Mini Review
Volume 7 Issue 1 - 2025
Robotic Surgery in Eye Care: A Comprehensive Review
Hindu Rao Hospital and NDMC Medical College Delhi
*Corresponding Author: Escientific Publishers, Hindu Rao Hospital and NDMC Medical College Delhi.
Received: February 12, 2025; Published: March 03, 2025
Abstract
Robotic surgery represents an innovative frontier in ophthalmology, aiming to enhance precision, reduce surgical complications, and expand the potential for minimally invasive procedures. Despite promising advancements, widespread clinical integration remains limited due to technical, financial, and procedural challenges. This review synthesizes findings from two systematic analyses on robotic-assisted eye surgery, highlighting applications, benefits, limitations, and future directions. Key robotic platforms such as the Preceyes Surgical System and Da Vinci Surgical System are explored, along with their role in advancing surgical outcomes in vitreoretinal, orbital, and corneal procedures. Further, the article identifies the hurdles and opportunities in scaling robotic systems for routine clinical use.
Introduction
Ophthalmology is a field demanding unparalleled precision due to the delicate structures of the eye and its small surgical field. Advances in surgical technology, including robotic assistance, have emerged as potential solutions to overcome the limitations of human dexterity, particularly physiological tremors. Robotic systems, integrated with artificial intelligence (AI) and imaging technologies, promise to transform ocular surgeries by improving precision, safety, and ergonomics.
Despite these advancements, robotic surgery in eye care is still in its nascent stages, with limited adoption in clinical practice. This article reviews current robotic systems, their applications, and challenges in ophthalmology while discussing future innovations required for broader acceptance and integration.
History
The term "robotics" originates from the Czech word "robota," meaning "servant" or "worker." Karel ?apek introduced it in his play R.U.R. (Rossum’s Universal Robots), while Isaac Asimov later popularized the concept through his "Three Laws of Robotics," which defined fictional robotic behavior. [1,2] Initially, robots replaced workers in hazardous industrial tasks, such as car assembly, to reduce workplace injuries. In medicine, robotic systems enhance precision, reduce tremors, improve visualization, and enable remote surgical interventions.
Robots have assisted in surgeries for over 20 years. The first robotic surgery, using the Puma 560 robotic arm, was performed in 1985 for neurosurgical biopsies at Westinghouse Electric in Pittsburgh, Pennsylvania. Assisted by computed tomography (CT) the robot inserted a needle into the brain, demonstratin precision in minimally invasive surgeries. In 1988, the Probot was developed to assist with transurethral prostate resections [3] at Imperial College in London. It had four movable axes and a fast-rotating blade. [3,4] Computer Motion, started in 1989, became a top provider of surgical robots as their Automated Endoscope System for Optimal Positioning (AESOP) robotic arm got FDA approval in 1994, making it the first telepresence surgical robot. AESOP evolved into the ZEUS system with three remotely controlled arms. In the early 1990s, Integrated Surgical Solutions and IBM developed ROBODOC®. It was used for hip replacements in 1992. [4] In 1999, Intuitive Surgical launched the da Vinci "Standard" surgical robot. Robotic surgery is now used across multiple fields, including cardiac, digestive, gynecological, and neurosurgical procedures. It is also being explored in head and neck cancer surgeries, showing promising outcomes. [4]
Overview of Robotic Systems in Ophthalmology
Robotic Surgery in Ophthalmology
Robotic systems have advanced ophthalmic surgeries, offering improved precision for procedures like phacoemulsification, keratoplasty, vitrectomy, and intravitreal injections. Early experiments, such as robot-assisted keratoplasty using the Da Vinci system, demonstrated the feasibility of corneal grafting and suturing in porcine and cadaver models. Devices like PRECEYES have enabled delicate retinal surgeries, such as membrane removal, and micro-cannulation has been successfully tested on pig eyes. The application of robotics extends to pterygium surgeries, amniotic membrane transplantation, and cataract surgeries aided by femtosecond lasers. Femtosecond lasers enhance safety and accuracy in procedures like LASIK, SMILE, and lamellar keratoplasties.
Robotic Surgery in Ophthalmology
Robotic systems have advanced ophthalmic surgeries, offering improved precision for procedures like phacoemulsification, keratoplasty, vitrectomy, and intravitreal injections. Early experiments, such as robot-assisted keratoplasty using the Da Vinci system, demonstrated the feasibility of corneal grafting and suturing in porcine and cadaver models. Devices like PRECEYES have enabled delicate retinal surgeries, such as membrane removal, and micro-cannulation has been successfully tested on pig eyes. The application of robotics extends to pterygium surgeries, amniotic membrane transplantation, and cataract surgeries aided by femtosecond lasers. Femtosecond lasers enhance safety and accuracy in procedures like LASIK, SMILE, and lamellar keratoplasties.
Key Robotic Platforms
1. Preceyes Surgical System
- Designed for vitreoretinal procedures, it provides joystick and foot pedal control for precise instrument movement. It also includes safety boundaries to prevent excessive motion.
- Applications: Subretinal drug delivery, epiretinal membrane (ERM) peeling, and internal limiting membrane (ILM) peeling.
2. Da Vinci Surgical System
- A versatile platform initially designed for general surgery, adapted for corneal and orbital surgeries.
- Features include remote-control instrument manipulation and multi-arm configurations.
3. KU Leuven Robotic System
- Offers stabilization for high-precision tasks like retinal vein cannulation.
- Combines manual handling with robotic support for tasks requiring sustained precision.
4. Medineering Robotic Endoscope Guiding System
- Originally designed for endoscopic applications, this system stabilizes visualization during orbital surgeries.
We will cover the common systems like the Da Vinci Surgical System and the Preceyes Surgical System as examples of current uses.
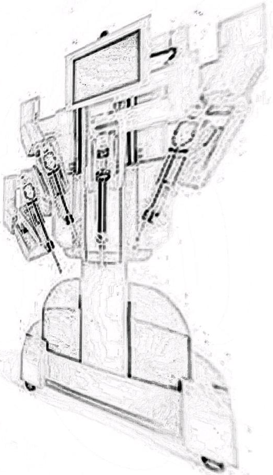
Da Vinci Surgical System
The Da Vinci Surgical System is one of the most well-established robotic platforms in medical surgery, (Figure 1) originally developed for general surgical procedures such as urology and gynecology. The da Vinci surgical system had four models for minimally invasive surgery: Si, X, Xi, and SP. The ExcelsiusGPS® is a computer-assisted system primarily for neurosurgical and spine procedures. It uses real-time navigation with three imaging systems: intraoperative 3D CT scan, preoperative 3D CT scan, and 2D fluoroscopy. [4]
The Da Vinci Surgical System is one of the most well-established robotic platforms in medical surgery, (Figure 1) originally developed for general surgical procedures such as urology and gynecology. The da Vinci surgical system had four models for minimally invasive surgery: Si, X, Xi, and SP. The ExcelsiusGPS® is a computer-assisted system primarily for neurosurgical and spine procedures. It uses real-time navigation with three imaging systems: intraoperative 3D CT scan, preoperative 3D CT scan, and 2D fluoroscopy. [4]
Da Vinci Surgical Systems adaptation to ophthalmology, however, represents a pioneering leap in leveraging robotic precision for delicate and complex eye surgeries. Manufactured by Intuitive Surgical, the system is designed to enhance surgical capabilities through a combination of robotic arms, 3D visualization, and remote-controlled manipulation.
Components and Design
The Da Vinci Surgical System consists of three primary components:
The Da Vinci Surgical System consists of three primary components:
1. Surgeon Console:
- The console allows the surgeon to operate the robotic arms from a remote station.
- It provides a high-definition, three-dimensional view of the surgical site, magnified up to 10 times, enhancing the precision of the surgeon’s actions.
- Two hand controls and foot pedals are used for intuitive and precise movements.
2. Patient Cart:
- The patient cart is equipped with robotic arms capable of holding surgical instruments and endoscopic cameras.
- The number of arms varies depending on the system (e.g., Da Vinci Xi has four arms).
- These arms replicate the surgeon’s hand movements in real-time, translating them into scaled, tremor-free motions.
3. Vision System:
- The vision system provides enhanced optical capabilities with stereoscopic cameras.
- It enables the surgeon to access hard-to-reach areas with unparalleled clarity and depth perception.
Applications in Ophthalmology
Initially designed for larger surgical fields, the Da Vinci system's adaptation to ophthalmology required significant modifications. Applications in eye care include:
Initially designed for larger surgical fields, the Da Vinci system's adaptation to ophthalmology required significant modifications. Applications in eye care include:
- Corneal Transplantation:
- Used for precision-based amniotic membrane grafting and penetrating keratoplasty.
- Reports suggest the system aids in minimizing suture-related complications.
- Orbital and Adnexal Surgeries:
- Includes orbital tumor excision and orbital decompression surgeries for conditions like Graves' orbitopathy.
- Robotic arms provide steady control, reducing the risk of excessive tissue damage.
- Pterygium Surgery:
- The system facilitates meticulous removal of pterygium tissue, particularly in recurrent cases.
Advantages
1. Precision and Stability:
- The robotic arms filter out physiological tremors, providing unprecedented stability for delicate maneuvers.
2. Enhanced Visualization:
- The stereoscopic imaging system allows better visualization of microscopic structures, such as corneal layers or orbital tissues.
3. Ergonomics:
- Surgeons operate from a seated console, reducing physical strain during lengthy procedures.
4. Minimally Invasive Approach:
- Smaller incisions lead to faster recovery times and fewer complications for patients. [5]
Challenges and Limitations
1. Procedure Duration:
1. Procedure Duration:
- Robotic surgeries with the Da Vinci system are generally longer than manual techniques due to setup and calibration requirements.
- The steep learning curve for surgeons further adds to the operational time.
2. Cost:
- The system is prohibitively expensive, with initial investments and maintenance costs posing significant barriers for adoption in ophthalmology.
3. Compatibility Issues:
- Adapting the system for smaller, rotational surgical fields in ophthalmology remains challenging.
4. Limited Evidence:
- Most studies involving the Da Vinci system in eye care are case reports or small-scale trials, limiting generalizable conclusions about its efficacy. [5,6,7]
- Evidence
- In a case series on pterygium surgeries, the system demonstrated high surgical success rates with minimal complications. However, the procedural time was significantly longer than traditional methods.
- Orbital fat decompression surgeries performed with the Da Vinci system reported reduced intraoperative bleeding and improved cosmetic outcomes. [6,7]
- Future Directions
- Enhancing the system’s miniaturization and flexibility for ophthalmic applications is a priority.
- Integrating advanced imaging technologies, such as intraoperative OCT, can further refine surgical precision.
- Reducing costs and developing dedicated training programs will be crucial for widespread adoption in eye care.
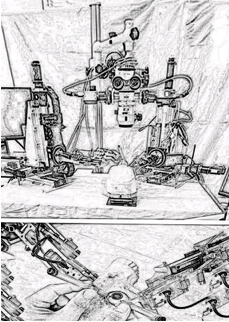
Preceyes Surgical System
The Preceyes Surgical System, developed by Preceyes B.V., is a robotic platform specifically designed for vitreoretinal surgeries. Unlike the Da Vinci system, Preceyes is purpose-built for the intricate demands of intraocular procedures, offering unparalleled precision for tasks requiring sub-micron accuracy.
The Preceyes Surgical System, developed by Preceyes B.V., is a robotic platform specifically designed for vitreoretinal surgeries. Unlike the Da Vinci system, Preceyes is purpose-built for the intricate demands of intraocular procedures, offering unparalleled precision for tasks requiring sub-micron accuracy.
Components and Design
The Preceyes system features a single robotic arm controlled via a combination of joystick and foot pedals. Key components include:
The Preceyes system features a single robotic arm controlled via a combination of joystick and foot pedals. Key components include:
1. Robotic Arm:
- The arm is equipped with a trocar holder and safety-encoded boundaries to prevent excessive instrument movement.
- Compatible with 23-, 25-, and 27-gauge instruments, commonly used in vitreoretinal surgeries.
2. Control System:
- A joystick and foot pedal interface allows surgeons to manipulate the robotic arm with precision and ease.
- Movements are scaled down, translating millimeter-scale joystick inputs into sub-micron movements.
3. Integrated Headrest and Trocar System:
- Designed to stabilize the patient’s eye during surgery, ensuring minimal motion.
Applications in Ophthalmology
The Preceyes system has demonstrated its utility in several vitreoretinal procedures, including:
The Preceyes system has demonstrated its utility in several vitreoretinal procedures, including:
- Subretinal Drug Delivery:
- Used for injecting tissue plasminogen activator (tPA) in cases of subfoveal hemorrhage.
- Offers consistent injection volumes and reduces the risk of over- or under-dosing.
- Epiretinal and Internal Limiting Membrane Peeling:
- Facilitates precise membrane removal for macular holes and ERM.
- Reduces the risk of iatrogenic retinal trauma.
- Retinal Vein Cannulation:
- Demonstrates the potential for advanced treatments like targeted drug delivery to occluded retinal veins.
Advantages
1. Unmatched Precision:
- The sub-micron accuracy is particularly valuable for procedures like subretinal injections and delicate membrane peeling.
2. Safety Features:
- Encoded safety boundaries prevent unintentional damage to surrounding ocular structures.
3. Learning Curve:
- Easier to master compared to multi-arm systems like Da Vinci, due to its simpler control mechanism.
4. Reduction in Surgeon Fatigue:
- Enables steady instrument manipulation without requiring prolonged manual focus.
Challenges and Limitations
1. Limited Applications:
- Primarily restricted to vitreoretinal surgeries, limiting its scope in broader ophthalmology.
2. Procedural Duration:
- Similar to the Da Vinci system, Preceyes-assisted procedures often take longer than manual surgeries.
3. Cost and Accessibility:
- High upfront costs and maintenance expenses remain significant barriers.
- Case Studies and Evidence
- In a randomized controlled trial (RCT) comparing manual and Preceyes-assisted surgeries for ERM peeling, outcomes were comparable in terms of surgical success and retinal thickness improvement. However, robotic procedures took significantly longer.
- Subretinal tPA delivery using the Preceyes system showed superior precision and consistency compared to manual injections, though not statistically significant in overall efficacy.[8,9]
Future Directions
- Expanding the system’s capabilities to anterior segment surgeries, such as corneal transplantation, could broaden its utility.
- Incorporating AI-driven automation for specific tasks, like retinal vein cannulation, could further enhance its efficiency.
- Efforts to reduce costs and improve accessibility will be crucial for adoption in routine clinical practice.
- Emerging players and trends
Corporate Players
The robotic eye surgery market is seeing rapid expansion with four major companies leading the way:
Acu Surgical and Zeiss Exchange Robotics: Already in limited human use for retina surgeries outside the United States.
Acu Surgical and Zeiss Exchange Robotics: Already in limited human use for retina surgeries outside the United States.
For Sight Robotics and Horizon Surgical Systems: Still in preclinical stages, focusing on technological development and validation. [8,10]
Vitreoretinal Surgeries
Robotic systems are primarily trialed in posterior segment procedures. Studies demonstrate that robots can assist in tasks requiring sub-micron precision, such as:
Robotic systems are primarily trialed in posterior segment procedures. Studies demonstrate that robots can assist in tasks requiring sub-micron precision, such as:
- Subretinal drug delivery, improving consistency in injection volume and duration.
- Membrane peeling for conditions like macular holes and ERM.
Although outcomes in terms of retinal thickness and visual acuity were comparable to manual techniques, robots provided superior consistency and reduced surgeon strain during prolonged procedures.[8] Corneal and Ocular Surface Procedures
The Da Vinci Surgical System has been tested for corneal transplantation and amniotic membrane grafting. However, procedural durations were longer due to the setup and learning curve associated with the system.[11,12,13]
Cataract
Robot-assisted cataract surgery using phacoemulsification was successfully done on 25 lens nuclei. The average operation time was about 26.44 minutes, with a standard deviation of 5.15 minutes. Key factors for completing the main steps of the procedure include intraocular dexterity and clear visualization of the operative field. [14]
Robot-assisted cataract surgery using phacoemulsification was successfully done on 25 lens nuclei. The average operation time was about 26.44 minutes, with a standard deviation of 5.15 minutes. Key factors for completing the main steps of the procedure include intraocular dexterity and clear visualization of the operative field. [14]
Femtosecond Lasers, Orbital and Adnexal Surgeries
Femtosecond lasers, widely used in various types of eye surgeries, including LASIK, SMILE, penetrating keratoplasty (PKP), insertion of intracorneal ring segments, anterior and posterior lamellar keratoplasty, deep anterior lamellar keratoplasty (DALK) and Descemet's stripping endothelial keratoplasty (DSEK) are useful for adjunctive robotic use. Applications include robotic-assisted orbital fat decompression and tumor excision. Early results suggest improved precision and reduced intraoperative bleeding, but limited sample sizes and procedural complexity hinder conclusive evidence. [15]
Femtosecond lasers, widely used in various types of eye surgeries, including LASIK, SMILE, penetrating keratoplasty (PKP), insertion of intracorneal ring segments, anterior and posterior lamellar keratoplasty, deep anterior lamellar keratoplasty (DALK) and Descemet's stripping endothelial keratoplasty (DSEK) are useful for adjunctive robotic use. Applications include robotic-assisted orbital fat decompression and tumor excision. Early results suggest improved precision and reduced intraoperative bleeding, but limited sample sizes and procedural complexity hinder conclusive evidence. [15]
Advantages of Robotic Systems
1. Enhanced Precision
- Robotic systems mitigate the impact of physiological tremors, enabling more stable and accurate instrument manipulation.
- Integration of intraoperative optical coherence tomography (OCT) enhances real-time feedback, critical for high-precision tasks.
2. Improved Ergonomics
- Surveys report reduced physical strain for surgeons using robotic systems, particularly in procedures requiring extended focus.
3. Minimally Invasive and Remote Capabilities
- Robotic systems can enable remote surgery, providing access to patients in underserved areas.
4. Innovative Training Tools
- Virtual reality simulators and robotic-assisted training platforms enhance skill acquisition and procedural confidence.
Limitations and Challenges
Procedural Duration
Robotic-assisted surgeries consistently require longer operation times compared to manual techniques. This is attributed to:
Procedural Duration
Robotic-assisted surgeries consistently require longer operation times compared to manual techniques. This is attributed to:
- Extensive setup and calibration.
- The learning curve associated with mastering robotic systems.
Cost and Accessibility
The high costs of robotic platforms and their associated maintenance limit adoption, particularly in low-resource settings.
Technical and Practical Barriers
The high costs of robotic platforms and their associated maintenance limit adoption, particularly in low-resource settings.
Technical and Practical Barriers
- Existing robotic systems are not fully optimized for the small and rotationally mobile surgical field of the eye.
- Integration with current surgical setups, such as operating microscopes and patient headrests, remains a challenge.
Lack of Standardization and Training
The absence of standardized robotic protocols in ophthalmology hinders large-scale adoption. Additionally, most surgeons lack training in robotic-assisted techniques, further delaying clinical integration.
The absence of standardized robotic protocols in ophthalmology hinders large-scale adoption. Additionally, most surgeons lack training in robotic-assisted techniques, further delaying clinical integration.
Current Evidence and Research Gaps
The reviewed articles highlight the scarcity of large-scale randomized controlled trials (RCTs) evaluating robotic-assisted surgeries in ophthalmology. Existing studies primarily consist of case reports and small case series, with the exception of a few RCTs involving the Preceyes Surgical System. [8-11] The key findings are as follows:
The reviewed articles highlight the scarcity of large-scale randomized controlled trials (RCTs) evaluating robotic-assisted surgeries in ophthalmology. Existing studies primarily consist of case reports and small case series, with the exception of a few RCTs involving the Preceyes Surgical System. [8-11] The key findings are as follows:
- Comparable clinical outcomes between robotic and manual surgeries in terms of visual acuity and retinal thickness.
- Limited complications, with no significant increase in ocular harms associated with robotic systems.
- Procedural durations often exceed manual techniques, reflecting practical inefficiencies.
The lack of patient-reported outcome measures (PROMs) and long-term follow-up studies further restricts our understanding of the broader impact of robotic systems on patient care.[6,8-11]
Future Directions
Technological Innovations
1. Miniaturization and Autonomy
Future Directions
Technological Innovations
1. Miniaturization and Autonomy
- Future robotic systems should focus on miniaturization for compatibility with ophthalmic procedures.
- Autonomous features, such as automated suturing or membrane dissection, could reduce reliance on manual inputs.
2. AI Integration
- AI can enhance robotic decision-making, providing predictive analytics for surgical planning and intraoperative adjustments.
3. Improved Ergonomics and Workflow
- Streamlined integration with surgical setups and reduced preparation times are critical for practical adoption.
Research Priorities
Should include the following:
Should include the following:
- Conducting large-scale RCTs to establish the efficacy and safety of robotic systems across diverse ophthalmic procedures.
- Developing standardized training programs and certifications for robotic-assisted surgeries.
- Exploring cost-effective solutions to make robotic systems accessible to low-resource settings.
Conclusion
Robotic surgery in ophthalmology is a promising yet evolving field. Current systems demonstrate significant potential to enhance precision, reduce surgeon strain, and facilitate complex procedures. However, challenges such as high costs, extended procedural durations, and the need for robust clinical evidence hinder widespread adoption.
Future advancements in technology, combined with comprehensive research and training initiatives, are essential for robotic systems to transform eye care. With continued innovation, robotic-assisted surgeries could overcome current physiological and logistical barriers, offering unprecedented opportunities for improving surgical outcomes and expanding access to high-quality eye care worldwide.
Conflict of Interest: None declared.
Financial Disclosures: None.
References
- Karel C?apek, Selver P. R.U.R. (1928). (Rossum’s universal robots); a fantastic melodrama. Garden City, N.Y.: Doubleday, Doran.
- Asimov I. (2000). The bicentennial man and other stories. 1st ed. London: Millennium.
- D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A. (2019). Robotic-Assisted Spine Surgery: History, Efficacy, Cost, and Future Trends. Robotic Surgery: Research and Reviews. 6: 9-23.
- Kalan S, Chauhan S, Coelho RF, Orvieto MA, Camacho IR, Palmer KJ, et al. (2010). History of robotic surgery. Journal of Robotic Surgery. 4(3): 141–7.
- Bourla DH, Hubschman JP, Culjat M, Tsirbas A, Gupta A, Schwartz SD. (2008). Feasibility Study Of Intraocular Robotic Surgery With The Da Vinci Surgical System. Retina. Jan 1 28(1): 154–8.
- Rahimy E, Wilson J, Tsao T-C, Schwartz S, Hubschman J-P. (2013). Robot-assisted intraocular surgery: development of the IRISS and feasibility studies in an animal model. Eye. 27(8): 972–8.
- Bourcier T, Nardin M, Sauer A, Gaucher D, Speeg C, Mutter D, et al. (2015). Robot-Assisted Pterygium Surgery: Feasibility Study in a Nonliving Porcine Model. Translational Vision Science & Technology. 4(1): 9–9.
- de Smet MD, Naus GJL, Faridpooya K, Mura M. (2018). Robotic-assisted surgery in ophthalmology. Current Opinion in Ophthalmology. 29(3): 248–53.
- Edwards TL, Xue K, Meenink HCM, Beelen MJ, Naus GJL, Simunovic MP, et al. (2018). First-in-human study of the safety and viability of intraocular robotic surgery. Nature Biomedical Engineering [Internet]. Jun 18 2(9): 649–56.
- Kamthan G, Ianchulev S. Robotics in Ophthalmology [Internet]. CRSToday. Available from:https://crstoday.com/articles/june-2023/robotics-in-ophthalmology
- Bourges J-L, Hubschman J-P, Burt B, Culjat M, Schwartz SD. (2009). Robotic microsurgery: corneal transplantation. The British journal of ophthalmology. 1672–5.
- Chammas J, Sauer A, Pizzuto J, Pouthier F, Gaucher D, Marescaux J, et al. (2017). Da Vinci Xi Robot–Assisted Penetrating Keratoplasty. Translational Vision Science & Technology [Internet]. 6(3): 21–1.
- Bourcier T, Becmeur PH, Mutter D. (2015). Robotically Assisted Amniotic Membrane Transplant Surgery. JAMA Ophthalmology. 133(2): 213.
- Bourcier T, Chammas J, Becmeur PH, Sauer A, Gaucher D, Liverneaux P, et al. (2017). Robot-assisted simulated cataract surgery. Journal of Cataract and Refractive Surgery. 43(4): 552–7.
- Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, McAlinden C, Pineda R, et al. (2015). The evolution of corneal and refractive surgery with the femtosecond laser. Eye and Vision. 14: 2.
Citation: Jatinder Bali and Nandan Bali. (2025). Robotic Surgery in Eye Care: A Comprehensive Review. Journal of Ophthalmology and Vision Research 7(1).
Copyright: © 2025 Jatinder Bali. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.