Research Article
Volume 1 Issue 1 - 2019
Birth Trauma and Compensatory-adaptive Mechanisms at the Head Configuration (Molding)
Doctor of Medical Sciences, Professor, WHO expert, and full member of the European Academy of Natural Sciences
*Corresponding Author: Vlasyuk vasily, Doctor of medical sciences, professor, WHO expert, and full member of the European Academy of Natural Sciences.
Received: October 16, 2019; Published: October 25, 2019
Abstract
Compensatory-adaptive changes from the side of the skull and brain of the fetus, which provide a physiological configuration, are presented. The types of pathological configuration of the head are distinguished when the pathology of the brain develops. The relationship of head compression in childbirth with changes in heart activity is considered.
Keywords: Birth trauma; Compression hypoxia; Compression of the head; Configuration (molding); Compensatory and adaptive mechanisms
Introduction
In the world science and practice, there are 4 basic ideas about birth trauma (BT): 1) Birth trauma as a disease in the fetus and newborn baby that occurs under the influence of mechanical forces during childbirth, 2) Birth traumatic injuries in the fetus and mother that occur during childbirth, 3) Damage to the brain of the fetus of a hypoxic-ischemic nature caused by compression of the head during childbirth, and 4) Psychological shock in the mother and stress in the fetus caused by labor. All these are objectively existing different approaches to one big problem - birth trauma. It is important to separate them among themselves. Birth trauma [1] as a disease is accompanied by significant mechanical damage that leads to a systemic reaction of the body and can lead to death. Birth traumatic injuries (caput succedaneum, small hemorrhages in various structures, etc. [1]) are not accompanied by a general reaction of the body and are associated pathological processes. When head compression occurs in the birth canal, ischemia and hypoxia of brain tissue can occur, this condition can be called “compression hypoxia” (CH) [2]. BT and CH are diseases, nosological forms, and birth injuries are local pathological processes, concomitant conditions. Birth shock (psychological shock) and mental changes associated with childbirth are widely reported in the literature [3-5].
To understand the mechanism of all the consequences of birth trauma, it is important to know the compensatory-adaptive changes in the fetus and mother, allowing to prevent the adverse effects of childbirth. These mechanisms are poorly understood. An example of this is the existence of the notion that cerebrospinal fluid in infants flows, as in adults, through arachnoid villi into the superior sagittal sinus [6]. If this were the case, then most children would be born with ruptured meninges, massive intracranial hemorrhages. In fact, fetuses and newborns do not have such villi connected to the dura mater, therefore, cerebrospinal fluid cannot flow into the superior sagittal sinus [1]. The structure of the skull, brain and its structures in the fetus is such that it can safely pass through the birth canal without injury. After birth, there is a significant restructuring in the tissues of the head and brain of the child, aimed at adapting to extrauterine life.
Similar evolutionary devices are known in wildlife. For example, a tooth at the end of the upper jaw of a crocodile hatching from an egg, which is necessary for breaking through the egg shell and which disappears shortly after birth. The mobility of the bones of the skullcap, long bridging veins (up to 4 cm), fluid in the subdural space of the human fetus - all these are evolutionary devices necessary for the normal course of the birth act. In an adult, the cranial bones are fused, the bridging veins are significantly shortened, fused with the dura mater and have almost no free part, there is no fluid in the subdural space, there are arachnoid villi, etc. In an adult, the need for adaptations important for the birth process disappears.
The configuration of the fetal head is not well understood. Configuration (molding) is the most important evolutionarily physiological compensatory-adaptive process in childbirth. This is a complex process of adaptation of the tissues of the head and brain of the fetus to the birth canal of the mother. The configuration helps to prevent the adverse effects of labor on the fetus and mother. The configuration consists of a series of successive changes in the fetus, it is associated with the activity of the heart and all systems of the fetus. All adaptation mechanisms have boundaries, the overcoming of which leads to pathological changes. Controlling adjective changes can help prevent ?? in a child.
The purpose of the work is to study the compensatory-adaptive changes in the fetus. The work is based on the results of our own morphological studies of the skull and brain.
Results and Discussion
Compensatory-adaptive changes that ensure the configuration of the head include:
- Displacement (overlapping) of the skullcap bones during the configuration of the head, their overlapping at the sutures [1];
- the presence of a subdural exudate (fluid) in the subdural space, providing equalization of pressure on the surface of the brain during configuration of the head and gliding of the cerebral hemispheres along the dura mater during their movement;
- The absence of arachnoid villi and cerebrospinal fluid outflow into the sinuses, which would prevent gliding between the arachnoid and dura mater;
- The presence of long bridging veins, which ensure the outflow of blood from the surface of the brain to the sinuses during movements of the cerebral hemispheres (Fig. 1);
- The presence of a cross view of the overlapping of bones, preventing excessive displacement of the bones of the skull during the configuration of the head [7];
- immaturity of the cortex and the absence of myelination of the white matter of the cerebral hemispheres, which ensure the plasticity of the brain and the change in its shape during the configuration of the head;
- the presence of long Schlesinger anastomosing veins, which ensure the outflow of venous blood from the cortex and superficial cerebral veins into the system of internal cerebral veins (with narrowing of the superior sagittal sinus, with pressure of the bones of the skull on the cerebral hemispheres);
- The movement of blood from the external cerebral veins, from the veins of the periosteum to the epidural cerebral veins;
- The presence of well-developed vertebral epidural venous plexuses that ensure the outflow of blood from the brain into the lower and upper vena cava. An increase in venous outflow from the brain through the vascular plexuses of the vertebral canal.
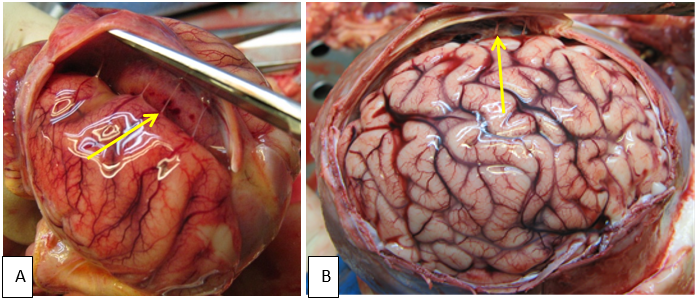
Figure 1: Differences in the length of bridging veins (arrows) in children of different ages:
A - long bridging veins in a premature newborn, B - bridging veins in a child of 4.5 months.
A - long bridging veins in a premature newborn, B - bridging veins in a child of 4.5 months.
The configuration is mainly ensured by (1) mobility of the bones of the skullcap, (2) the presence of a subdural exudate, (3) the absence of arachnoid villi and the outflow of cerebrospinal fluid into the sinuses, and (4) the presence of long bridging veins that provide blood flow in the brain substance during brain mass movements inside the skull. When configured, the bones of the skullcap overlapping to each other. The falx and tentorium cerebelli prevent excessive bone overlapping and compression of the brain.
These structural devices prevent the development of cerebrovascular accidents during compression of the head and its configuration. Thanks to these devices, a child can be born without hypoxia during a prolonged or quick birth, with a cephalopelvic disproportion, with the use of obstetric forceps and other complications of childbirth. However, all adaptive mechanisms have their own limits of compensation, beyond the boundaries of which damage and hypoxia of brain tissue occur.
The configuration (molding) can be physiological and pathological, and pathological is divided (Figure 2) into three types - excessive (pronounced), rapid and asymmetrical [8]. The configuration can become pathological when using obstetric forceps and a vacuum extractor. The pathological configuration leads to both birth trauma and compression hypoxia of the brain [2]. The physiological configuration is not accompanied by brain damage, and the pathological leads to this lesion. The pathological configuration is a deviation from the normal physiological process and is associated with complications of childbirth (cephalopelvic disproportion, rigidity of the birth canal, large sizes of the head, contracted pelvis, rapid parturition, asynclitic entry of the head into the pelvis, obstetric benefits, the application of obstetric forceps, etc.). It is accompanied by various ruptures, subdural and leptomeningeal hemorrhages and other disorders of cerebral circulation.
With an excessive configuration, the tensile strength of various structures of the skull and brain becomes such that various tears and hemorrhages occur (with strong contractions of the uterus, during labor stimulation, contracted pelvis, application of obstetric forceps, squeezing out the fetus etc.). The tension force of the falx and tentorium cerebelli begins to exceed their strength, which leads to rupture of structures. First of all, the tentorium cerebelli is tearing, as it is almost twice less durable than falx. Before ruptures, intradural hemorrhages can occur. A rupture of the cerebellar tentorium leads to subdural hemorrhage and often to the death of the child. With strong pressure on the parietal bones, the cerebral hemispheres are significantly displaced, bridging veins are stretched. First, the inflows of the bridging veins rupture, which leads to subarachnoid and subpial hemorrhages, and then the veins themselves rupture, which leads to subdural hemorrhages. With significant bone overlapping, there is strong pressure on the brain primarily in the areas of overlapping (sutures), the formation of impressions in it in the form of steps, rupture of blood vessels, subarachnoid and intracerebral hemorrhages. Other changes characteristic of birth trauma also occur.
A rapid configuration occurs during rapid parturition and precipitated labor, oxytocin stimulation, the use of obstetric forceps or a vacuum extractor, with pelvic presentation, with the desire to quickly complete the birth in the interests of the mother or fetus. In these cases, various compensatory-adaptive mechanisms do not have time to develop, the blood circulation in various structures does not have time to rebuild, the fetus does not have time to change the position of the head, etc. Structures can withstand gradually developing tension, but break when the same force acts for a short period of time. With an increase in uterine activity, utero-placental blood circulation decreases and skull compression [9] is become stronger.
An asymmetric configuration often occurs when the head is inserted asynclitically. Small asynclitism (physiological) is characteristic of normal childbirth and is associated with small lateral movements (declination) of the head in the birth canal. With a contracted pelvis, with a cephalopelvic disproportion, with stimulation of childbirth, etc., declination of the head becomes pathological (pathological asynclitism). In this case, the tension force of the two halves of the tentorium cerebelli becomes different and focuses on one half, which leads to a rupture. If the head were inserted synclitically, then with the same degree of configuration, the tension force would be distributed evenly over the two halves of the tentorium cerebelli and no rupture would occur. It is with the asymmetric configuration of the head that many cases of birth injury are associated, since ruptures of the tentorium cerebelli are most often unilateral.
The above explanations follow from the pattern I discovered about the correlation between the region of periosteal congestion of the skullcap and the localization of tentorium cerebelli tears [1, 8]. It is this regularity that only now allows us to explain the long-discovered fact that those born in the 2nd position have a found significantly higher performance than Verbal IQ's [10]. Given this pattern, at the 2nd position, the right half of the cerebellar tentorium is most often damaged, right-sided subdural hemorrhages occur, and more damage the right hemisphere of the brain, which is more responsible for performance functions than for speech.
Three degrees of head configuration are distinguished [11]: 1 degree (+1) - the edges of the skull bones move in the area of the sutures, can touch, but do not overlap, 2 degree (+2) - the bones come on each other, but can easily shift in the opposite direction, 3grade (+3) - the bones come on top of each other, but even with pressure from the finger the hands do not go back; the entry process can progress. The absence of bone displacements is considered as a zero stage. These data are entered in the partogram. When studying the configuration, the diameters of the skull are determined; coefficients and indices are extracted from the data on measurements of the skull [12, 13].
The degree of configuration can be determined in another way [1]: 1 degree (light) - overlapping of bones over one of the sutures, 2 degree (moderate) - overlapping of bones over 2-3 sutures, 3 degree (pronounced) - overlapping of bones over 4 -5 sutures. Clinical studies have shown that with the second and third degrees of the configuration of the head, early deceleration is observed: with the 2nd degree, the appearance of early decelerations, and with the 3rd degree, the appearance of early and sporadic decelerations [14]. Mild and moderate configurations do not lead to pathological changes, but a severe (pathological) degree leads to compression hypoxia of the fetal brain and birth injury. What are the differences between CH and BT? Both conditions are due to the impact on the skull of mechanical forces. However, unlike CH in BT, various tissue breaks occur, accompanied by hemorrhages. This usually occurs when the compression force exceeds that which occurs with C?.
It has been established that with an increase in the degree of configuration, the frequency of subdural, leptomeningeal and intraventricular hemorrhages, as well as periventricular leukomalacia increases [1]. Thus, in order to understand the cause of birth injury, it is important to know the compensatory-adaptive mechanisms that overcome traumatic injuries. So, with the configuration of the head, tension occurs in two halves of the tentorium cerebelli, at first there are intradural hemorrhages in it, and only then tears occur in it, often leading to fatal intradural hemorrhages. Therefore, for the prevention of ruptures, it is important to prevent the pathological configuration of the head.
When the head is compressed, venous outflow of blood from the tissues of the head, skull and brain is disturbed, a decrease in cerebral blood flow, hypoxia and acidosis of the brain tissue occur, leading to damage to brain cells. Various compensatory-adaptive mechanisms begin to act in the fetal body: an increase in heart rate, an increase in cardiac output, an increase in blood pressure, an intensification of metabolic processes, a transition to economically more beneficial anaerobic glycolysis, an increase in blood levels of cortisol and catecholamines, and centralization of blood circulation in the fetus etc. If there are no violations in the uteroplacental and umbilical cord blood circulation, then a condition (CH) may develop in which it is the brain that suffers from hypoxia, and the internal organs receive a sufficient amount of oxygen. In experimental studies, the development of such a state in animal fetuses has been proved [15-17]. CH is a type of intranatal hypoxia in which hypoxic-ischemic damage occurs mainly in the brain due to compression of the head. CH is simultaneously a type of birth injury with a predominantly hypoxic-ischemic brain damage due to compression of the head during childbirth. Children who survived CH develop “compression hypoxic-ischemic encephalopathy” [18, 19].
In spontaneous labor in the configuration process, due to the need to adapt the fetal head to the size and shape of the birth canal of the mother, a compression of the fetal head occurs. The pressure on the fetal head from the side of the pelvis in childbirth is 120-250 (sometimes reaches 510) mm Hg. [18, 20]. The configuration process involves many compensation mechanisms, the failure of which leads to brain damage. In addition, other causes that compress the skull may act during childbirth: obstetric forceps, vacuum extractor, benefits, external pressure on the uterus, and others. Two effects occur under the influence of these physical factors: 1) cerebrovascular accident with hypoxic-ischemic brain damage and 2) birth traumatic injuries. When the head is compressed, intracranial pressure rises, cerebral blood flow and oxygen content decrease in the brain [11, 22], and in response to an increase in intrauterine pressure more than 100 mm Hg bradycardia develops. Due to compensatory mechanisms, intracranial pressure fluctuates within certain limits (12–20 mm Hg) and can stabilize [23], but with significant compression of the skull it can rise again and lead to death. The fetus of a dog in an experiment dies at an intracranial pressure of 18 mm Hg or higher [15].
An increase in the degree of configuration of the head leads to traumatic and hypoxic injuries. With an excessive configuration of the head, compression hypoxia of the brain first occurs, which then passes into birth trauma (Figure 3). BT and CH can be differentiated depending on the nature of the damage.

Figure 3: The relationship between excessive head configuration with compression hypoxia and birth trauma.
With an increase in skull compression, blood pressure rises, the heart rate decreases, and the load on the heart increases. Each fight is accompanied by this adaptive mechanism [24, 25]; with bradycardia, diastole lengthens, blood flow to the heart increases, the minute volume of blood increases, which leads to a certain restoration of impaired blood supply caused by compression of the skull. In the period between contractions, the fetal heart rate is restored. If bradycardia lasts between contractions (or tachycardia develops), this indicates a breakdown of the compensation mechanism, persistent tissue ischemia, and cardiac failure. Then there is a drop in blood pressure, the blood circulation in the placenta decreases, general hypoxia and hypoxemia progresses, hypoxic-ischemic brain damage increases. Therefore, compression hypoxia of the brain leads to general fetal hypoxia.
Bradycardia also develops with compression of the umbilical cord, its vessels separately, and even with compression of the internal iliac artery (in experimental studies [26]). It also leads to increased blood pressure, lengthening the period of diastole, the development of hypoxia and acidosis in the blood of the fetus. In fact, any difficulties with blood circulation in the placenta-fetus system (through the brain and head tissues, through the great vessels, through the umbilical cord vessels) lead to a similar reaction from the heart and the development of bradycardia.
With BT, damage characteristic of CH may be present. However, with CH there should be no damage characteristic of BT. Based on the clinical and morphological diagnosis of the lesions in question, it is possible to establish objectively diagnoses of BT and CH, as well as conduct their differential diagnosis.
Conclusion
Thus, the fetus during childbirth is protected from compression in the birth canal by compensatory-adaptive changes of an evolutionary nature. Some of these devices are found in the skull and in the brain and are manifested by a process such as configuration. The configuration can be physiological and pathological, and pathological is divided into excessive, fast and asymmetric. In addition, I distinguish three degrees of configuration. Compression of the head with circulatory disorders in it leads to an increase in blood pressure, bradycardia, and an increase in systolic ejection of blood from the heart, and normalization of the blood supply to the brain. Prolonged and excessive compression of the head can lead not only to various ruptures, intracranial hemorrhages (BT) and hypoxic-ischemic lesions of the brain, but also to dysregulation of the heart, heart failure and general fetal hypoxia. To prevent damage to the brain in the fetus, it is important to diagnose the configuration during childbirth.
References
- Vlasyuk VV. (2019). Birth Trauma and Perinatal Brain Damage. Springer International Publishing, Springer Nature Switzerland AG.
- Vlasyuk VV. (2019). Compression Circulatory Hypoxia of the Brain as a Type of Intrapartum Hypoxia. J Gynecol.
- Emerson WR. (1998). Birth Trauma: The Psychological Effects of Obstetrical Interventions. Journal of Prenatal and Perinatal Psychology & Health 13:11-44.
- Taghizadeh Z, Irajpour A, Nedjat S, Arbabi M, Lopez V. (2014). Iranian mothers’ perception of the psychological birth trauma: A qualitative study. Iranian J Psychiatry 9: 31-36.
- Roberts NP, Roberts PA, Jones N, Bisson JI. (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review. 38: 25–38.
- Barashnev YuI. (2011). Perinatal neurology. Second edition, supplemented. M: Triad -H.
- Vlasyuk VV. (2018). Configuration (molding) of the fetal head during labor and related issues. Neurol Neurosci Rep. 1(2): 1-2
- Vlasyuk V.V. (2009). Birth Trauma and perinatal cerebrovascular circulation disorder. St. Petersburg: Nestor-History.
- Simpson KR. (2011). Assessment and Optimization of Uterine Activity during Labor. Clin Obs Gyn 54: 40-49.
- Willerman L. (1970). Fetal head position during delivery and intelligence. In: Physical Trauma as an Etiologial Agent in Mental Retardation. Ed: C.R.Angle and E.A.Bering. Washington 105-108.
- Sorbe B. (1983). Dahlgren S. Some important factors during vaginal delivery are a photographic study. Int J Gynaecol Obstet. 21(3): 205-12.
- Fang Pu, Liqiang Xu, Deyu Li, et al. (2011). Effect of different forces on fetal skull molding. Medical Engineering and Physics. 33(5): 620–625.
- Kriewall, TJ, Stanley JS, McPherson GK. (1977). Neonatal head shape after delivery. Journal of Perinatal Medicine. 5: 260-267.
- Mochalova M.N., Ponomareva Yu.N., Mudrov V.A. (2015). Features of the configuration of the head at birth large fruit. Modern problems of science and education 3.
- Zirakadze AN, Kintraya PYa. (1983). Experimental analysis of the value of methods for monitoring the functional state of the fetus during labor. On Sat scientific Proceedings of the Research Institute of Perinatal Medicine, Obstetrics and Gynecology of the Ministry of Health of the Georgian SSR. Tbilisi. 3-9.
- Mann LI. (1971). The Effect of Head Compression on FHR. Brain Metabolism and Function. Obstet Gynecol 39: 721-726.
- O’Brien WF. (1984). Effect of Cephalic Pressure on Fetal Cerebral Blood Flow. Am J Perinatal 1(3): 223-226.
- Lindgren L. (1977). The influence of pressure upon fetal head during labor. Acta Obstet Gynecol Scand. 56(04): 303-309.
- Schifrin BS, Deymier PA, Cohen WR. (2014). Cranial compression ischemic encephalopathy: fetal neurological injury. In: Stress and Developmental Programming: Beyond Phenomenology. Hauppauge, NY: Nova Scientific Publishers. 651–688.
- Antonucci MC, Pitman MC, Eid T, et al. (1997). Simultaneous monitoring of head-to-cervix forces, intrauterine pressure and cervical dilatation during labor. Med Eng Phys. 19(4):317-326.
- Aldrich CJ, D'Antona D, Wyatt JS, et al. (1994). Fetal cerebral oxygenation can be measured at near-infrared spectroscopy. Obstet Gynecol. 84: 861-866.
- Peebles DM, Spencer JA, Edwards AD et al. (1994). Relation between human and cerebral oxygen saturation of the spectrum studied in laboratories. Br J Obstet Gynaecol. 101:44–48.
- Heyborne KD. (2017). A Systematic Review of the Intrapartum Fetal Head Compression: What is the Impact on the Fetal Brain? AJP Rep. 7:79-85.
- Gutner MD. (1958). Intranatal asphyxia. Krasnoyarsk: Krasnoyarsk Medical Institute.
- Halpern RC. (2014). Intrapartum Pathways to Neonatal Neurologic Injury – A Lawyer’s View. OTLA Medical Malpractice Conference.
- Evers JLH, De Haah J, Jongsma HW, et al. (1981). The preejection period of the fetal cardiac cycle. Europ. J. Obstet. Gynecol 11: 401-433.
Citation: Vlasyuk vasily. (2019). Birth Trauma and Compensatory-adaptive Mechanisms at the Head Configuration (Molding). Journal of Gynaecology and Paediatric Care 1(1).
Copyright: © 2019 Vlasyuk vasily. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

