Case Report
Volume 7 Issue 1 - 2025
Unilateral Open Angle Glaucoma in Ipsilateral Nevus of Ota: An Oculo-Dermal Association
1Department of Ophthalmology, Dr Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh
2Assistant Professor, Department of Dermatology, Dr Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh
2Assistant Professor, Department of Dermatology, Dr Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh
*Corresponding Author: Dr. Mukta Sharma, Department of Ophthalmology, Dr Radhakrishnan Government Medical College, Hamirpur, Himachal Pradesh.
Received: February 17, 2025; Published: February 24, 2025
Abstract
Oculodermal Melanocytosis (Nevus of Ota) is a hamartomatous nevus of dermal melanocytes. It presents as a bluish grey patch on the face involving the area of distribution of the ophthalmic and maxillary divisions of the trigeminal nerve. The nevus can be unilateral or bilateral, and in addition to skin, it may involve ocular and oral mucosal surfaces. It is a rare disorder and the ocular complications, such as glaucoma and melanoma, may be vision or life-threatening. Here we report a case of 20 years old female who presented with decreased vision in her right eye. On detailed examination it turned out to be a case of Nevus of Ota with Open Angle Glaucoma.
Keywords: Nevus of Ota; Oculodemal Melanocytosis; Glaucoma
Introduction
Oculodermal Melanocytosis, commonly known as Nevus of Ota, was first described by Masao Ota of Japan in 1939. It affects 0.014-0.034% of population in South East Asia. It is more prevalent in Japan, where the incidence is about 0.2-0.3%. Unilateral involvement is the rule in 90%, but 10% of the cases may be bilateral. It typically presents at birth but can also appear in puberty or during pregnancy. Females are more prone than males, with a ratio of 5:1. [1]
The condition manifests as a bluish grey patch in the areas of distribution of the ophthalmic and maxillary divisions of the trigeminal nerve. Entrapment of melanocytes in upper one third of the dermis leads to grayish-blue macular hyperpigmentation of the ipsilateral facial skin. Rarely, there can also be intraoral involvement with similar pigmented lesions seen on the palate. [2,3,4]
Ocular manifestations include episcleral or scleral melanosis, heterochromia, iris mammillations and glaucoma. Nevus of Ota extending into the eye have an increased risk of developing glaucoma (in 10% of patients) as invasion of melanocytes can block drainage of aqueous, leading to elevated intraocular pressures. Malignant Cutaneous or Ocular Melanoma may develop in these patients.1 in 400 patients can develop Uveal (typically choroidal) melanoma in the affected eye. Risk factors for malignant transformation include
- Related Cutaneous or Palatal Melanocytosis (especially in the temple)
- Scleral involvement of the superior, nasal, or temporal quadrants
- Diffuse iris Melanocytosis
Choroidal Melanocytosis Diagnosis of Nevus of Ota can be made based on its clinical morphology and sites of involvement. [5,6] Our aim to report this case is to apprise the healthcare professionals about the long-term ocular complications that can be associated with this rare disorder.
Case Report
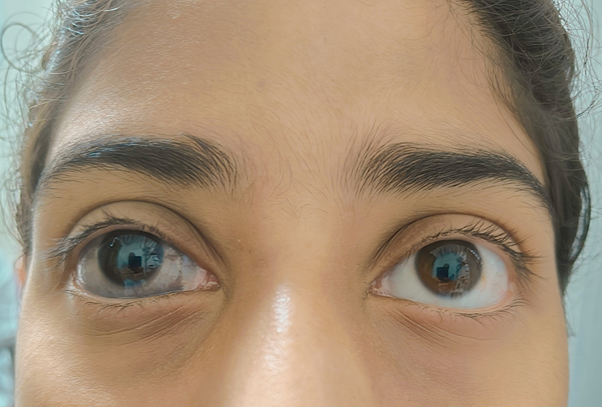
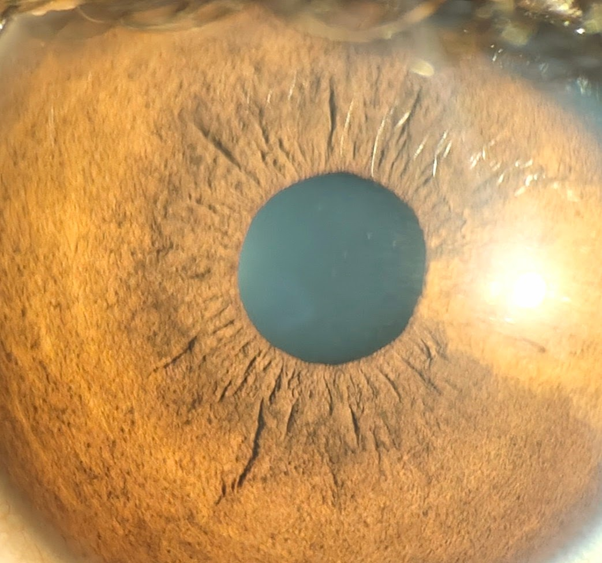
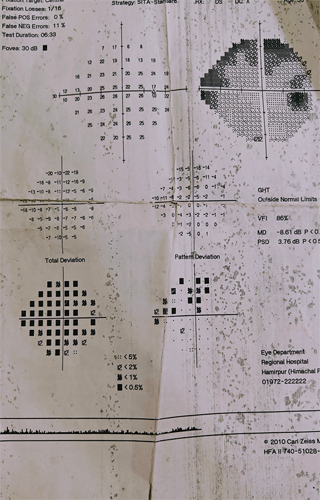
A 20 years old female presented in our OPD with the chief complaint of diminution of vision in her right eye for the past few months. On examination Visual Acuity in Right and Left eye was 6/36 (6/18 after correction with -1.50DSp) and 6/6 respectively. Pupillary reactions were normal. Slit Lamp Examination revealed bluish grey discoloration of sclera involving almost all the quadrants and darkly pigmented iris (Heterochromia) in right eye, as compared to the left eye. Dilated fundus examination was done. To our surprise the Cup Disc Ratio in the right and left eye was 0.4 and 0.2 respectively. Intraocular Pressure by GAT was recorded to be 22 and 18mmHg respectively. She was called again for Visual Field Examination and Gonioscopy. On Visual Field Examination, early glaucomatous field defects were observed on the right side. Gonioscopy was done using Posner 4 mirror Gonioscope which revealed open angles with all the angle structures visible but darkly pigmented trabecular meshwork on the right side, as compared to the normal side. Dermatologist consultation was also sought and diagnosis of Nevus of Ota with Open Angle Glaucoma was made. She was put on Anti Glaucoma Treatment and kept under life long six monthly follow up.
Slit Lamp Picture of Nevus of Ota and Visual Field Printout as shown in Pics 1-3.
Discussion
Nevus of Ota is rare disorder that affects Asians and blacks more commonly than Whites. Pathophysiology is still unconfirmed. It is postulated that it results from defective migration of neural crest cells to the epidermis during embryonic stage. The two peak ages of onset are early infancy and early adolescence suggesting that hormones play a role in the development of this condition. After its onset, Nevus of Ota may enlarge slowly and progressively darken in color. Its appearance usually remains stable once adulthood is reached. Dermatosis that needs to be considered in the Differential diagnosis are many. Few of the important ones are:
Ocular melanosis is a condition differentiated from Nevus of Ota by the absence of eyelid involvement.
Nevus of Ito is a condition differentiated by hyperpigmentation of the neck, shoulders, axilla, and upper extremity.
Nevus of Hori is a condition almost identical to Nevus of Ota, but it is bilateral on presentation, as opposed to the unilateral Nevus of Ota.
Acquired Bilateral Nevus of Ota-like Macules (ABNOM)- Sclera and Oral mucosa are not involved in ABNOM or Sun’s nevus.
Drug-induced hyperpigmentation is usually after the ingestion of drugs like minocycline, amiodarone, and gold.
Melasma - typically associated with pregnancy. [7] Treatment of skin lesions depend upon patient’s choice since these are not life threatening. The Q- switched lasers (694 nm Ruby, 755 nm Alexandride or 1064 nm Nd-Yag) with their high peak power and pulse width in nano second range are best suited to treat various epidermal, junctional, mixed and dermal lesions. The Q-switched Nd-YAG is an ideal choice to treat dermal pigment as in Nevus of Ota and in darker skin types, as it reduces the risk of epidermal injury and pigmentary alterations. [8] Ocular associations are present and include involvement of sclera, cornea, anterior chamber angle, iris, retina and optic disc. The two vision-threatening complications are glaucoma and uveal melanoma. The metastasis from uveal melanoma can risk the life of the patient. The risk of glaucoma is 10 - 15%. In cases of uveal melanoma, 3% have evidence of Nevus of Ota. Moreover, the risk of metastasis from uveal melanoma is also higher in cases of Nevus of Ota, although it is a benign and rare disorder. [9]
Conclusion
Ocular associations of Nevus of Ota may be vision and life threatening. Therefore, any such patient coming to our OPD must be examined keeping in mind the possible complications and be put on a regular and long-term follow-up by an Ophthalmologist and Dermatologist.
References
- Oninikoyi, Omobola; Adigun, Chris G. Lui, (2007). Harvey. Nevus of Ota and Ito. March 22, 2008.
- Rapini RP, Bolognia JL, Jorizzo JL. Dermatology: 2-Volume Set. St. Louis: Mosby. 1720-22: 3. Bhattacharya, S. K., Girgla, H. S., & Singh, G. (1973). Nevus of Ota. International Journal of Dermatology. 12(6): 344-347:
- Chauhan, A., Sharma, N., Dutt S. (2016). Nevus of Ota. DOS times. Page 16-17:
- Kopf, A.W &Weidman, A. I. (1962). Nevus of Ota. Archives of Dermatology. 85(2): 195-208.
- Hannan, C. (2018). Nevus of Ota: Treatment, Eye, Removal, Glaucoma, and More. Healthline.
- Bisceglia M, Carosi I, Fania M, Di Ciommo A, Lomuto M. (1997). Nevus of Ota. Presentation of a case associated with a cellular blue nevus with suspected malignant degeneration and review of the literature. Pathologica. 89(2): 168-74.
- Skin treatment Patil, Uddhav A.; Dhami, Lakshyajit D. (2008). Indian Journal of Plastic Surgery. Mumbai, India: 41 (Supplement) 101–113.
- Magarasevic L, Abazi Z. (2013). Unilateral open-angle glaucoma associated with the ipsilateral Nevus of Ota. Case Report Ophthalmol .924-37.
Citation: Mukta Sharma and Neeraj Sharma. (2025). Unilateral Open Angle Glaucoma in Ipsilateral Nevus of Ota: An Oculo-Dermal Association. Journal of Ophthalmology and Vision Research 7(1).
Copyright: © 2025 Mukta Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.