Case Report
Volume 3 Issue 1 - 2021
Excision of large Intraconal cavernous hemangiomas presented superolateral to the optic nerve through a planned combined superolateral fornix-based conjunctival flap and lateral canthotomy (CF & LC).
1Professor of Ophthalmology, Alexandria University, Egypt
2Associate Professor of Ophthalmology, Alexandria University, Egypt
2Associate Professor of Ophthalmology, Alexandria University, Egypt
*Corresponding Author: Hesham A Ibrahim, Professor of Ophthalmology, Alexandria University, Egypt.
Received: June 01, 2021; Published: June 14 , 2021
Abstract
Purpose: to describe a surgical approach that allows the excision of a huge localized well encapsulated intraconal lesion located superolateral to the optic nerve without the need for craniotomy or lateral orbitotomy
Methods: This is a prospective interventional case series. The study included three consecutive cases who had a large intraconal cavernous hemangioma (28 mm-32 mm in length), superolateral to the optic nerve and who underwent surgical removal through a planned combined superolateral CF & LC. Preoperative and postoperative clinical assessment were documented with clinical photographs, and radiological investigations. Visual acuity, ocular motility, pupillary reaction, fundus picture, eyelid position and excursion were documented. Postoperative follow-up was carried out for at least 6-months.
Results: Surgical time was within one hour for all patients. Following the 1st postoperative week, patients had minimal postoperative edema, preserved visual acuity, normal pupil size and reaction, full extra ocular motility, recovered eyelid excursion, and upper eyelid position.
Conclusions: The planned combined superolateral fornix-based CF & LC approach allows the excision of huge encapsulated well-localized intraconal lesion presenting superolateral to the optic nerve with low morbidity and rapid recovery. Such lesions would otherwise be removed through a more extensive craniotomy or lateral orbitotomy.
Keywords: Cavernous hemangioma; Lateral canthotomy; Orbitotomy; Orbital diseases; Proptosis
Introduction
With the development of modern diagnostic radiology and the ability to reach a preoperative collaborative accurate diagnosis, increasingly surgeons perform minimally invasive orbital surgery for a well-localized encapsulated orbital lesion [1]. The need for wide exploratory orbitotomy and craniotomy for such lesions are becoming less acceptable [2-4].
The transconjunctival approach provides a direct access to the intraconal space. Unlike the commonly performed lower eyelid fornix incision, an upper fornix incision is not possible because it transfixes important structures; the levator muscle, the lacrimal gland, and its lacrimal ductules. [5,6]
In this study, the authors describe a planned combined fornix based superolateral CF & LC approach that creates a safely extendable surgical window that allows the removal of huge well-encapsulated masses presenting superolateral to the optic nerve. Such masses would otherwise be removed through a more extensive craniotomy or lateral orbitotomy.
Methods
The local Institutional Review Board approved the study protocol. The Declaration of Helsinki tenets were followed. Participants provided written informed consent for patients’ information and images to be published. All figures included in this work do not show patients identity.
This is a prospective interventional case series of three consecutive patients who had: gradual progressive disfiguring axial proptosis, deterioration of visual acuity, and/or double vision with well-defined large deep intraconal lesions on CT or MRI. The provided radiological diagnosis was: intraconal cavernous hemangioma presented superolateral to the optic nerve with a tumor length of 28mm or more and width of 22mm or more. Tumors occupied most of the orbit and extended deep behind the coronal plane midway between the posterior pole of the globe and the orbital apex. These patients underwent tumor excision through a planned combined superolateral fornix-based CF & LC approach. The study included assessment of preoperative and postoperative visual acuity, ocular motility, pupillary reaction, fundus picture, eyelid position and excursion, preoperative photographs, radiological investigations, and postoperative photographic documentation.
Surgical procedure
All surgeries were performed under general anesthesia by a single surgeon (HAI). Lateral canthotomy was performed just to allow the upper eyelid to be retracted beyond the superior orbital margin. A wire speculum was inserted. Under the surgical microscope, a 5-clock-hour peritomy was performed. The peritomy extended from the medial edge of the superior rectus tendon to the inferior edge of the lateral rectus.
All surgeries were performed under general anesthesia by a single surgeon (HAI). Lateral canthotomy was performed just to allow the upper eyelid to be retracted beyond the superior orbital margin. A wire speculum was inserted. Under the surgical microscope, a 5-clock-hour peritomy was performed. The peritomy extended from the medial edge of the superior rectus tendon to the inferior edge of the lateral rectus.
Two radial incisions at the edges of the peritomy were performed to reach the corresponding fornix. The radial incision inferior to the lateral rectus was fashioned obliquely so that it reaches the lateral fornix at the inner conjunctival incision of the lateral canthotomy. Figure 1A
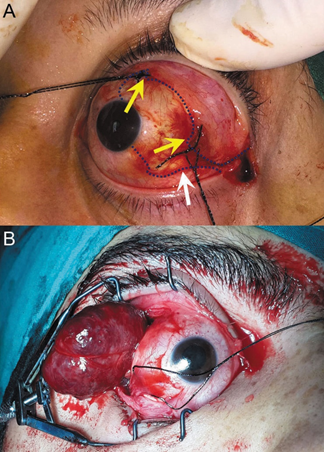
Figure 1: A: conjunctival peritomy in the left eye extending from 11 to 4 O’clock. Yellow arrows show the edges of the conjunctival flap. The white arrow shows the lower radial incision is fashioned at a different level from the inner wound of the lateral canthotomy. B: peritomy in the right eye extends from 1 to 8 o’clock with tumor delivered between the lateral and superior recti
The two limbal angles of the superolateral bulbar conjunctival flaps were marked with 4-0 silk sutures so that they can be recognized and re-sutured accurately at the end of surgery. Figure 1A
A 4-0 silk traction suture was placed under the lateral and superior recti tendons. The wire speculum was removed. The conjunctival flap was reflected onto the under surface of the upper eyelid and kept off the surgical field, anterior to the tarsus by malleable retractors.
The traction sutures on the recti were pulled inferonasally by the assistant to expose the tenon’s capsule between the lateral and superior recti muscles. Blunt dissection was used to open the tenon with the tip of Wescott scissors. A surgical window was then created to reach the intraconal space above and lateral to the optic nerve by splitting the blades of an artery forceps. Once the anterior surface of the mass was exposed, a Freer periosteal elevator was used to sweep around it and gently dissect it from surrounding structures. Once the mass was freed from the surroundings, the lesion was scooped out to be delivered between the recti muscles. Maintaining a gentle, slow but firm constant forward levering pressure on the mass with two opposing Freer periosteal elevators allowed the mass to slowly remodel its shape out through the surgical window. Figure 1B After lesion delivery, the wire speculum was reinserted, and the procedure was completed under the surgical microscope. The conjunctiva marked edges were identified and re-sutured back to the limbus with 8-0 vicryl sutures. The lateral cantholysis was repaired with 5-0 vicryl sutures. A combination of steroid antibiotic eye ointment, Tobradex (Alcon-Couvreur, Puurs (Belgium) (Novartis) was installed. A pressure bandage was applied. The specimen was sent for pathological examination. Tobradex eye ointment was used twice daily for 2 weeks. The lateral canthal sutures were removed after one week. Patients were followed up after one week, one month, three months and 6 months. Visual acuity, ocular motility, upper eyelid excursion, eyelid position, the presence of lateral canthal scar, ocular irritation, dry eye manifestations, or complications of conjunctival healing were reported.
Results
The tumor length in the three cases measured 35mm in case one, 30mm in case 2, and 28mm in case 3. All masses occupied most of the orbit, pushing the optic nerve down and in. Surgical time was below 60 minutes for all patients. Postoperative edema, levator function, and ocular motility had resolved by the 1st postoperative week and documented with photographs. Figures 2-4 Pathological examination of the tissue biopsy confirmed the radiological diagnosis of cavernous hemangioma in all cases. All three patients achieved full and rapid recovery with no intra-operative or postoperative complications. No patient suffered from any deterioration of vision or persistent double vision. All patients had normal postoperative pupil size and reaction. Full extraocular motility, eyelid excursion, and upper eyelid position was preserved. No patient experienced a dry eye or significant outer canthal or conjunctival scarring.

Figure 2: Patient #1
A: 36-year-old male suffering from progressive proptosis and deteriorating vision MRI for patient # 1; a) T1 WI Isointense with hypointense pseudo capsule b & c) T2 WI: Hyperintense with septation. d) T1 WI with contrast and Fat Suppression: Patchy central with delayed homogeneous enhancement. Lesion size was 32.5mm long and 22.1mm wide B: one-week postoperative visit. Nearly full recovery was achieved. Normal recti and levator function
A: 36-year-old male suffering from progressive proptosis and deteriorating vision MRI for patient # 1; a) T1 WI Isointense with hypointense pseudo capsule b & c) T2 WI: Hyperintense with septation. d) T1 WI with contrast and Fat Suppression: Patchy central with delayed homogeneous enhancement. Lesion size was 32.5mm long and 22.1mm wide B: one-week postoperative visit. Nearly full recovery was achieved. Normal recti and levator function
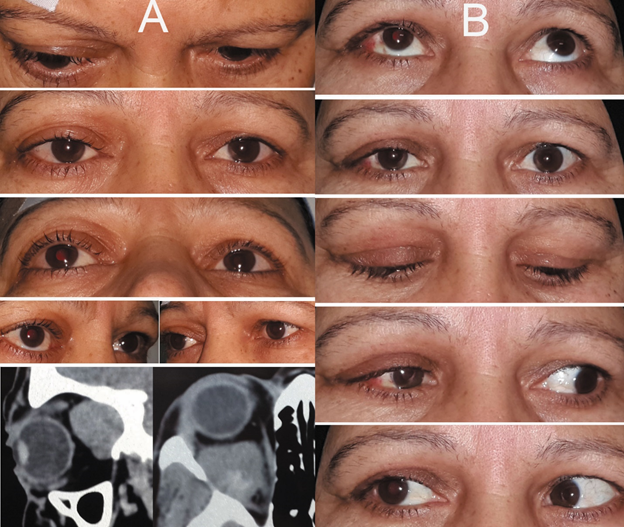
Figure 3: Patient #2
A: 49-years old female patient with slowly progressive right proptosis. She was concerned with the disfigurement induced by the mass. CT scan orbit shows Iso-dense right large superolateral intraconal mass, with bone remodeling and patchy enhancement that started centrally. B: one-week postoperative visit, the patient has achieved full recovery with intact levator and recti function.
A: 49-years old female patient with slowly progressive right proptosis. She was concerned with the disfigurement induced by the mass. CT scan orbit shows Iso-dense right large superolateral intraconal mass, with bone remodeling and patchy enhancement that started centrally. B: one-week postoperative visit, the patient has achieved full recovery with intact levator and recti function.

Figure 4: Patient #3
A: Preoperative photographs and CT of a 60-years-old male patient with progressive proptosis and 3.2mm x 2.5mm large well demarcated mass isodense with patchy enhancement. B; Six-month postoperative follow-up with intact levator action and extra-ocular muscle function.
A: Preoperative photographs and CT of a 60-years-old male patient with progressive proptosis and 3.2mm x 2.5mm large well demarcated mass isodense with patchy enhancement. B; Six-month postoperative follow-up with intact levator action and extra-ocular muscle function.
Discussion
The lower fornix incision combined with lateral canthotomy (Lower eyelid swinging) is a well-known commonly practiced approach for lower orbital lesion either intraconal, extraconal, or sub-periosteal. [5] Structures that are severed during such approach often do not jeopardize lower eyelid or adnexal function. The lower eyelid fornix approach is not totally applicable to the upper eyelid, otherwise vital structures such as the levator palpebrae superioris and the lacrimal gland with its ductules could be damaged. The planned combined superolateral fornix-based CF & LC approach creates a safely expandable surgical window to the superolateral intraconal space.
The special characteristics of certain orbital lesions such as cavernous hemangioma, fibroma, or schwannoma are advantageous in the way they can be approached. These lesions are well encapsulation and are easily separable from the surrounding structures. Their shape can be remodeled with constant firm pressure and thus can be squeezed out from the orbit without disintegration.
The gold standard approach to excise such lesions when they are huge and extending deep behind the posterior pole of the globe is through craniotomy or lateral orbitotomy. In 1989 McNab AA and Wright JE reported 85 patients who underwent surgery for cavernous hemangioma. They classified the depth of the lesions within the orbit into 3 zones. Only lesions anterior to the posterior pole of the globe or located in the extraconal space were suitable for anterior orbitotomy. In their series only 2 patients had superotemporal location in the posterior orbit and 9 in the mid-orbital plane. All these patients underwent either lateral orbitotomy or craniotomy. According to their classifications, lesions with a similar large size and posterior orbital location as those presented in this series would have had undergone lateral orbitotomy or craniotomy. [6]
Goldberg AR et al. in 2014, described their experience in performing orbitotomy without marginotomy as a minimally invasive procedure. [1] They had five cases of tumor size of 28 mm or larger in all quadrants but they didn’t indicate how many of these five cases were superotemporal to the optic nerve. They performed an upper eyelid skin crease incision to excise intraconal superolateral lesions. To reach the intraconal space, they opened the intermuscular septum and displaced the levator muscle medially [1].
The planned combined superolateral fornix-based CF & LC approach provides a wide, safely expandable surgical window. If compared with the upper eyelid crease incision approach, it provides direct access to the intraconal space, so there is no need to manipulate the levator muscle or to retract it medially. In case of huge lesions, it is safe to widen the surgical window laterally unhindered by the lacrimal secretory system, while in the upper eyelid crease incision approach, the mass delivered above the levator would be medial to the lacrimal gland. For moderate size masses this may not cause significant damage, but with huge masses such as those presented in this series, widening the surgical window can induce injury to the lacrimal ductules on their way to the upper fornix or may require performing more complicated orbital surgery like lateral orbitotomy. Lateral canthotomy is less likely to produce a conceivable scar than that produced by laterally extending the upper eye lid crease incision. The recti muscles in the extended upper eyelid crease incision approach would not be specifically visualized and if widening dissection was required, they can potentially be damaged, while with the planned combined superolateral fornix-based CF & LC approach the use of traction on the recti muscles serves two purposes; it allows visualization of the recti muscles which avoids muscle injury during tumor dissection, and it opens the surgical space. This direct access consumes less theater time, permits minimal tissue disruption, has less morbidity, and achieves rapid recovery.
A cryo-probe or a 3-0 silk traction suture could have been helpful to bring the tumor forward, but the authors preferred not to do that because the freely dissected lesion can be delivered by applying a gentle, slow but firm forward levering action (scooping). This would allow slow remodeling of the tumor. Traction sutures passing into the lesion can cheese-wire and jeopardize the integrity of the mass.
This technique theoretically allows an intraoperative change of plan. If a wider surgical window is required, performing upper cantholysis or a wider marginotomy can still be performed through the lateral canthotomy [7]. Although all presented cases had lesions with a size larger than that of the globe and were located deep in the posterior orbit, the authors was not obliged to change surgical plans in any of these cases. Figures 2A, 3A & 4
Other minimally invasive surgical procedures have been described in the literature to obtain access to the superior intraconal space. S Hamed-Azzamet et al. in 2017, described a technique to reach the superolateral intraconal and extraconal spaces through a lateral canthotomy without cantholysis which was described as sufficient to get a biopsy or excise a small lesion. [8] S Hamed-Azzamet technique has the advantage of not disturbing the conjunctiva but may not be suitable for large posteriorly located masses similar to those presented in this series.
Jin-Wei Cheng et al. In 2007, described a trans-conjunctival approach without a lateral cathotomy [9]. Kyong Jin Cho et Al in 2010, published a trans conjunctival excision of cavernous hemangioma in 9 patients from all quadrants. They needed to disinsert one of the recti muscles and had to perform lateral canthotomy in 2 cases [10]. This may be similar to the planned combined superolateral fornix-based CF & LC approach, but they performed it as additional unplanned step and provided no further surgical details.
The disadvantages of the CF & LC approach are the need to perform two opposing conjunctival incisions; the lateral radial incision of the conjunctiva and the inner wound of the lateral canthotomy which carries the risk for conjunctival adhesion. However, these two incisions are not fashioned at the same horizontal level which guard against symblepharon, and we have not encountered this complication in any of our patients so far. Another disadvantage is the need for peritomy and lateral canthotomy. The amount of conjunctival dissection is equal to that required for two-muscle strabismus surgery and much less than that required for buckle insertion during retinal surgery. Marking the conjunctival angles with sutures would ensure proper tissue realignment and healing. Lateral canthotomy is a commonly practiced oculoplastic procedure. It is repaired by direct tissue re-approximation, which does not induce any lateral canthal distortion or scars.
The number of patients presented in this series is small, but this is because the location, size, and pathology of such lesions qualified for this technique is relatively rare. The biggest series in the literature describing similar lesion size and location are less than 5 cases [1, 7].
Conclusions
The planned combined superolateral fornix-based CF & LC approach is a minimally invasive procedure that gives a direct, expandable surgical access to the deep superolateral intraconal compartment, has low morbidity and rapid recovery. It does not compromise patient’s safety or the surgeon’s ability to adopt a change in the intraoperative surgical plan.
Declarations
Data Availability
Availability of data and materials: All original data materials are available. All cases were documented with photographs and most of these are included in the figures. All original photographs with dates can be provided to the reviewers to prove the early convalescence and the low morbidity of such approach.
Availability of data and materials: All original data materials are available. All cases were documented with photographs and most of these are included in the figures. All original photographs with dates can be provided to the reviewers to prove the early convalescence and the low morbidity of such approach.
Animal Research (Ethics)
No animals were used in this research
No animals were used in this research
Consent to Participate (Ethics)
Informed consent was obtained from all individual participants included in the study.
Informed consent was obtained from all individual participants included in the study.
Consent to Publish (Ethics)
Patients signed informed consent regarding publishing their data and photographs
Patients signed informed consent regarding publishing their data and photographs
Clinical Trials Registration: The Institutional Review Board at the University of Alexandria, Egypt, approved the study protocol. The Declaration of Helsinki tenets were followed.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Hesham Ali Ibrahim and Heba Nabil Sabry. The first draft of the manuscript was written by Hesham Ali Ibrahim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Hesham Ali Ibrahim and Heba Nabil Sabry. The first draft of the manuscript was written by Hesham Ali Ibrahim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflict of Interest/Financial disclosure
The authors have no relevant financial or nonfinancial interests to disclose.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
The authors have no financial or proprietary interests in any material discussed in this article.
The authors have no relevant financial or nonfinancial interests to disclose.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
The authors have no financial or proprietary interests in any material discussed in this article.
Funding
The authors did not receive support from any organization for the submitted work.
No funding was received to assist with the preparation of this manuscript.
No funding was received for conducting this study.
No funds, grants, or other support was received.
The authors did not receive support from any organization for the submitted work.
No funding was received to assist with the preparation of this manuscript.
No funding was received for conducting this study.
No funds, grants, or other support was received.
Ethics approval: Approval was obtained from the ethics committee of The Institutional Review Board at the University of Alexandria, Egypt. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
References
- Goldberg RA, Rootman DB, Nassiri N, Samimi DB, Shadpour JM. (2014). Orbital Tumors Excision without Bony Marginotomy under Local and General Anesthesia Journal of Ophthalmology. 2014. Published online Apr 14
- Scheuerle AF, Steiner HH, Kolling G, Kunze S, Aschoff A. (2004). Am J Ophthalmol. Treatment and long-term outcome of patients with orbital cavernomas. Aug; 138(2): 237-44
- McNab AA. (2005). Am J Ophthalmol. Treatment and long-term outcome of patients with orbital cavernomas. Apr; 139(4): 751-2
- Goldberg RA. (2005). Am J Ophthalmol. Treatment and long-term outcome of patients with orbital cavernomas. Apr;139(4): 749-50
- McCord CD Jr, Moses JL. (1979). Exposure of the inferior orbit with fornix incision and lateral canthotomy. Ophthalmic Surg 10:53-63
- McNab AA, Wright JE. (1989). Cavernous haemangioma of the orbit. Aust N Z J Ophthalmol 17:337-45.
- Rootman J, Stewart B, Golbert RA (eds). (2014). Orbital Surgery a Conceptual Approach. Wolters Kluwer, Lippincott Williams & Wilkins: Philadelphia.
- Hamed-Azzam S, Verity DH, Rose GE. (2017). Lateral canthotomy orbitotomy: a rapid approach to the orbit. Eye. September. 173-7
- Cheng J, Wei R, Cai J. Li Y. (2008). Transconjunctival orbitotomy for orbital cavernous hemangiomas. Can J Ophthalmol. 43: 234–8
- Cho KJ, Paik J, Yang S. (2010). Surgical Outcomes of Transconjunctival Anterior Orbitotomy for Intraconal Orbital Cavernous Hemangioma. Korean J Ophthalmol 24(5): 274-278
Citation: Hesham A Ibrahim and Heba N Sabry. (2021). Excision of large Intraconal cavernous hemangiomas presented superolateral to the optic nerve through a planned combined superolateral fornix-based conjunctival flap and lateral canthotomy (CF & LC). Journal of Ophthalmology and Vision Research 3(1).
Copyright: © 2021 Hesham A Ibrahim. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
