Case Report
Volume 5 Issue 1 - 2023
Short-term Efficacy of Vitrectomy Combined with Air Tamponade on Rhegmatogenous Retinal Detachment with Inferior Holes
Department of Retinal and Vitreous Diseases, Nanjing Aier Hospital, Aier Medical Group, Nanjing 210006, China
*Corresponding Author: He Yongning, NanJing Aier Eye Hospital, No.100 Xianhe Street, Qinhuai District, Nanjing, Jiangsu Province, China
Received: April 18, 2023; Published: April 29, 2023
Abstract
Purpose: To observe the short-term efficacy of vitrectomy combined with air tamponade for rhegmatogenous retinal detachment (RRD) with inferior holes.
Methods: Retrospective case series. Fifty patients with RRD and inferior holes who underwent pars plana vitrectomy (PPV) combined with air tamponade from June 2017 to December 2020 in Nanjing Aier Hospital were analyzed. Best-corrected visual acuity (BCVA) measurement, non-contact intraocular pressure (NCT) evaluation, slit-lamp microscopy, indirect funduscopy with a slit lamp, wide-angle fundus photography, optical coherence tomography (OCT), ophthalmic AB ultrasound examination, and evaluation of the length of the optic axis with the IOL-Master were performed before surgery. All patients underwent 23-gauge vitrectomy combined with air tamponade. The aforementioned examinations were performed at 5 days, 3 weeks, and 3 months postoperatively. Retinal reattachment, BCVA, intraocular pressure, and complications were observed.
Results: Initial reattachment was achieved in 98% of the 49 patients 3 months after surgery. No patient had retinal redetachment during the follow-up. Preoperative LogMAR BCVA was 1.81 ± 0.87, and at 5 days, 3 weeks, and 3 months after surgery were 0.72 ± 0.35, 0.59 ± 0.34, and 0.58 ± 0.32, respectively. All patients gained better postoperative BCVA (P<0.001). Increased ocular pressure was found in two cases on the first postoperative day, and the pressure returned to normal after drainage of the anterior chamber fluid. Local retinal redetachment occurred in one patient two months after surgery. This patient underwent scleral buckling and final reattachment.
Conclusion: Vitrectomy combined with air tamponade is an effective treatment for RRD patients with well-relaxed and closed inferior retinal holes. It might reduce the complications from silicone oil tamponade and being in a facedown position for a long period.
Keywords: Retinal detachment; Vitrectomy; Air tamponade; Retinal surgery; Inferior holes
Introduction
Rhegmatogenous retinal detachment (RRD) is a common, blinding oculopathy, and treatment methods usually include scleral buckling, pars plana vitrectomy (PPV), or a combination of the methods [1-13]. Pars plana vitrectomy can find holes and release vitreous traction and is widely used in clinical practice. Pars plana vitrectomy requires the combined application of vitreous cavity filling, including inert gases, air, or silicone oil. The dark shadow formed by intravitreal gas causes poor vision for a period after surgery. It takes about 2 weeks for 20% of SF6 gas to be absorbed, and about 2 months for 13% of C3F8 to be absorbed [14-15]. Compared with inert gases, air is absorbed faster, effects a patient’s vision for a shorter period and is inexpensive. In addition, air tamponade is associated with a lower incidence of postoperative high intraocular pressure and postoperative complicated cataract [14]. According to the results of many studies [16-20], the surgical success rate is about the same between inert gas tamponade and air tamponade in the treatment of RRD, regardless of the locations of the holes. Whereas other studies have shown that inert gas tamponade was superior to air tamponade for inferior holes [10, 21]. In 2013, Tan et al. [10] showed that the overall success rates of intravitreal air tamponade and SF6 tamponade in the treatment of RRD were 81.0% and 86.9%, respectively. However, in the cases with RRD involving the inferior quadrants, the reattachment rate in the air tamponade group was 69.6%, lower than the 84.7% success rate in the SF6 tamponade group. In 2015, Zhou et al. [21] performed PPV with air tamponade in 32 patients with inferior retinal detachment, and the primary reattachment rate was 84.4%. In 2019, Tetsumoto et al. [22] reported no difference in the reattachment rates between air tamponade and 20% SF6 tamponade for 27-gauge PPV in the treatment of RRD, irrespective of where the clock positions of the holes were. Therefore, the application of air tamponade in the treatment of RRD of inferior holes remains controversial. In recent years, owing to the limited application of inert gases in China, PPV with silicone oil tamponade in the treatment of RRD has mostly been applied. However, silicone oil tamponade can cause many complications, such as secondary glaucoma, aggravated cataract, and retinal toxicity, requiring facedown positioning for long periods, and the need for a second operation to remove the oil, which increases costs [23]. Lastly, RRD complicated by choroidal detachment (CD) is considered a contraindication for air tamponade. In this study, patients with RRD of inferior holes, including those with CD, were treated with PPV combined with air tamponade, in order to explore the feasibility of PPV with air tamponade in the treatment of RRD of inferior holes, thereby minimizing the use of silicone oil.
Materials and Methods
Subjects
A retrospective analysis was performed on 50 patients (50 eyes; 27 male and 23 female) with RRD of inferior holes who underwent 23G PPV in Nanjing Aier Hospital from February 2017 to December 2020. Inclusion criteria were as follows: (1) proliferative vitreous retinopathy (PVR) below grade C3, without obvious vitreoretinal proliferation, or with preretinal and subretinal proliferation, which could be completely released during surgery; (2) holes located below the 3-9 o’clock horizontal line, without restriction on the size and number of holes; (3) no restriction on the range of retinal detachment; (4) no restriction on whether it was combined with CD and the degree of CD; (5) no restriction on refractive degree and ocular axial length; (6) no restriction on whether there was dialysis of ora serrata or recurrent retinal detachment after PPV. Exclusion criteria were as follows: (1) those with retinal proliferation, stiffness, anterior displacement, and retinal shortening; (2) those with a significantly atrophied choroid and retinal pigment epithelium (RPE)-Bruch membrane complex in the macular region and a visible macular hole of the sclera; (3) those with tractional detachment of the retina.
A retrospective analysis was performed on 50 patients (50 eyes; 27 male and 23 female) with RRD of inferior holes who underwent 23G PPV in Nanjing Aier Hospital from February 2017 to December 2020. Inclusion criteria were as follows: (1) proliferative vitreous retinopathy (PVR) below grade C3, without obvious vitreoretinal proliferation, or with preretinal and subretinal proliferation, which could be completely released during surgery; (2) holes located below the 3-9 o’clock horizontal line, without restriction on the size and number of holes; (3) no restriction on the range of retinal detachment; (4) no restriction on whether it was combined with CD and the degree of CD; (5) no restriction on refractive degree and ocular axial length; (6) no restriction on whether there was dialysis of ora serrata or recurrent retinal detachment after PPV. Exclusion criteria were as follows: (1) those with retinal proliferation, stiffness, anterior displacement, and retinal shortening; (2) those with a significantly atrophied choroid and retinal pigment epithelium (RPE)-Bruch membrane complex in the macular region and a visible macular hole of the sclera; (3) those with tractional detachment of the retina.
The study conduct followed the principles of the Declaration of Helsinki. Patients were fully informed of all aspects of the procedure, and all provided written informed consent. The study was conducted with approval from the Ethics Committee of Nanjing Aier Eye Hospital.
The mean age of the 50 patients was 57.18 ± 13.14 years, and the mean course of disease was 22.13 ± 32.05 days. There were 17 patients (34%) with CD, 7 patients (14%) with fixed retinal folds, 28 patients (56%) with multiple retinal holes (3 or more), and 14 patients (28%) with high myopia. According to the clock positions of the lowest hole, there were 12 eyes (24%) with holes located at 8-9 o’clock and 3-4 o’clock, 6 eyes (12%) with holes located at 7-8 o’clock and 4-5 o’clock, and 32 eyes (64%) with holes located at 5-7 o’clock. According to the range of retinal detachment, there was 1 eye (2%) involving 1 quadrant, 13 eyes (26%) involving 2 quadrants, 14 eyes (28%) involving 3 quadrants, and 22 eyes (44%) involving 4 quadrants. There were 5 eyes (10%) with grade A PVR, 38 eyes (76%) with grade B, 4 eyes (8%) with grade C1, and 3 eyes (6%) with grade C2.
Outcome measurements
All patients underwent preoperative BCVA using the Snellen visual acuity chart converted to the logarithm of the angle of minimum resolution, namely LogMAR visual acuity for statistical analysis. In addition, pre-operative examinations included non-contact intraocular pressure (NCT) evaluation, slit-lamp microscopy, indirect slit-lamp ophthalmoscopy, ocular A/B ultrasound, Aalborg wide-angle fundus photography, optical coherence tomography (OCT), and ocular axial length (IOL-master measurement).
All patients underwent preoperative BCVA using the Snellen visual acuity chart converted to the logarithm of the angle of minimum resolution, namely LogMAR visual acuity for statistical analysis. In addition, pre-operative examinations included non-contact intraocular pressure (NCT) evaluation, slit-lamp microscopy, indirect slit-lamp ophthalmoscopy, ocular A/B ultrasound, Aalborg wide-angle fundus photography, optical coherence tomography (OCT), and ocular axial length (IOL-master measurement).
Surgical methods
All subjects underwent three-port 23G PPV using the ALCON Constellation vitrectomy system under a binocular indirect ophthalmoscope (BIO) noncontact wide-angle retinoscope. During the operation, the vitreous at the incision was removed first, followed by vitrectomy at the central axis and posterior pole, and finally posterior vitreous detachment was performed. The vitreous body around the holes, areas of degeneration, and basal part were removed as much as possible. The holes and areas of degeneration were sealed by using a laser, and condensation was carried out if necessary. Complete gas-liquid exchange was performed, and the subretinal fluid was drained as much as possible. Sterile air was retained in the vitreous cavity. The puncture trocar was removed at a perfusion pressure of 35 mmHg using the vitrectomy machine. The self-closure incision was not sutured unless leaks were detected wherein the incision was sutured with an 8-0 absorbable suture. The intraocular pressure was adjusted to Tn.
All subjects underwent three-port 23G PPV using the ALCON Constellation vitrectomy system under a binocular indirect ophthalmoscope (BIO) noncontact wide-angle retinoscope. During the operation, the vitreous at the incision was removed first, followed by vitrectomy at the central axis and posterior pole, and finally posterior vitreous detachment was performed. The vitreous body around the holes, areas of degeneration, and basal part were removed as much as possible. The holes and areas of degeneration were sealed by using a laser, and condensation was carried out if necessary. Complete gas-liquid exchange was performed, and the subretinal fluid was drained as much as possible. Sterile air was retained in the vitreous cavity. The puncture trocar was removed at a perfusion pressure of 35 mmHg using the vitrectomy machine. The self-closure incision was not sutured unless leaks were detected wherein the incision was sutured with an 8-0 absorbable suture. The intraocular pressure was adjusted to Tn.
For some patients with severe CD, it was necessary to place a perfusion tube into the vitreous cavity using extra scleral drainage to promote choroid reattachment. According to the degree of lens opacity, 15 eyes simultaneously underwent phacoemulsification. Combined surgery was not recommended for patients with severe CD owing to a significant calculation error of the lens.
Facedown positioning was required for 3-5 days after the operation for all patients, and then patients adopted a prone or lateral head position which depended upon the location of the holes, to put the hole at the highest level. Patients with CD underwent the operation as soon as possible to minimize delays in treatment and 30-40 mg of prednisone was administered orally, once daily immediately after admission until 5 days postoperatively.
Postoperative follow-up and determination of reattachment
Postoperative examinations included BCVA measurement, NCT, slit-lamp microscopy, indirect slit-lamp ophthalmoscopy, OCT, and B-ultrasound and these examinations were performed 5 days, 3 weeks, and 3 months after surgery. The recorded time to complete air absorption and gas absorption was based on Aalborg wide-angle fundus photography and the time the patient subjectively perceived it took for the round air bubbles in front of their vision to completely disappear. The complete anatomical reattachment was confirmed by using indirect slit-lamp ophthalmoscopy, Aalborg wide-angle fundus photography, and B-ultrasound examination and flat retinal appearance.
Postoperative examinations included BCVA measurement, NCT, slit-lamp microscopy, indirect slit-lamp ophthalmoscopy, OCT, and B-ultrasound and these examinations were performed 5 days, 3 weeks, and 3 months after surgery. The recorded time to complete air absorption and gas absorption was based on Aalborg wide-angle fundus photography and the time the patient subjectively perceived it took for the round air bubbles in front of their vision to completely disappear. The complete anatomical reattachment was confirmed by using indirect slit-lamp ophthalmoscopy, Aalborg wide-angle fundus photography, and B-ultrasound examination and flat retinal appearance.
Statistical analysis
SPSS25 statistical software was used to process the data. The independent sample t test was used for the data, and one-way analysis of variance was used for the comparison of the variables at different time points. P < 0.05 was considered to indicate statistical significance.
SPSS25 statistical software was used to process the data. The independent sample t test was used for the data, and one-way analysis of variance was used for the comparison of the variables at different time points. P < 0.05 was considered to indicate statistical significance.
Results
Primary attachment rate
At 5 days and 3 weeks after the operation, primary retinal reattachment was observed in all 50 patients. However, one patient with RRD of 360° total retinal detachment, involving 4 quadrants and complicated CD was observed to have local retinal detachment 2 months after surgery. The cause was undiscovered needle-like holes where the retina was reattached after scleral buckling. At 3 months after the operation, primary retinal reattachment was observed in all the other patients for an overall reattachment rate of 98%.
At 5 days and 3 weeks after the operation, primary retinal reattachment was observed in all 50 patients. However, one patient with RRD of 360° total retinal detachment, involving 4 quadrants and complicated CD was observed to have local retinal detachment 2 months after surgery. The cause was undiscovered needle-like holes where the retina was reattached after scleral buckling. At 3 months after the operation, primary retinal reattachment was observed in all the other patients for an overall reattachment rate of 98%.
In the 17 patients with RRD of inferior holes combined with CD, primary retinal reattachment was observed in 16 patients. Primary retinal reattachment was observed in all the 28 patients with retinal detachment involving 1-3 quadrants and 21 of the 22 patients with retinal detachment involving 4 quadrants.
Comparison of BCVA before and after the operation
The log MARBCVA before the operation was 1.81 ± 0.87 and the log MARBCVA at 5 days, 3 weeks, and 3 months after the operation were 0.72 ± 0.35, 0.59 ± 0.34, and 0.58 ± 0.32, respectively. BCVA at different times after the operation was significantly improved compared with that before the operation (each P < 0.05).
The log MARBCVA before the operation was 1.81 ± 0.87 and the log MARBCVA at 5 days, 3 weeks, and 3 months after the operation were 0.72 ± 0.35, 0.59 ± 0.34, and 0.58 ± 0.32, respectively. BCVA at different times after the operation was significantly improved compared with that before the operation (each P < 0.05).
Postoperative conditions and complications
The intraocular pressure was greater than or equal to 25 mmHg on the first day in 2 cases after the operation. It was speculated that it was caused by viscoelastic agent residues during the combined cataract surgery, and the intraocular pressure returned to normal after drainage of the anterior chamber fluid.
The intraocular pressure was greater than or equal to 25 mmHg on the first day in 2 cases after the operation. It was speculated that it was caused by viscoelastic agent residues during the combined cataract surgery, and the intraocular pressure returned to normal after drainage of the anterior chamber fluid.
About 1/2 of the air in the vitreous cavity was absorbed within 3-5 days after the operation; at this time, the macular fovea could be visualized. The dark shadow of air bubbles disappeared in front of patients’ eyes in an average of 12.3 days (10-15 days) as the air was completely absorbed.
One patient suffered intraoperative damage to the posterior lens capsule, resulting in complicated cataract. The preoperative visual acuity of the patient was tested by counting fingers in front of the eye and was 0.15 at 3 weeks after the operation. Figure1-4 are images of four patients preoperatively, postoperatively with partial gas tamponade, and 3 months postoperatively, respectively (Figure1-4).
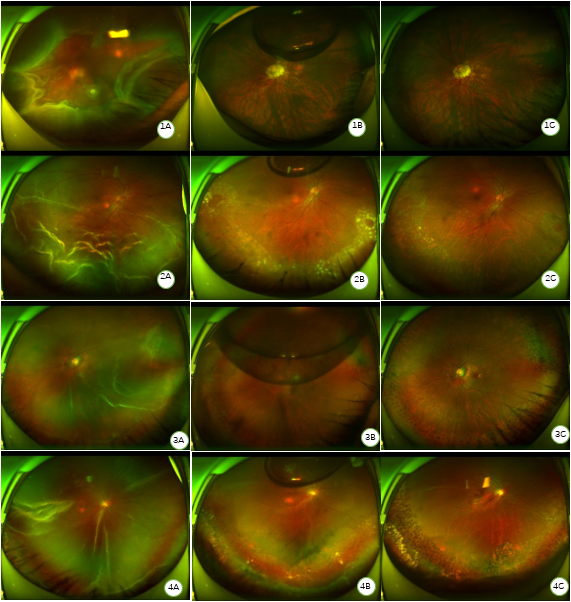
Figure 1: Images of a patient with high myopia and with large holes between the 5:30 and 2:00 o’clock meridians combined with 360° CD, preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 2: Images of an RRD patient with multiple holes, subretinal proliferative streaks combined with CD, preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 3: Images of an RRD patient with multiple holes combined with pathological myopia, preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 4: Images of a patient with retinal redetachment after oil removal preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 2: Images of an RRD patient with multiple holes, subretinal proliferative streaks combined with CD, preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 3: Images of an RRD patient with multiple holes combined with pathological myopia, preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Figure 4: Images of a patient with retinal redetachment after oil removal preoperatively (A), postoperatively with partial gas tamponade (B), and 3 months postoperatively (C).
Discussion
Feasibility of air tamponade after PPV in the treatment of RRD of inferior holes
As early as 1990, Carim [24] was the first to apply air tamponade in the treatment of retinal holes. In 2009, Hasegawa et al. [25] believed that air and SF6 had basically the same closure rate for macular holes. Gas tamponade can isolate intravitreal fluid and promote the reattachment of the retina and holes through surface tension. In 2020, Yu Ying et al. [23] performed air tamponade treatment on 90 eyes with RRD, of which, there were 7 eyes with inferior holes, and the primary retinal reattachment rate was 96.6%. Studies have shown that PPV with air tamponade in the treatment of RRD with superior holes has gradually been recognized. In 2005, Martinez-Castillo et al. [16] combined PPV with air tamponade treatment of RRD with inferior holes, and supine positioning for 30 minutes after the operation, and the primary reattachment rate reached 90% without the need for long term facedown positioning. The author speculated that it only took a few hours to form an effective adhesion around holes, especially in the first 24 hours after the operation, and after the formation of adhesions around the holes, intraocular fluid could not pass through and enter the subretinal cavity. Although air was absorbed quickly, the time was still sufficient to close the holes. The study showed that the average air-filled volume was about 77% (60% to 90%), 24 hours after surgery. It took an average of 3.8 days for the air to drop to 1/2 volume of the vitreous cavity, and it took about 10.9 days for complete absorption. In our study, facedown positioning was recommended for 3-5 days after the operation; by this time, about 1/2 of the air was absorbed. After that, patients adopted a prone or lateral head position, whichever put the hole higher, to continue to isolate the fluid. The primary reattachment rate in 50 patients was 98%, indicating that this approach was successful.
As early as 1990, Carim [24] was the first to apply air tamponade in the treatment of retinal holes. In 2009, Hasegawa et al. [25] believed that air and SF6 had basically the same closure rate for macular holes. Gas tamponade can isolate intravitreal fluid and promote the reattachment of the retina and holes through surface tension. In 2020, Yu Ying et al. [23] performed air tamponade treatment on 90 eyes with RRD, of which, there were 7 eyes with inferior holes, and the primary retinal reattachment rate was 96.6%. Studies have shown that PPV with air tamponade in the treatment of RRD with superior holes has gradually been recognized. In 2005, Martinez-Castillo et al. [16] combined PPV with air tamponade treatment of RRD with inferior holes, and supine positioning for 30 minutes after the operation, and the primary reattachment rate reached 90% without the need for long term facedown positioning. The author speculated that it only took a few hours to form an effective adhesion around holes, especially in the first 24 hours after the operation, and after the formation of adhesions around the holes, intraocular fluid could not pass through and enter the subretinal cavity. Although air was absorbed quickly, the time was still sufficient to close the holes. The study showed that the average air-filled volume was about 77% (60% to 90%), 24 hours after surgery. It took an average of 3.8 days for the air to drop to 1/2 volume of the vitreous cavity, and it took about 10.9 days for complete absorption. In our study, facedown positioning was recommended for 3-5 days after the operation; by this time, about 1/2 of the air was absorbed. After that, patients adopted a prone or lateral head position, whichever put the hole higher, to continue to isolate the fluid. The primary reattachment rate in 50 patients was 98%, indicating that this approach was successful.
Influence of CD on the efficacy of air tamponade therapy
Rhegmatogenous retinal detachment complicated by CD accounted for about 8.6% of the RRD cases [26]. Because of low intraocular pressure and damage to the vascular barrier, ocular uveitis is often severe, and proliferation is common after surgery, resulting in a lower reattachment rate than in simple RRD. Until now, the prevailing view has been that silicone oil tamponade must be applied in the treatment of RRD complicated by CD. Silicone oil tamponade, supplemented by patient positioning, can isolate intravitreal fluid for a long time, prevent fluid from entering the subretinal cavity, and promote hole closure and retinal reattachment. However, because silicone oil occupies a certain volume of the vitreous cavity, the concentration of intraocular inflammatory factors will be higher, and proliferation is more likely to occur. If the vitreous cavity is filled with air instead, the intraocular inflammatory factors will be diluted during air absorption, and the concentration will be lower than with silicone oil, potentially reducing the postoperative proliferative response. Yu Ying et al. [23] performed air tamponade treatment on 90 eyes with RRD and patients who had remission of mild to moderate CD after glucocorticoid treatment were included in the study. PPV with air tamponade or silicone oil tamponade treatment was administered, and the primary retinal reattachment rate in the air tamponade group was 96.6%. In this study, 17 out of 50 patients had CD, and 6 of them had intraocular pressure lower than 5 mmHg on the day of surgery. Significant choroidal detachment with hemispherical ridge-like bulging was observed during the operation. We speculated that compared with conventional RRD, the key to the treatment of RRD combined with CD was the closure of all holes, complete PVD, peri-break vitrectomy, and basal vitrectomy, to minimize retinal detachment caused by postoperative vitreous proliferation. During the operation, the vitreous body was stained with triamcinolone acetonide. The white particles of the drug attached to the surface of the vitreous and retina, which clearly showed the condition of the vitreous body. Suprachoroidal fluid was partially drained through the puncture opening during the surgery, and the vitreous body in the area of the holes and lattice degeneration, was removed as much as possible under the aid of perfluorcarbon and the assistant. In this study, the 17 patients with RRD with inferior holes combined with CD were treated with PPV with air tamponade, and 16/17 had primary retinal reattachment. The abovementioned results indicate that for RRD with inferior holes combined with CD, air tamponade could be used instead of silicone oil tamponade if the retina can be completely released, the vitreous body is properly handled, all holes and degeneration areas are sealed, and anti-inflammatory therapy is intensified.
Rhegmatogenous retinal detachment complicated by CD accounted for about 8.6% of the RRD cases [26]. Because of low intraocular pressure and damage to the vascular barrier, ocular uveitis is often severe, and proliferation is common after surgery, resulting in a lower reattachment rate than in simple RRD. Until now, the prevailing view has been that silicone oil tamponade must be applied in the treatment of RRD complicated by CD. Silicone oil tamponade, supplemented by patient positioning, can isolate intravitreal fluid for a long time, prevent fluid from entering the subretinal cavity, and promote hole closure and retinal reattachment. However, because silicone oil occupies a certain volume of the vitreous cavity, the concentration of intraocular inflammatory factors will be higher, and proliferation is more likely to occur. If the vitreous cavity is filled with air instead, the intraocular inflammatory factors will be diluted during air absorption, and the concentration will be lower than with silicone oil, potentially reducing the postoperative proliferative response. Yu Ying et al. [23] performed air tamponade treatment on 90 eyes with RRD and patients who had remission of mild to moderate CD after glucocorticoid treatment were included in the study. PPV with air tamponade or silicone oil tamponade treatment was administered, and the primary retinal reattachment rate in the air tamponade group was 96.6%. In this study, 17 out of 50 patients had CD, and 6 of them had intraocular pressure lower than 5 mmHg on the day of surgery. Significant choroidal detachment with hemispherical ridge-like bulging was observed during the operation. We speculated that compared with conventional RRD, the key to the treatment of RRD combined with CD was the closure of all holes, complete PVD, peri-break vitrectomy, and basal vitrectomy, to minimize retinal detachment caused by postoperative vitreous proliferation. During the operation, the vitreous body was stained with triamcinolone acetonide. The white particles of the drug attached to the surface of the vitreous and retina, which clearly showed the condition of the vitreous body. Suprachoroidal fluid was partially drained through the puncture opening during the surgery, and the vitreous body in the area of the holes and lattice degeneration, was removed as much as possible under the aid of perfluorcarbon and the assistant. In this study, the 17 patients with RRD with inferior holes combined with CD were treated with PPV with air tamponade, and 16/17 had primary retinal reattachment. The abovementioned results indicate that for RRD with inferior holes combined with CD, air tamponade could be used instead of silicone oil tamponade if the retina can be completely released, the vitreous body is properly handled, all holes and degeneration areas are sealed, and anti-inflammatory therapy is intensified.
Influence of the range of retinal detachment on the efficacy of air tamponade therapy
Zhou et al. [21] compared 32 cases of PPV combined with air tamponade and 32 cases of PPV combined with C3F8 tamponade in the treatment of RRD with inferior holes. The average number of quadrants involved was 2.96 in the reattachment group and 3.83 in the non-reattachment group and this difference was significant. Therefore, the spectrum of retinal detachment may be an independent risk factor affecting reattachment. Among the 50 patients in this study, the one case without reattachment had a 360° total retinal detachment, involving 4 quadrants combined with CD. The larger the range of retinal detachment, the more difficult it will be to handle the vitreous body. The activity, proliferation, traction, and contraction of the residual vitreous body can result in the reopening of original holes, the occurrence of new holes or tractional retinal detachment, which is the root cause of postoperative retinal redetachment. Therefore, proper vitreous handling is critical for the treatment of RRD when coupled with a wide range of involvement.
Zhou et al. [21] compared 32 cases of PPV combined with air tamponade and 32 cases of PPV combined with C3F8 tamponade in the treatment of RRD with inferior holes. The average number of quadrants involved was 2.96 in the reattachment group and 3.83 in the non-reattachment group and this difference was significant. Therefore, the spectrum of retinal detachment may be an independent risk factor affecting reattachment. Among the 50 patients in this study, the one case without reattachment had a 360° total retinal detachment, involving 4 quadrants combined with CD. The larger the range of retinal detachment, the more difficult it will be to handle the vitreous body. The activity, proliferation, traction, and contraction of the residual vitreous body can result in the reopening of original holes, the occurrence of new holes or tractional retinal detachment, which is the root cause of postoperative retinal redetachment. Therefore, proper vitreous handling is critical for the treatment of RRD when coupled with a wide range of involvement.
Postoperative intraocular pressure
Thompson et al. [27] concluded that increased intraocular pressure and the proportion of complicated cataract cases were significantly reduced when using air tamponade compared to inert gas tamponade. Jiayi Yang et al. [28] found that the occurrence of early high intraocular pressure after PPV was closely related to intraocular fillings and high myopia. The incidence of high intraocular pressure was 32.2% when silicone oil was used, whereas it was 13.3% when air tamponade was used, and 48.6% and 19.8% in patients with and without high myopia, respectively. Among the 50 patients in this study, 14 had high myopia, and only 2/50 had high intraocular pressure on the first day after the operation, and both underwent combined cataract surgery. The origin of the high intraocular pressure was thought to be caused by intraoperative viscoelastic agent residues, and the intraocular pressure returned to normal on the second day after drainage of the anterior chamber fluid. It was previously reported that the proportion of postoperative high intraocular pressure was elevated for RRD combined with CD. However, none of the 17 cases complicated by CD developed high intraocular pressure after air tamponade therapy in our study. The sample size was small, but our results strongly suggest that different fillings have a significant effect on intraocular pressure when our results are compared to the published literature.
Thompson et al. [27] concluded that increased intraocular pressure and the proportion of complicated cataract cases were significantly reduced when using air tamponade compared to inert gas tamponade. Jiayi Yang et al. [28] found that the occurrence of early high intraocular pressure after PPV was closely related to intraocular fillings and high myopia. The incidence of high intraocular pressure was 32.2% when silicone oil was used, whereas it was 13.3% when air tamponade was used, and 48.6% and 19.8% in patients with and without high myopia, respectively. Among the 50 patients in this study, 14 had high myopia, and only 2/50 had high intraocular pressure on the first day after the operation, and both underwent combined cataract surgery. The origin of the high intraocular pressure was thought to be caused by intraoperative viscoelastic agent residues, and the intraocular pressure returned to normal on the second day after drainage of the anterior chamber fluid. It was previously reported that the proportion of postoperative high intraocular pressure was elevated for RRD combined with CD. However, none of the 17 cases complicated by CD developed high intraocular pressure after air tamponade therapy in our study. The sample size was small, but our results strongly suggest that different fillings have a significant effect on intraocular pressure when our results are compared to the published literature.
Duration of facedown positioning
Facedown positioning is routinely required after PPV with silicone oil tamponade in the treatment of RRD, especially RRD with inferior holes, and the duration is usually 14 days to 1 month [12, 16, 21]. Our results support the conclusion that the duration of facedown positioning can be greatly shortened by PPV with air tamponade. Tetsumoto et al. [22] performed 27G PPV with air or SF6 tamponade for patients with RRD, and facedown positioning was required for at least 7 days after surgery. Xuemei Liang et al. [12] found that 3-5 days of facedown positioning after air tamponade was sufficient for the treatment of RRD of superior holes. Chen et al. [19] performed PPV combined with air tamponade for 37 patients with RRD, 5 of whom had inferior holes. Facedown positioning was strictly required for at least 1 day after surgery, and the primary reattachment rate was 100%. The 50 patients in this study all had RRD with inferior holes, and facedown positioning was required for 3-5 days after the operation, and then patients adopted a prone or lateral head position, to keep the hole at the highest level. Our primary reattachment rate was 98% supporting the conclusion that air tamponade can greatly shorten the duration of facedown positioning and relieve the pain of patients, while achieving a high reattachment rate.
Facedown positioning is routinely required after PPV with silicone oil tamponade in the treatment of RRD, especially RRD with inferior holes, and the duration is usually 14 days to 1 month [12, 16, 21]. Our results support the conclusion that the duration of facedown positioning can be greatly shortened by PPV with air tamponade. Tetsumoto et al. [22] performed 27G PPV with air or SF6 tamponade for patients with RRD, and facedown positioning was required for at least 7 days after surgery. Xuemei Liang et al. [12] found that 3-5 days of facedown positioning after air tamponade was sufficient for the treatment of RRD of superior holes. Chen et al. [19] performed PPV combined with air tamponade for 37 patients with RRD, 5 of whom had inferior holes. Facedown positioning was strictly required for at least 1 day after surgery, and the primary reattachment rate was 100%. The 50 patients in this study all had RRD with inferior holes, and facedown positioning was required for 3-5 days after the operation, and then patients adopted a prone or lateral head position, to keep the hole at the highest level. Our primary reattachment rate was 98% supporting the conclusion that air tamponade can greatly shorten the duration of facedown positioning and relieve the pain of patients, while achieving a high reattachment rate.
The failure of PPV for RRD is mainly caused by vitreous proliferation and missed or new holes. Therefore, all holes should be found, and the vitreous body around holes, degenerated areas, and the peripheral basal vitreous body, especially the vitreous body within the range of retinal detachment, should be removed as much as possible. If there is preretinal or subretinal proliferation, intraoperative release is required. If the retina can be completely released and lie completely flat in the gas-filled state after gas-liquid exchange, then air tamponade can be used. If there is retinal thickening, intraretinal proliferation, shortening of the retina, anterior displacement, and so on, which may require retinal incision to be completely released, then silicone oil tamponade is still recommended. In this study, there were 7 patients with grade C1-2 PVR and fixed retinal folds. After intraoperative removal of preretinal or subretinal proliferation, the retina could be fully released. All patients still underwent air tamponade, and there was no retinal redetachment after reattachment.
In conclusion, treatment of RRD with inferior holes, even with CD, PPV with air tamponade can be highly successful provided the retina can be fully released during surgery, and there can be proper handling of the vitreous body around degenerated areas and holes and all holes closed. Additional advantages of air tamponade included the reduction in the use of silicone oil, shortening the duration of facedown positioning, and reduced incidence of postoperative high intraocular pressure.
Acknowledgements: We would like to thank Editage (www.editage.cn) for English language editing.
References
- Hwang JC. (2012). Regional practice patterns for retinal detachment repair in the United States. Am J Ophthalmol. 153(6): 1125–1128.
- Nemet A, Moshiri A, Yiu G, Loewenstein A, Moisseiev E. (2017). A review of innovations in rhegmatogenous retinal detachment surgical techniques. J Ophthalmol. 2017: 4310643.
- Chan CK, Lin SG, Nuthi AS, Salib DM. (2008). Pneumatic retinopathy for the repair of retinal detachments: a comprehensive review (1986-2007). Surv Ophthalmol. 53: 443–478.
- Jackson TL, Donachie PH, Sallam A. (2014). United Kingdom National ophthalmology database study of vitreoretinal surgery: report 3, retinal detachment. Ophthalmology. 121: 643–648.
- Soni C, Hainsworth DP, Almony A. (2013). Surgical management of rhegmatogenous retinal detachment: a meta-analysis of randomized controlled trials. Ophthalmology. 120: 1440–1447.
- Bourla DH, Bor E, Axer-Siegel R, Mimouni K, Weinberger D. (2010). Outcomes and complications of rhegmatogenous retinal detachment repair with selective sutureless 25-gauge pars plana vitrectomy. Am J Ophthalmol. 149: 630–634.
- Park SW, Kwon HJ, Kim HY, Byon IS, Lee JE, Oum BS. (2015). Comparison of scleral buckling and vitrectomy using wide angle viewing system for rhegmatogenous retinal detachment in patients older than 35 years. BMC Ophthalmol. 15:1.
- Heimann H, Bartz-Schmidt KU, Bornfeld N. (2007). Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment. A prospective randomized multicenter clinical study. Ophthalmology. 114: 2142–2154.
- Campo RV, Sipperley JO, Sneed SR. (1999). Pars plana vitrectomy without scleral buckle for pseudopakic retinal detachments. Ophthalmology. 106: 1811–1815.
- Tan HS, Oberstein SY, Mura M, Biji HM. (2013). Air versus gas tamponade in retinal detachment surgery. Br J Ophthalmol. 97(1): 80–82
- Zhang H, Li YY, Ma K, Liu NP. (2018). Short-term efficacy of 25G vitrectomy combined with air filling in the treatment of primary perforated retinal detachment. Eye. 27(5): 377–380.
- Liang XM, Jia YH. (2020). Comparison of the efficacy of air and silicone oil filling in the treatment of perforated retinal detachment after 25G vitrectomy. Int J Ophthalmol. 20(4): 711–714.
- Huang HB, Han GJ. (2019). Comparison of the efficacy of 25G and 27G vitrectomy combined with air filling for RRD. Int J Ophthalmol. 19(9): 1602–1604.
- Thompson JT. (1989). Kinetics of intraocular gases: disappearance of air, sulfur hexafluoride, and perfluoropropane after pars plana vitrectomy. Arch Ophthalmol. 107: 687–691.
- Wong RF, Thompson JT. (1988). Prediction of the kinetics of disappearance of sulfur hexafluoride and perfluoropropane. Ophthalmology. 95: 609–613.
- Martinez-Castillo V, Boixadera A, Verdugo A, Garcia-Arumi J. (2005). Pars plana vitrectomy alone for the management of inferior breaks in pseudophakic retinal detachment without facedown position. Ophthalmology. 112(7): 1222–1227.
- Martinez-Castillo VJ, Garcia-Arumi J, Boixadera A. (2016). Pars plana vitrectomy alone for the management of pseudophakic rhegmatogenous retinal detachment with only inferior breaks. Ophthalmology. 123: 1563–1569.
- Zhang Z, Peng M, Wei Y, Jiang X, Zhang S. (2017). Pars plana vitrectomy with partial tamponade of filtered air in rhegmatogenous retinal detachment caused by superior retinal breaks. BMC Ophthalmol. 17:64.
- Chen QY, Tang YX, He YQ, Lin HM, Gao RL, Li MY, Hou JT, Ma HJ, Zhang JL. (2018). Air tamponade in retinal detachment surgery followed by ultra-widefield fundus imaging system. Int J Ophthalmol. 11: 1198–1203.
- Pak KY, Lee SJ, Kwon HJ, Park SW, Byon IS, Lee JE. (2017). Exclusive use of air as gas tamponade in rhegmatogenous retinal detachment. J Ophthalmol. 134: 1948.
- Zhou CD, Qiu QH, Zheng Z. (2015). Air versus gas tamponade in rhegmatogenous retinal detachment with inferior breaks after 23-gauge pars plana vitrectomy: a prospective, randomized comparative interventional study. Retina. 35(5): 886–891.
- Tetsumoto A, Imai H, Hayashida M, Otsuka K, Matsumiya W, Miki A, Nakamura M. (2020). The comparison of the surgical outcome of 27-gauge pars plana vitrectomy for primary rhegmatogenous retinal detachment between air and SF6 gas tamponade. Eye. 34(2): 299–306.
- Yu Y, Zeng L, Yang ZK, Zhu RR, Xue SD, Chen H. (2020). Clinical application and influencing factors of air filling in vitrectomy for perforated retinal detachment. Chinese Journal of Fundus Diseases. 36(8): 605–610.
- Carim MM. (1990). Scleral buckling after failed air injection pneumatic retinopexy. Arch Ophthalmol. 108(1): 11–12.
- Hasegawa Y, Hata Y, Mochizuki Y. (2009). Equivalent tamponade by room air as compared with SF6 after macular hole surgery. Graefes Arch Clin Exp Ophthalmol. 247(11): 1455–1459.
- Jia LY, Zhang YP, Zhou HY, She HC, Cao XS, Gao LQ, Ma K. (2021). Analysis of prognostic factors of high myopia complicated with choroidal detachment type retinal detachment. Eye. 30(1): 42–46.
- Thompson JT. (1989). Kinetics of intraocular gases. Disappearances of air, sulfur hexafluoride, and perfluoropropane after pars plana vitrectomy. Arch Ophthalmol. 107(5): 687–691.
- Yang J Y, He T, Xing YQ. (2019). Incidence and related factors of early intraocular hypertension after vitrectomy for retinal detachment. Medical J Wuhan Univ. 39(3): 488–491.
- Huang LL, Song Y, Wu Y, Sun ZM. (2014). Clinical characteristics of vitrectomy in the treatment of high myopia retinal detachment. J Clin Ophthalmol. 22(5): 403–405.
- Cheng YH, Wang H, Li B, Ji M, Shi Q, Qi Y, Hu YG, Xie AM, Pei C. (2020). Vitrectomy with air tamponade for surgical repair of rhegmatogenous retinal detachment by eye position guided fluid-air exchange. Int J Ophthalmol. 13(9): 1417–1422.
Citation: Zhuang Jingjing, He Yongning, Luo wei and Tang Ruifei. (2023). Short-term Efficacy of Vitrectomy Combined with Air Tamponade on Rhegmatogenous Retinal Detachment with Inferior Holes. Journal of Ophthalmology and Vision Research 5(1).
Copyright: © 2023 He Yongning. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
