Conceptual Paper
Volume 1 Issue 2 - 2019
A Rule of Astigmatism in Pediatric Subluxated Crystalline Lens
Center for Pediatric Ophthalmology, Department of Ophthalmology, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
*Corresponding Author: Ran David MD PhD, Center for Pediatric Ophthalmology, Department of Ophthalmology, Hadassah-Hebrew University, Medical Center, POB 12000, Jerusalem 91120, Israel.
Received: October 06, 2019; Published: October 14, 2019
Abstract
Background: Crystalline lens subluxation leads to refractive error typically resulting in myopia and astigmatism. Repeated refraction is mandatory. Retinoscopy is challenging due to phaco/iridodonesis and distorted reflex. This study explored simplified rule of thumb to help determining the correct refraction. We postulated that the expected axis of astigmatism should be parallel to the direction of subluxation.
Methods: We performed a retrospective study of patients (<19 years old), with a subluxated crystalline lens who underwent lensectomy without intraocular lens implantation, at Hadassah University Medical Center between 1980 and 2016. Traumatic cases were excluded. In each case, the correlation between the axis of astigmatism and direction of subluxation was evaluated.
Results: Forty-three eyes were included. The average age was 67.40 (range 10 to 230) months. The average pre–op astigmatism (-3.90D, range -0.75 to -8.75D) was reduced significantly after lensectomy (-0.68D, range -0.5 to -2D). The average pre–op spherical equivalent (SE) was myopic (-5.93D, range -18.75 to +17D). In each direction the pre-op axis of astigmatism was found to be in 93.33% cases horizontal in superior; 76.92% oblique in superotemporal; 100% vertical in temporal; 100% oblique in infero-temporal; 100% horizontal in inferior; 100% vertical in nasal; 66.67% oblique in superonasal, subluxations. Totally, 86% of measured axis were inside those expected ranges in all directions.
Conclusion: We found a high correlation between the direction of subluxation and the astigmatic axis before surgery for pediatric lens subluxation. We postulate that the high and irregular astigmatism in subluxation is mainly lenticular. As a rule of thumb, the astigmatic axis is expected to be parallel to the direction of subluxation.
Introduction
Ectopia lentis (EL) is one of the most difficult situations for treatment in pediatric ophthalmology. EL includes any displacement or malposition of the crystalline lens irrespective of the cause. Lens malposition may occur from congenital or developmental conditions such as Marfan syndrome, homocystinuria, Ehlers-Danlos syndrome, hyperlysinemia, sulfite oxidase deficiency, simple ectopia lentis and congenital aniridia. It may also be acquired due to trauma (1).
Crystalline lens malposition usually causes a reduced visual acuity, the extent of which varies with the degree of lens displacement. This typically leads to refractive error, mainly myopia and astigmatism. Early diagnosis and effective correction of vision is critical to prevent amblyopia. Thus, repeated and accurate refraction is mandatory. Occasionally, retinoscopy is challenging due to phacodonesis, iridodonesis and a distorted reflex (2, 3).
This study explored a simplified rule of thumb to help determining the correct refraction in cases of crystalline lens subluxation. We postulate that the high astigmatism in subluxated lens is largely lenticular, therefore the expected axis of astigmatism should be parallel to the direction of lens subluxation.
Methods
We performed a retrospective study of pediatric patients (< 19 years old), with the diagnosis of subluxated crystalline lens who underwent lensectomy without intraocular lens implantation at Hadassah University Medical Center between 1980-2016. The study was approved by the institutional review board.
We collected the refraction including sphere, astigmatism and its axis and spherical equivalent (SE) before and after lensectomy. Direction of lens subluxation was assessed only if was clearly depicted by the treating physician in the medical file. Direction of lens subluxation was divided into 8 categories (superior; superotemporal; temporal; inferotemporal; inferior; inferonasal; nasal and superonasal subluxations) according to the main direction of lens displacement. Cases with traumatic etiology, missing data or unclear description of subluxation direction were excluded. In each case, the correlation between the axis of astigmatism and direction of subluxation was evaluated. All children underwent cycloplegic refraction by retinoscopy by a certified pediatric optometrist and a comprehensive eye exam by a senior pediatric ophthalmologist.
We postulated that the astigmatism in subluxated lens is mainly lenticular in nature. Therefore, we expected that there should be a high correlation between the direction of lens subluxation and axis of astigmatism. We suggested that the axis of astigmatism is parallel to the direction of subluxation. We defined a range of ± 30 degrees from expected axis as a tolerated error (Figure 1).
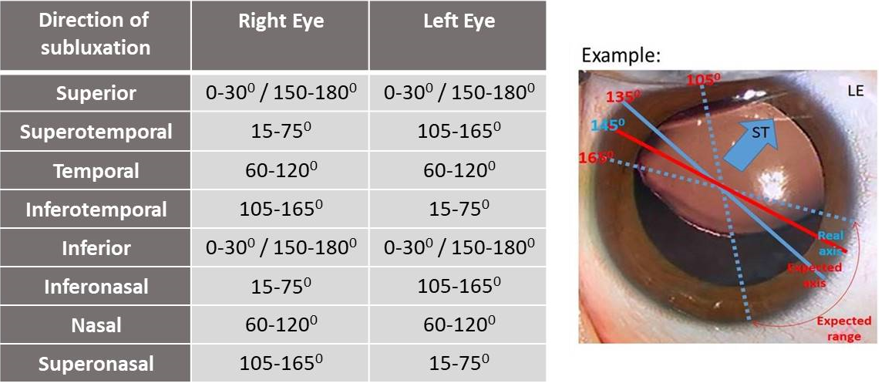
Figure 1: Expected axis of astigmatism according to direction of subluxation. On the right, an example of a case of a left eye (LE) with superotemporal (ST) lens subluxation. Thus, the expected astigmatism should be found in 135±30° (The expected range of astigmatism axis is 105-165°). The actual pre-op axis of astigmatism was 145° and found to be within the expected range of astigmatism axis.
Statistical analysis
Statistical analysis performed using T-test, Fisher`s exact test and Pearson Chi-square test. P value less than 0.05 were considered statistically significant.
Statistical analysis performed using T-test, Fisher`s exact test and Pearson Chi-square test. P value less than 0.05 were considered statistically significant.
Results
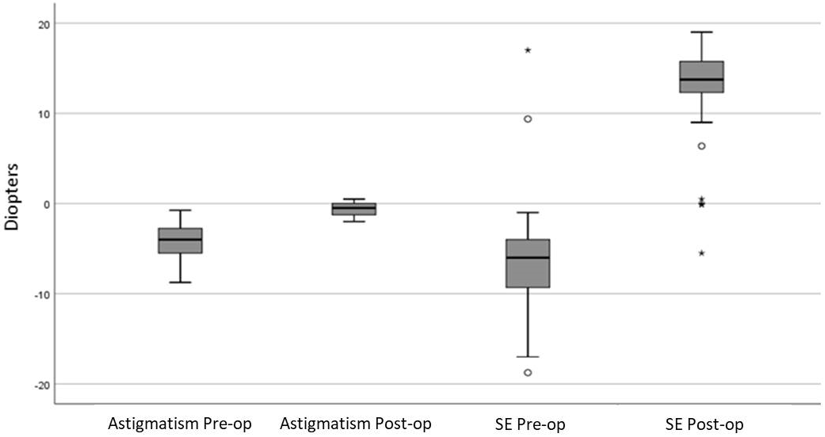
Forty-three eyes were included. Eighteen were left eyes and 25 were right eyes. Twenty-four were boys and 19 girls. The average age was 67.40 (range 10 to 230) months. The average pre–op astigmatism (-3.90D, range -0.75 to -8.75D) was reduced significantly after lensectomy (-0.68D, range -0.5 to -2D), (P-value< 0.001). The average pre-operative SE was myopic (-5.93D, range -18.75 to +17D) and after surgery it was +12.46D (range -5.5 to +19D) mainly due to post-operative aphakia (P-value< 0.001) (Figure 2).
In each direction the pre-operative axis of astigmatism was found to be in 93.33% cases horizontal in superior; 76.92% oblique in superotemporal; 100% vertical in temporal; 100% oblique in inferotemporal; 100% horizontal in inferior; 100% vertical in nasal; 66.67% oblique in superonasal, subluxations. Totally, 86% of measured axes were within the expected ranges in all directions of subluxation (Figure 3 and Figure 4).
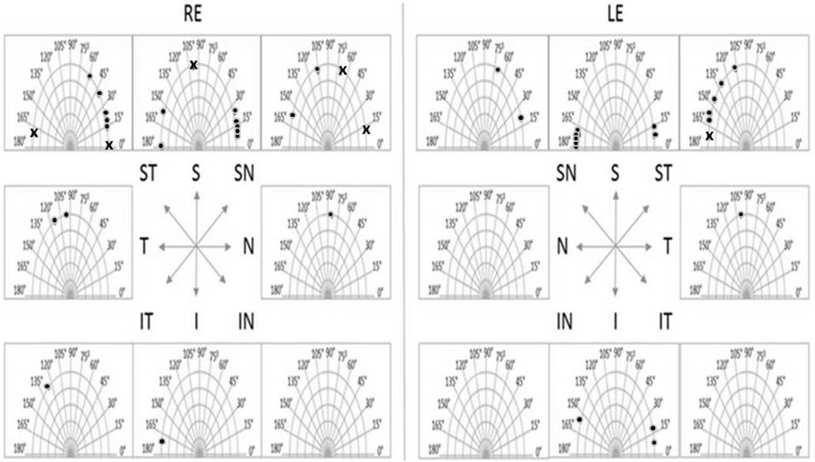
Figure 3: Pre-op axis of astigmatism according to direction of lens subluxation, in each eye. Dots represent cases within expected axis range of astigmatism. X sign represent exceptional values.
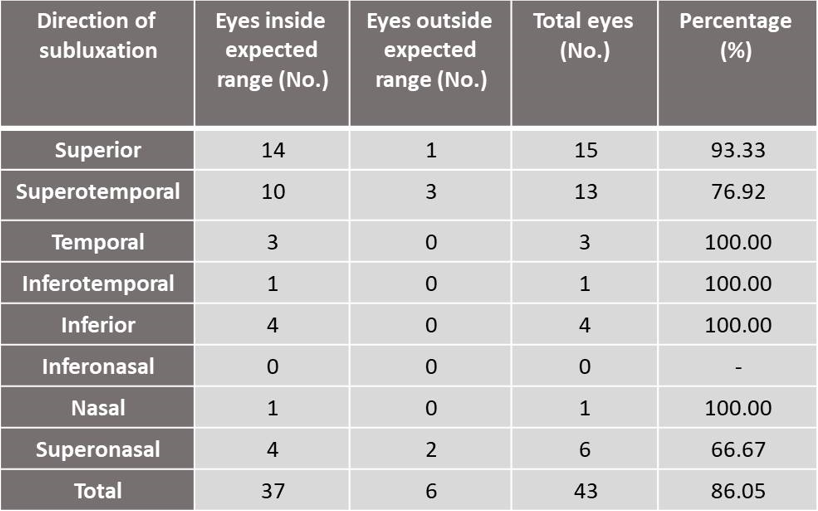
Figure 4: Distribution of eyes within expected axis range of astigmatism according to direction of subluxation.
Discussion
Children and young adults with EL are best managed by repetitive and careful refractions. In this particular population, not achieving satisfactory refractive measurements can lead to amblyopia. Often, retinoscopy is challenging due to phacodonesis, iridodonesis and a distorted reflex (2, 3). In this study we explored simplified rules of thumb to help determine the correct refraction in those complicated cases.
It is highly probable that eyes with EL will have high lenticular astigmatism due to displacement of the lens from its natural optical axis (4). Therefore, we postulated that the axis of astigmatism should be in high correlation to the direction of lens subluxation. Consequently, we expected that the axis of astigmatism is parallel to the direction of subluxation.
Our study shows a high correlation (86%) between the direction of subluxation and the astigmatic axis before surgery for pediatric lens subluxation. However, other studies suggested a high corneal astigmatism in cases with EL especially secondary to Marfan syndrome. Kinori M. et al, claimed that corneas of Marfan patients with EL are flatter and have a higher degree of corneal astigmatism (4). Same tendency of corneal flattening was found in other studies as well (5-7). Zang Y, in his study found also a positive correlation between age and corneal astigmatism in EL eyes. (7). Interestingly, those studies did not deliberate the lenticular astigmatism which definitely contributes considerably to the total astigmatism in EL. A main limitation of our study, except for its retrospective design, is that we did not have any measurement of corneal curvature or axial length. To overcome this limitation and to prove our assumption that astigmatism in EL is mainly lenticular, we compared cycloplegic refraction before and after extraction of the lens. We showed that the pre-operative astigmatism was reduced significantly after lensectomy. This finding emphasis the high influence of the lens itself on the total pre-operative astigmatism. Together with the high correlation between the direction of subluxation and the astigmatic axis we could confirm our assumption that the high astigmatism in EL cases are mainly lenticular.
In conclusion, we postulate that the high and irregular astigmatism in lens subluxation is largely lenticular. We suggest an easy rule of thumb, where the astigmatic axis is expected to be parallel to the direction of subluxation. This simplified rule can help determining the correct refractive error in children and young adults with subluxated lens and resultant challenging refraction.
Conflict of interest: No
References
- Hoffman, R.S., Snyder, M.E, Devgan, U., Yeoh, R. and Braga-Meie, R., (2013). Management of the subluxated crystalline lens. Journal of Cataract Refractive Surgery. 39(12): 1904-15.
- Guo, X., Mao, W., Chen, Y., Ma, Q., Zeng, L. and Luo, T., (1991). A clinical study and analysis of congenital lenticular dislocation (35 cases). Yan Ke Xue Bao. 7(4): 185-9.
- Neely, D.E. and Plager D.A., (2001). Management of ectopia lentis in children. Ophthalmol Clin North Am. 14(3): 493-9.
- Kinori, M., Wehrli, S., Kassem, I.S., Azar, N.F., Maumenee I.H., and Mets M.B., (2017). Biometry characteristics in adults and children with Marfan syndrome: from the Marfan eye consortium of Chicago. Am J Ophthalmol. 177: 144–9.
- Chen, J., Jing, Q., Tang, Y., Qian, D., Lu, Y. and Jiang, Y., (2018). Age differences in axial length, corneal curvature, and corneal astigmatism in Marfan syndrome with ectopia lentis. Journal of Ophthalmology. 2018: 1436834.
- Drolsum, L., Rand-Hendriksen, S., Paus, B., Geiran, O.R., and Semb, S.O. (2015). Ocular findings in 87 adults with Ghent-1 verified Marfan syndrome. Acta Ophthalmol. 93: 46–53.
- Zhang, Y., Jin, G., Young, C.A., Cao, Q., Lin, J., Lin J., Wang, Y., and Zheng D. (2018). Analysis of corneal astigmatism before surgery in Chinese congenital ectopia lentis Patients. Current eye research. 43(8): 972–6.
Citation: David Ran MD PhD., et al. (2019). A Rule of Astigmatism in Pediatric Subluxated Crystalline Lens. Journal of Ophthalmology and Vision Research 1(2). DOI: 10.5281/zenodo.3590475
Copyright: © 2019 David Ran MD PhD., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.