D) | 0.56±0.65 (0 to 2.5) | 0.53±0.56 (0 to 2.25) | .90 |
| Distance stereo acuity | 270±264.51 (60 to 1000) | 261.67±258.65 (60 to 1000) | .94 |
| Median | 150 | 200 | - |
| Near stereo acuity | 79.17±46.99 (40 to 200) | 80.83±46.27 (40 to 200) | .93 |
| Median | 60 | 70 | - |
| Postop (6moths) | LBV Group (n=12) | PresbyMAX Group (n=12) | *P Value (between groups) |
| Anisometropia (D) | 1.35±0.35 (0.75 to 1.88) | 0.80±0.41 (0.38 to 1.63 ) | .003 |
| Distance stereo acuity | 850±271.36 (400 to 1000) | 733.33±319.72 (200 to 1000) | .36 |
| Median | 1000 | 1000 | - |
| **P (Pre- to Post) | .000 | .001 | - |
| Near stereo acuity | 47.5±14.22 (30 to 70) | 46.67±12.30 (30 to 70) | .88 |
| Median | 40 | 40 | - |
| **P (Pre- to Post) | .04 | .03 | - |
| All values are presented as mean ± standard deviation (range); Units of stereo acuity was seconds of arc; *P represents that data were compared between two groups postoperatively, **P represents that data were compared in the same group from pre- to post-operation; D=diopter. LBV group: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser, PresbyMAX group:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser. | |||
Table 4: Stereo acuity data after surgery.
Contrast Sensitivity: Figure 3 showed the preoperative and postoperative contrast sensitivity (CS) at spatial frequencies (SF) of 3, 6, 12 and 18 cycles per degree (cpd), under photopic, mesopic and mesopic with glare lighting conditions. Both groups have similar initial contrast sensitivity at 3 cpd, 6 cpd, 12 cpd and 18 cpd under all conditions (P>.05). Changes in contrast sensitivity scores were assessed under photopic condition and mesopic condition with and without the disability glare at 1 month and 6 months postoperatively. For both groups, at 1 month or 6 months follow-up, compared in logarithmic scale, the changes in binocu¬lar contrast sensitivity from the preoperative values in all test conditions were not significantly different at any frequency (P > .05). Figure 4 compares the magnitude of contrast sensitivity drop between LBV treatment and PresbyMAX treatment under different conditions. A more severe drop of contrast sensitivity threshold for PresbyMAX was observed at all spatial frequencies under mesopic lighting condition. Besides, a more severe drop of contrast sensitivity threshold for PresbyMAX was also observed at 6cpd, 12cpd and 18cpd spatial frequencies under photopic lighting condition and at 6cpd spatial frequencies under mesopic lighting condition with glare, but there are no significant differences between two groups at these frequencies.
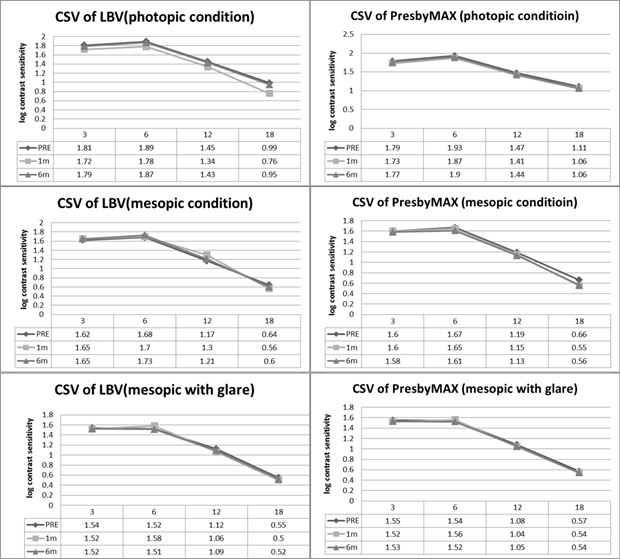
Figure 3: The preoperative and postoperative contrast sensitivity Visual Acuity (CSV) at spatial frequencies of 3, 6, 12 and 18 cycles per degree, under photopic, mesopic and mesopic with glare lighting conditions in both groups. PRE:preoperative; m:month. LBV: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser, PresbyMAX:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser.
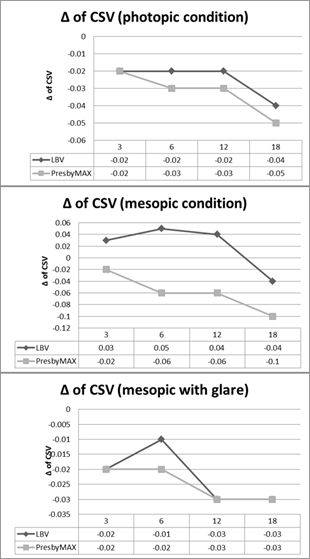
Figure 4: Comparing the magnitude of contrast sensitivity Visual Acuity (CSV) drop between LBV treatment and PresbyMAX treatment under photopic, mesopic and mesopic with glare lighting conditions. Δ of CSV :The magnitude of CSV change pre- to post- operation. LBV: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser, PresbyMAX:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser.
Subjective Rating: Table 5 shows the subjective rating after treatments. At 6 months after treatments, the overall satisfactions with correction were 93.33±5.53 (range 80 to 100) and 91.25±6.50 (range 80 to 100) in LBV group and PresbyMAX group, respectively. The satisfaction scores for near vision, intermediate vision and distance vision improved significantly in both groups from pre- to post- operations. The satisfaction scores for night vision after treatments slightly increased but have no significant change in both groups (P=.35 and 0.40, respectively). All patients were independent of near spectacles and no patient used spectacles for distance vision, even while driving at night. No patient complained of severe glare or double vision. No patient found it difficult to adaption of the new binocular vision after treatment. The satisfaction scores of each item have no significant differences between two groups at 6 months after surgery.
| LBV group | PresbyMAX group | P* | |||||
| Scale | Preoperative | Postoperative | P** | Preoperative | Postoperative | P** | |
| Near vision | 40.83±30.13 (0 to 80) | 93.33 ± 7.17 (85 to 100) | .00 | 40.83±30.13 (0 to 80) | 93.75±6.81 (80 to 100) | .00 | .89 |
| Distance vision | 65±9.57 (50 to 80) | 92.5±7.5 (80 to 100) | .00 | 65.83±8.86 (50 to 85) | 90±9.35 (80 to 100) | .00 | .50 |
| Intermediate vision | 69.17±9.54 (60 to 90) | 94.17±7.86 (80 to 100) | .00 | 67.5±10.90 (50 to 90) | 92.92±9.00 (70 to 100) | .00 | .73 |
| Night vision | 80.83±9.53 (60 to 90) | 85±10.99 (70 to 100) | .35 | 78.75±11.57 (60 to 90) | 82.92±11.08 (60 to 100) | .40 | .66 |
| §Dependence on glasses | 49.17±44.25 (0 to 100) | 0 | .00 | 52.50±40.03 (0 to 100) | 0 | .00 | - |
| Satisfaction with correction | 47.5±22.03 (0 to 60) | 93.33±5.53 (80 to 100) | .00 | 45.83±21.47 (0 to 60) | 91.25±6.50 (80 to 100) | .00 | .43 |
| *Questionnaire included scales ranging from 0 to 100,where 0 induced not at all satisfied and 100 indicated completely satisfied;§0 indicated have no need glasses and 100 indicated completely depend on glasses. *P represents that data were compared between two groups postoperatively, **P represents that data were compared in the same group from pre- to post-operation, All values are presented as mean ± standard deviation (range). LBV group: underwent LASIK with an aspheric ablation profile using the MEL 80 excimer laser,PresbyMAX group:underwent presbyLASIK with a biaspheric multifocal ablation profile using an AMARIS 750S excimer laser. | |||||||
Table 5: Postoperative Patient Satisfaction Scores pre- to post-operation*
Discussion
LBV and PresbyMAX are two different techniques for presbyopia correction using different laser platforms, but both of them combine micro-monovision and spherical aberration induced by reshaping corneal asphericities. At 6 months after surgery, the monocular uncorrected distance visual acuity and binocular uncorrected intermediate visual acuity and uncorrected near visual acuity improved in both groups, and the degree of safety and predictability was high. We analyzed different intermediate distances visual acuities, which were 63cm for computer using and 100cm for cooking or playing mahjong. The significant improved postoperative uncorrected intermediate visual acuity and the increased satisfaction scores about intermediate vision in both groups demonstrated that good intermediate binocular vision performances achieved although combined monovision in both techniques. The residual accommodation left due to patient age of 51 or younger at the time of treatment might partly interfere and support intermediate and near vision tasks. But all patients suffered from presbyopic symptoms before surgery and were complaining about their near vision abilities. Six-month after surgery, the complaint of reduced near vision performance is minimum or even not existing. One reason could be the increased of the depth of field to induce the so-called pseudo-accommodation which provides functional near vision by non-accommodative factors. [10] Nonetheless, the amount of pseudo-accommodation alone would not be enough for “spectacle-free” functional near vision. The micro-monovision portion with myopic target is of additional help for sufficient near vision.
In fact, monovsion is still a regular and effective choice for presbyopia correction, which can be archived by IOLs, contact lens or laser ablations. [11-13] But the anisometropia induced by monovision is hard to adapt for some patients. LVB and PresbyMAX both decrease anisometropias which were 1.35±0.35 (0.75 to 1.88) and 0.80±0.41 (0.38 to 1.63) at six months after treatments in our study. In the current study, no patients said “find it difficult to adapt” during whole period of following up. The near stereoacuity was significantly improved rather than being worse postop¬eratively. This may be due to near vision improvement after surgery. However distance stereoacuity degrade to subnormal levels in both groups. Thus, the limitation of micro-monovi¬sion is still the influence on stereoacuity. The acceptance of the very little anisometropia should be preoperatively tested and had to be tolerated by the patient to remain a study candidate. The potential unwanted outcomes should be explained to the patients and noted in the informed consent.
Despite spherical aberrations (SA) induced in both techniques, a compromise in night vision could not be found at 6 month after surgery in both groups. Furthermore, previous literature reports of multifocal ablation profiles showed slightly decreased contrast sen¬sitivity under photopic and mesopic conditions [6, 7] which our results confirm. For both groups, at 1 month or 6 months follow-up, the changes in binocu¬lar contrast sensitivity from the preoperative values in all test conditions were not significantly different at any frequency. However, a more severe drop of contrast sensitivity (CS) threshold for PresbyMAX was observed, especially under mesopic lighting condition. These may be due to pupil dilation under mesopic lighting condition. Pupil size and dynamics which may often play an additional role for good vision at all distances and thus, patient satisfaction in multifocal cornea ablation designs.
Some previous presbyLASIK studies indicated that clinical outcomes of multifocal corneal ablation designs are less predictable and at higher risk than those for other corneal modalities, such as monovision or LBV. [2, 14] But our results look better than those of other researches in cornea multifocal excimer laser field to alleviate presbyopic symptoms [6, 7] and seem to be compared favorably with the results of other micro-monovision treatments. [3, 8]
In both two groups, no retreatment was requested and no patient asked to reverse the intended micro-monovision design for better distance vision during the 6 month of following-up. 100% of patients achieved both 20/25 or better uncorrected distance visual acuity and J5 or better uncorrected near visual acuity at the 6 month follow-up visit. In our cohort, four eyes loss of one line corrected distance visual acuity after surgery and no eyes lost 2 lines, most of them have no change or gain one line of corrected distance visual acuity from pre to post operation.
The limitation of our study was that most patients in this study with moderate myopia with low astigmatism and this relatively young presbyopic group partly results in good performance for near vision acuity. Nevertheless, 40 to 45 years old people are still the most common population who are considering cornea laser ablation for refractive errors in China, so there are no enough aged presbyopic patients with refractive errors were enrolled during our study period and analyzed efficacy and safety of presbyopic treatments in this group possibly have more clinical values for cornea refractive surgeon. Our results bases on a 6-month clinical follow-up, however, presbyopia continues to progress with age. Our study included myopic presbyopes of up to 51 years of age, i.e. most of patients were of young presbyopic age, although there was no upper age limit in the study protocol. Therefore, a longer follow-up could shed light on the durability of (near) performance during further degradation of accommodation.
In conclusion, the aspheric micro-monovision LASIK (LBV) and hybrid bi-aspheric multifocal central presbyLASIK treatments were both safe and effective for correction of presbyopia and myopic astigmatism. There were no statistically significant differences in visual acuities and visual performances. Thus, for presbyopia with or without astigmatisms correction, multifocal central presbyLASIK treatment gave visual and refractive results comparable to those by the aspheric micro-monovision LASIK (LBV). We suggest that choose one of them is a safe alternative when another is not available.
Conflict of Interest: No conflicting relationship exists for any author. The authors state that they have no proprietary interest in the products named in this article.
References
- Davidson RS, Dhaliwal D, Hamilton DR, et al. (2016). Surgical Correction of Presbyopia. Journal of cataract and refractive surgery 42: 920-30.
- Vargas-Fragoso V, Alio JL. (2017). Corneal Compensation of Presbyopia: Presbylasik: An Updated Review. Eye and vision 4:11.
- Reinstein DZ, Archer TJ, Gobbe M. Lasik for Myopic Astigmatism and Presbyopia Using Non-Linear Aspheric Micro-Monovision with the Carl Zeiss Meditec Mel 80 Platform. Journal of refractive surgery (2011) 27:23-37.
- Ruiz LA, Cepeda LM, Fuentes VC. (2009). Intrastromal Correction of Presbyopia Using a Femtosecond Laser System. Journal of refractive surgery 25: 847-54.
- Baudu P, Penin F, Arba Mosquera S. (2013). Uncorrected Binocular Performance after Biaspheric Ablation Profile for Presbyopic Corneal Treatment Using Amaris with the Presbymax Module. American Journal of Ophthalmology 155: 636-47.e1.
- Luger MH, Ewering T, Arba-Mosquera S. (2013). One-Year Experience in Presbyopia Correction with Biaspheric Multifocal Central Presbyopia Laser in Situ Keratomileusis. Cornea 32: 644-52.
- Luger MH, McAlinden C, Buckhurst PJ, et al. (2015). Presbyopic Lasik Using Hybrid Bi-Aspheric Micro-Monovision Ablation Profile for Presbyopic Corneal Treatments. Am J Ophthalmol 160: 493-505.
- Zhang T, Sun Y, Weng S, et al. (2016). Aspheric Micro-Monovision Lasik in Correction of Presbyopia and Myopic Astigmatism: Early Clinical Outcomes in a Chinese Population. Journal of refractive surgery 32: 680-5.
- Waring GO, 3rd. (2000). Standard Graphs for Reporting Refractive Surgery. Journal of refractive surgery 16: 459-66.
- Torricelli AA, Junior JB, Santhiago MR, Bechara SJ. (2012). Surgical Management of Presbyopia. Clin Ophthalmol 6:1459-66.
- Goldberg DB. (2001). Laser in Situ Keratomileusis Monovision. Journal of cataract and refractive surgery 27: 1449-55.
- Levinger E, Trivizki O, Pokroy R, et al. (2013). Monovision Surgery in Myopic Presbyopes: Visual Function and Satisfaction. Optom Vis Sci 90:1092-7.
- Miranda D, Krueger RR. (2004). Monovision Laser in Situ Keratomileusis for Pre-Presbyopic and Presbyopic Patients. Journal of refractive surgery 20:325-8.
- Arba Mosquera S, Alio JL. (2014). Presbyopic Correction on the Cornea. Eye and vision 1:5.
Citation: Fang Liu MD., et al. (2019). Laser Blended Vision versus PresbyLASIK for Correction of Presbyopia and Myopic Astigmatism. Journal of Ophthalmology and Vision Research 1(2).
Copyright: © 2019 Fang Liu MD., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
