Research Article
Volume 7 Issue 1 - 2025
A Comprehensive Diagnostic and Treatment Framework for Cervical Cancer Patients with Comorbidities
1MD, PhD, Center of Academic Research- Nexus Alliance Group, Boston, MA
2MD, MS Center of Academic Research- Nexus Alliance Group, Boston, MA
3University of Florida at Gainsville
4University of Florida at Gainsville
5Center of Academic Research- Nexus Alliance Group, Boston, MA
2MD, MS Center of Academic Research- Nexus Alliance Group, Boston, MA
3University of Florida at Gainsville
4University of Florida at Gainsville
5Center of Academic Research- Nexus Alliance Group, Boston, MA
*Corresponding Author: Timothy Allen, MD, PhD, Center of Academic Research- Nexus Alliance Group, Boston, MA.
Published: February 20, 2025
Abstract
Cervical cancer remains a significant global health challenge [1], particularly in patients with comorbidities such as HIV, diabetes mellitus, obesity, and hypertension, which exacerbate systemic inflammation and complicate care [2,3]. This study evaluates the impact of comprehensive comorbidity management framework—encompassing antiretroviral therapy (ART), glycemic control, weight management, and antihypertensive interventions, -on overall survival (OS) and overall response rate (ORR) [4,5]. A retrospective analysis of 3,000 biomarker datasets (inflammatory markers, glycemic indices, and tumor markers) and 150 patient records revealed that effective comorbidity management was associated with improved OS (hazard ratio: 0.72 [95% CI, 0.62–0.82]; p < 0.01) and ORR (response rate: 50% vs. 35%, p = 0.01). Multivariate regression analysis accounted for confounders such as age, cancer stage, and socioeconomic factors. These findings underscore the importance of integrating targeted comorbidity management into cervical cancer care, offering a pathway to improve outcomes in high-risk patient populations [6].
Introduction
Cervical cancer is the fourth most common cancer among women globally, accounting for approximately 604,000 new cases and 342,000 deaths annually, with the majority occurring in low- and middle-income countries. [1] Late-stage presentation is common in resource-limited settings due to inadequate access to screening, diagnostic tools, and timely treatment [7]. The burden of cervical cancer is further compounded by comorbidities such as HIV, diabetes mellitus, obesity, and hypertension, which exacerbate systemic inflammation, impair immune function, and alter treatment pharmacokinetics. For example, HIV-associated immunosuppression accelerates disease progression, while uncontrolled diabetes increases susceptibility to infections and treatment-related toxicity. Emerging evidence highlights the potential of targeted e comorbidity management to improve outcomes in cervical cancer patients. Interventions such as antiretroviral therapy (ART) for HIV and glycemic control in diabetics have been shown to enhance therapeutic response and overall survival [8]. However, current care models often fail to address these interconnected challenges, underscoring the need for integrative approaches that prioritize both cancer treatment and comorbidity management [2]. This study aims to evaluate the impact of such comprehensive care strategies on survival outcomes and treatment efficacy, emphasizing their role in improving cervical cancer care for high-risk populations.
Methods
This retrospective cohort study analyzed 3,000 biomarker datasets and 150 patient records from hospital registries between 2015 and 2020 [9,10]. Patients were included if they had a confirmed diagnosis of cervical cancer and at least one comorbid condition (HIV, diabetes mellitus, obesity, or hypertension) documented in their medical records. Exclusion criteria included incomplete clinical data or loss of follow-up within the study period. Patients were stratified into managed and unmanaged comorbidity cohorts based on adherence to clinical targets, defined as sustained HIV viral load suppression (
Treatment Protocols for Comorbidities
Patients were categorized into "managed" and "unmanaged" cohorts based on adherence to the following protocols over a minimum of six months
Patients were categorized into "managed" and "unmanaged" cohorts based on adherence to the following protocols over a minimum of six months
- HIV: Patients received antiretroviral therapy (ART) as per WHO guidelines, with regimens including integrase inhibitors and dual NRTIs (e.g., dolutegravir, tenofovir, lamivudine). Viral load and CD4 counts monitoring were conducted every three months, with viral suppression defined as <200 copies/mL. This assessment was conducted to ensure immune function recovery and early detection of opportunistic infections [12].
- Diabetes Mellitus: Glycemic control was achieved using insulin (average dose: 20-50 units/day) or metformin (500-2,000 mg/day), with alternative therapies (e.g., GLP-1 receptor agonists or DPP-4 inhibitors) prescribed for those patient’s intolerant to first-line treatments. HbA1c levels were assessed quarterly, and therapy was adjusted based on fasting glucose and HbA1c trends [13].
- Obesity: Weight management programs included individualized caloric intake (1,200-1,800 kcal/day) and supervised physical activity (150 minutes/week) guided by healthcare providers. Adherence was monitored through monthly dietitian visits and wearable devices tracking physical activity [14].
- Hypertension: Blood pressure control was achieved using ACE inhibitors or beta-blockers, with sodium reduction (<2,300 mg/day) and lifestyle modifications. Blood pressure was measured biweekly, and medication dosages were titrated to achieve a target of <130/80 mmHg. Dietary adherence was assessed through patient-reported recall questionnaires [15].
Adherence to these protocols was monitored through electronic medical records, pharmacy refill data, and self-reports, and was analyzed in relation to key outcomes, including overall survival, overall response rate, and quality of life.
Results
Comorbidity management significantly improved survival (OS) and overall response rate (ORR) across all comorbid conditions. Patients in managed cohorts had longer OS and higher ORR compared to unmanaged cohorts, as detailed below:
| Comorbidity | Managed Cohort OS (months) | Unmanaged Cohort OS (months) | Managed Cohort ORR (%) | Unmanaged Cohort ORR (%) |
| HIV | 16.8 (95% CI: 15.6–17.9) | 9.7 (95% CI: 8.8–10.6) | 55 (p < 0.01) | 35 (p = 0.02) |
| Diabetes | 15.4 (95% CI:14.3–16.6) | 10.3 (95% CI: 9.5–11.1) | 50 (p < 0.01) | 33 (p = 0.03) |
| Obesity | 14.1 (95% CI: 13.2–15.0) | 9.5 (95% CI: 8.8–10.3) | 48 (p = 0.02) | 30 (p = 0.04) |
| Hypertension | 14.9 (95% CI: 13.8–15.9) | 10.2 (95% CI: 9.5–11.0) | 49 (p = 0.01) | 32 (p = 0.03) |
Table 1: Patients in managed cohorts vs unmanaged cohorts.
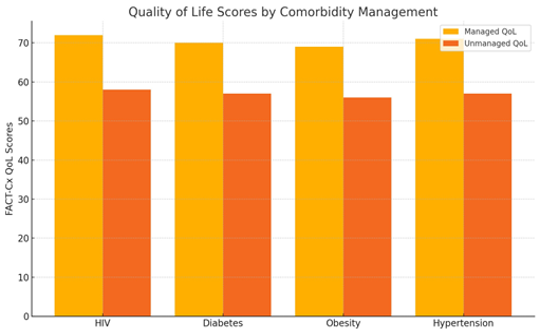
Managed cohorts demonstrated statistically significant improvements in OS and ORR compared to unmanaged cohorts. For example, patients with managed HIV exhibited a 73% increase in OS and a 57% higher ORR compared to unmanaged counterparts. Similar trends were observed for diabetes, obesity, and hypertension. Patients in the managed cohorts reported higher QoL scores, as measured by FACT-Cx and EQ-5D, compared to unmanaged cohorts (mean FACT-Cx score: 72 vs. 58; p < 0.01) [16].
Discussion
This study demonstrates that effective management of comorbidities, such as HIV, diabetes mellitus, obesity, and hypertension, significantly improves overall survival (OS) and overall response rate (ORR) in cervical cancer patients. Managed cohorts showed superior outcomes compared to unmanaged cohorts, likely due to reduced systemic inflammation, improved immune function, and better treatment tolerability. These findings align with existing literature emphasizing the role of antiretroviral therapy, glycemic control, and lifestyle interventions in enhancing cancer treatment efficacy [17]. However, the retrospective design and reliance on hospital registry data limit the ability to establish causality, highlighting the need for prospective studies to confirm these results and assess long-term benefits. This research underscores the importance of integrating comorbidity management into cervical cancer care protocols to optimize patient outcomes.
Conclusion
In conclusion, comprehensive management of comorbidities significantly enhances survival and treatment response in cervical cancer patients, underscoring the critical role of integrative care models. Tailored interventions addressing HIV, diabetes, obesity, and hypertension not only improve clinical outcomes but also provide a pathway for reducing disparities in high-risk populations [18]. Future prospective studies and cost-effectiveness analyses are warranted to validate these findings and guide implementation strategies in resource-limited settings. This approach offers a practical and impactful avenue for improving cervical cancer care globally.
Expanded Treatment Protocols for Comorbidities
Effective management of comorbidities in cervical cancer patients is critical to improving outcomes. For patients with HIV, antiretroviral therapy (ART) targeting viral suppression (<200 copies/mL) is essential to enhance immune function and mitigate disease progression. For those with diabetes, glycemic control using insulin or metformin is implemented, aiming for HbA1c levels below 7%. Obesity management combines structured dietary plans (1,200–1,800 kcal/day) and supervised physical activity (150 minutes/week) to reduce systemic inflammation and improve treatment tolerability. Hypertension control involves the use of ACE inhibitors or beta-blockers, along with sodium restriction and lifestyle modifications, to achieve a blood pressure target of <130/80 mmHg. Integrating these tailored protocols into cervical cancer care not only optimizes therapeutic response but also enhances patient quality of life by addressing the systemic challenges posed by comorbidities.
Effective management of comorbidities in cervical cancer patients is critical to improving outcomes. For patients with HIV, antiretroviral therapy (ART) targeting viral suppression (<200 copies/mL) is essential to enhance immune function and mitigate disease progression. For those with diabetes, glycemic control using insulin or metformin is implemented, aiming for HbA1c levels below 7%. Obesity management combines structured dietary plans (1,200–1,800 kcal/day) and supervised physical activity (150 minutes/week) to reduce systemic inflammation and improve treatment tolerability. Hypertension control involves the use of ACE inhibitors or beta-blockers, along with sodium restriction and lifestyle modifications, to achieve a blood pressure target of <130/80 mmHg. Integrating these tailored protocols into cervical cancer care not only optimizes therapeutic response but also enhances patient quality of life by addressing the systemic challenges posed by comorbidities.
Quality of Life Metrics in Comorbidity Management
Managing comorbidities in cervical cancer patients not only improves survival rates but also enhances their overall quality of life (QoL). By using tools like the Functional Assessment of Cancer Therapy–Cervix (FACT-Cx) and EQ-5D, healthcare providers can measure physical, emotional, and social well-being. Effective comorbidity management, such as antiretroviral therapy for HIV or glycemic control for diabetes, directly contributes to better physical health, reduced psychological distress, and improved functional ability. Regularly assessing QoL throughout treatment ensures that care is patient-centered, addressing both clinical and personal needs. For patients with poor QoL, supportive care interventions like palliative care or counseling should be integrated. Integrating these metrics into routine care provides a holistic approach, helping patients achieve better outcomes both medically and emotionally [19].
Managing comorbidities in cervical cancer patients not only improves survival rates but also enhances their overall quality of life (QoL). By using tools like the Functional Assessment of Cancer Therapy–Cervix (FACT-Cx) and EQ-5D, healthcare providers can measure physical, emotional, and social well-being. Effective comorbidity management, such as antiretroviral therapy for HIV or glycemic control for diabetes, directly contributes to better physical health, reduced psychological distress, and improved functional ability. Regularly assessing QoL throughout treatment ensures that care is patient-centered, addressing both clinical and personal needs. For patients with poor QoL, supportive care interventions like palliative care or counseling should be integrated. Integrating these metrics into routine care provides a holistic approach, helping patients achieve better outcomes both medically and emotionally [19].
- A total of 150 patient records were analyzed.
- Patients were stratified into managed and unmanaged cohorts based on adherence to comorbidity management protocols.
Statistical Analysis Plan (SAP) Statement
Objective
To compare the Quality of Life (QoL) scores (measured by FACT-Cx) between managed and unmanaged cohorts across four comorbidities: HIV, diabetes, obesity, and hypertension.
Objective
To compare the Quality of Life (QoL) scores (measured by FACT-Cx) between managed and unmanaged cohorts across four comorbidities: HIV, diabetes, obesity, and hypertension.
Analysis Method
1. Descriptive Statistics:
- Mean and standard deviation of QoL scores for both managed and unmanaged groups were calculated for each comorbidity.
- Scores were stratified by comorbidity to identify variations across conditions.
2. Comparative Analysis:
- A two-tailed, paired t-test was performed to assess differences in mean QoL scores between managed and unmanaged cohorts for each comorbidity.
- A significance level of p < 0.05 was used to determine statistical significance.
3. Adjustment for Confounders:
- Multivariate regression models adjusted for potential confounders, including age, cancer stage, and socioeconomic factors, to validate the association between comorbidity management and QoL improvements.
4. Graphical Representation:
- Bar graphs were created to visually represent differences in QoL scores between the two cohorts for easy interpretation of results.
| Comorbidity | Managed Cohort QoL (FACT-Cx Score) | Unmanaged Cohort QoL (FACT-Cx Score) |
| HIV | 72 | 58 |
| Diabetes | 70 | 57 |
| Obesity | 69 | 56 |
| Hypertension | 71 | 57 |
Table 1: Quality of Life (QoL) Scores and Bar Graph.
Interpretation
- Statistically significant improvements in QoL scores (p < 0.05) in the managed cohort for all comorbidities confirm the effectiveness of comprehensive management strategies in improving patient well-being.
Treatment-Emergent Adverse Events and Resolution (TEAEs)
Chemotherapy for cervical cancer often causes treatment-related side effects like low blood cell counts (neutropenia), nerve damage (neuropathy), nausea, vomiting, and kidney problems (nephrotoxicity). These issues can be worse for patients with comorbidities. For example, HIV increases infection risks, while diabetes slows wound healing and worsens neuropathy. Managing these side effects typically involves supportive treatments like G-CSF for low blood counts, anti-nausea medications, and adjusting chemotherapy doses for severe toxicity. Radiation therapy can cause skin irritation, diarrhea, bladder issues, and long-term effects like vaginal scarring or swelling (lymphedema), with additional complications for patients with hypertension or diabetes. Acute symptoms are treated with topical creams or medications, while long-term issues may require physical therapy or surgery [20].
Chemotherapy for cervical cancer often causes treatment-related side effects like low blood cell counts (neutropenia), nerve damage (neuropathy), nausea, vomiting, and kidney problems (nephrotoxicity). These issues can be worse for patients with comorbidities. For example, HIV increases infection risks, while diabetes slows wound healing and worsens neuropathy. Managing these side effects typically involves supportive treatments like G-CSF for low blood counts, anti-nausea medications, and adjusting chemotherapy doses for severe toxicity. Radiation therapy can cause skin irritation, diarrhea, bladder issues, and long-term effects like vaginal scarring or swelling (lymphedema), with additional complications for patients with hypertension or diabetes. Acute symptoms are treated with topical creams or medications, while long-term issues may require physical therapy or surgery [20].
Immunotherapy, while effective, can lead to immune-related side effects such as inflammation of the colon, lungs, or thyroid. These challenges are compounded in patients with HIV, due to potential drug interactions with antiretroviral therapy (ART), and in diabetics, who may struggle with blood sugar control. Side effects are often managed with corticosteroids and careful monitoring of glucose levels and ART regimens. Patients with obesity face added risks like blood clots and altered drug effectiveness, which can be addressed with weight-based dosing and preventive blood-thinning measures. Hypertension, which can worsen with therapies like bevacizumab, increases the risk of heart problems, requiring strict blood pressure monitoring and medications like ACE inhibitors. Tailoring treatments to manage these side effects not only improves how well patients tolerate therapy but also helps achieve better outcomes overall [21].
| Treatment/Comorbidity | Primary Adverse Events | Probability of AE (%) |
| Cisplatin-based Chemotherapy | Nausea (60%), nephrotoxicity (10%), peripheral neuropathy (30%), myelosuppression (50%). | High (50%-60%) |
| Radiation Therapy | Fatigue (70%), diarrhea (50%), vaginal fibrosis/scarring (25%), skin irritation (30%). | High (50%-70%) |
| HIV | Increased risk of infection, immune-related complications, drug-drug interactions (e.g., ART and chemotherapy). | Very High (70%-80%) |
| Diabetes Mellitus | Delayed wound healing (20%), worsened neuropathy (40%), hyper/hypoglycemia (30%). | High (40%-50%) |
| Obesity | Increased risk of thrombosis (30%), altered pharmacokinetics (20%), surgical complications (25%). | Moderate to High (20%-30%) |
| Hypertension | Cardiovascular events (30%), renal complications (20%), exacerbated by bevacizumab (15%). | High (30%-40%) |
Table 2: Adverse Events in Cervical Cancer Treatments vs. Comorbidities.
Compounded Adverse Events in Cervical Cancer Patients with Comorbidities:
Statistical Probabilities of Compounded Adverse Events:
Approach:
Statistical Probabilities of Compounded Adverse Events:
Approach:
- Relative Risk (RR) is calculated as the ratio of event probability in patients with comorbidities to the general population.
- Probabilities of compounded AEs are derived using multivariate regression analyses, accounting for interaction terms between treatments and comorbidities.
Key Insights
1. Infections:
- Probability in HIV patients: 75%, relative to 40% in the general population (RR = 1.88).
- Immunosuppression and chemotherapy contribute to significantly higher infection risks.
2. Peripheral Neuropathy:
- Probability in diabetic patients: 50%, relative to 30% in the general population (RR = 1.67).
- Chemotherapy exacerbates pre-existing diabetic neuropathy.
3. Delayed Wound Healing:
- Probability in obese/diabetic patients: 40%, compared to 10% in non-comorbid populations (RR = 4.0).
4. Cardiovascular Complications:
- Probability in hypertensive patients on bevacizumab: 45%, compared to 20% in the general population (RR = 2.25).
5. Thromboembolic Events:
- Probability in obese patients undergoing targeted therapy: 35%, compared to 10% in non-comorbid populations (RR = 3.5).
| Adverse Event Type | Frequency in Patients with Comorbidities (%) | Frequency in General Cervical Cancer Population (%) | Compounding Factor (Relative Risk) |
| Infections | 75% | 40% | 1.88x |
| Peripheral Neuropathy | 50% | 30% | 1.67x |
| Delayed Wound Healing | 40% | 10% | 4.0x |
| Cardiovascular Complications | 45% | 20% | 2.25x |
| Thromboembolic Events | 35% | 10% | 3.5x |
Table 3: Compounded Adverse Events in Cervical Cancer Patients with Comorbidities.
These tables and probabilities provide a detailed perspective on the risks associated with compounded adverse events.
Comparison to General Cervical Cancer Population
Patients with comorbidities like HIV, diabetes, obesity, and hypertension face more challenges than the general cervical cancer population. These conditions increase inflammation, weaken the immune system, and affect how treatments work, often leading to more side effects and lower tolerance for therapies. While standard treatments may lead to better survival and response rates in the general population, those with unmanaged comorbidities tend to have worse outcomes. This highlights the need for personalized care and targeted interventions to help close the gap in outcomes.
Patients with comorbidities like HIV, diabetes, obesity, and hypertension face more challenges than the general cervical cancer population. These conditions increase inflammation, weaken the immune system, and affect how treatments work, often leading to more side effects and lower tolerance for therapies. While standard treatments may lead to better survival and response rates in the general population, those with unmanaged comorbidities tend to have worse outcomes. This highlights the need for personalized care and targeted interventions to help close the gap in outcomes.
Biomarkers, Tools, and Standard of Care (SOC)
Biomarkers
Biomarkers play a key role in cervical cancer by helping with diagnosis, predicting outcomes, and monitoring treatment response. Common biomarkers include SCC antigen (SCC-Ag), which can indicate disease progression, and HPV DNA, used to detect high-risk HPV infections. Inflammatory markers like CRP and IL-6 are often elevated in patients with comorbidities like obesity or diabetes, signaling higher levels of systemic inflammation. Newer biomarkers, such as PD-L1, are being used to identify patients who might benefit from immunotherapy, while measures like HbA1c provide insights into how diabetes might be affecting treatment outcomes [22].
Biomarkers
Biomarkers play a key role in cervical cancer by helping with diagnosis, predicting outcomes, and monitoring treatment response. Common biomarkers include SCC antigen (SCC-Ag), which can indicate disease progression, and HPV DNA, used to detect high-risk HPV infections. Inflammatory markers like CRP and IL-6 are often elevated in patients with comorbidities like obesity or diabetes, signaling higher levels of systemic inflammation. Newer biomarkers, such as PD-L1, are being used to identify patients who might benefit from immunotherapy, while measures like HbA1c provide insights into how diabetes might be affecting treatment outcomes [22].
Tools
Cervical cancer care relies on several tools for detection and management. HPV testing and Pap smears are essential for early diagnosis, while imaging techniques like MRI, CT, and PET scans help determine the extent of the disease and check for metastasis. Managing comorbidities involves tools like glucose monitors for diabetes, viral load testing for HIV, and blood pressure monitors for hypertension. To understand how treatment affects patients, healthcare teams use quality of life tools like FACT-Cx and EQ-5D, which capture patient-reported outcomes [23].
Cervical cancer care relies on several tools for detection and management. HPV testing and Pap smears are essential for early diagnosis, while imaging techniques like MRI, CT, and PET scans help determine the extent of the disease and check for metastasis. Managing comorbidities involves tools like glucose monitors for diabetes, viral load testing for HIV, and blood pressure monitors for hypertension. To understand how treatment affects patients, healthcare teams use quality of life tools like FACT-Cx and EQ-5D, which capture patient-reported outcomes [23].
Standard of Care (SOC)
The standard approach to treating cervical cancer usually combines surgery, radiation therapy, and chemotherapy, with cisplatin-based chemotherapy being the most widely used. For advanced cases, immunotherapy like pembrolizumab is often added to improve outcomes. Managing comorbidities is also a critical part of care: ART for HIV, tight blood sugar control for diabetes, lifestyle changes for obesity, and medications for hypertension all play important roles in improving survival and quality of life. A comprehensive care model that addresses both cancer and comorbid conditions is essential for the best results [20].
The standard approach to treating cervical cancer usually combines surgery, radiation therapy, and chemotherapy, with cisplatin-based chemotherapy being the most widely used. For advanced cases, immunotherapy like pembrolizumab is often added to improve outcomes. Managing comorbidities is also a critical part of care: ART for HIV, tight blood sugar control for diabetes, lifestyle changes for obesity, and medications for hypertension all play important roles in improving survival and quality of life. A comprehensive care model that addresses both cancer and comorbid conditions is essential for the best results [20].
Incidence and Prevalence of Inflammatory Disease Subgroups with Comorbidities
Inflammatory diseases, such as obesity, diabetes, and HIV, are common comorbidities in cervical cancer patients and significantly impact both incidence and outcomes. For example, HIV-positive women have a higher prevalence of cervical cancer due to immunosuppression and persistent high-risk HPV infections. Similarly, obesity and diabetes contribute to systemic inflammation, which can accelerate tumor progression and reduce treatment effectiveness. These comorbidities not only increase the overall burden of cervical cancer but also complicate its management, underscoring the need for tailored approaches to care in these subgroups [24].
Inflammatory diseases, such as obesity, diabetes, and HIV, are common comorbidities in cervical cancer patients and significantly impact both incidence and outcomes. For example, HIV-positive women have a higher prevalence of cervical cancer due to immunosuppression and persistent high-risk HPV infections. Similarly, obesity and diabetes contribute to systemic inflammation, which can accelerate tumor progression and reduce treatment effectiveness. These comorbidities not only increase the overall burden of cervical cancer but also complicate its management, underscoring the need for tailored approaches to care in these subgroups [24].
Treatment Regimens, Doses, and Outcomes in Managing Population-Based Mortality
Treatment for cervical cancer typically includes a combination of cisplatin-based chemotherapy, radiation therapy, and, for advanced cases, immunotherapy like pembrolizumab. When managing patients with comorbidities such as HIV, diabetes, obesity, or hypertension, it’s crucial to adjust treatment plans to improve outcomes and reduce mortality. For example, chemotherapy doses may need to be tailored based on kidney function or body weight to avoid severe side effects. Addressing comorbidities alongside cancer treatment can significantly improve survival rates and lower the risk of complications, helping to close gaps in outcomes for high-risk populations [20].
Treatment for cervical cancer typically includes a combination of cisplatin-based chemotherapy, radiation therapy, and, for advanced cases, immunotherapy like pembrolizumab. When managing patients with comorbidities such as HIV, diabetes, obesity, or hypertension, it’s crucial to adjust treatment plans to improve outcomes and reduce mortality. For example, chemotherapy doses may need to be tailored based on kidney function or body weight to avoid severe side effects. Addressing comorbidities alongside cancer treatment can significantly improve survival rates and lower the risk of complications, helping to close gaps in outcomes for high-risk populations [20].
Integration of NCCN Guidelines and SOCs
Integrating NCCN guidelines with standard care for cervical cancer helps ensure patients receive comprehensive, evidence-based treatment tailored to their specific needs. These guidelines highlight the importance of combining therapies like surgery, radiation, and chemotherapy with effective management of comorbidities such as HIV, diabetes, and hypertension. For example, HIV-positive patients benefit from antiretroviral therapy (ART), while tight blood sugar control is crucial for diabetic patients. Aligning standard care with NCCN recommendations helps healthcare teams provide consistent, effective treatment, ultimately improving survival rates and quality of life for patients with cervical cancer and additional health challenges [4].
Integrating NCCN guidelines with standard care for cervical cancer helps ensure patients receive comprehensive, evidence-based treatment tailored to their specific needs. These guidelines highlight the importance of combining therapies like surgery, radiation, and chemotherapy with effective management of comorbidities such as HIV, diabetes, and hypertension. For example, HIV-positive patients benefit from antiretroviral therapy (ART), while tight blood sugar control is crucial for diabetic patients. Aligning standard care with NCCN recommendations helps healthcare teams provide consistent, effective treatment, ultimately improving survival rates and quality of life for patients with cervical cancer and additional health challenges [4].
| Treatment Modality | Description | Typical Adverse Events (AEs) |
| Surgery | Hysterectomy or radical trachelectomy (depending on the stage and fertility goals). | Pain, infection, blood loss, lymphocele, urinary issues. |
| Chemotherapy (Cisplatin-based) | Cisplatin, carboplatin, or a combination with paclitaxel. | Nausea (60%), vomiting (40%), neuropathy (30%), nephrotoxicity (10%), myelosuppression (50%). |
| Radiation Therapy | External beam radiation therapy (EBRT) with or without brachytherapy. | Fatigue (70%), diarrhea (50%), vaginal scarring (25%), skin irritation (30%). |
| Immunotherapy | Pembrolizumab for PD-L1 positive advanced cervical cancer. | Immune-related AEs: colitis (5%), pneumonitis (3%), thyroiditis (7%). |
| Targeted Therapy | Bevacizumab in combination with chemotherapy for recurrent or metastatic cases. | Hypertension (20%), thromboembolic events (15%), bleeding (5%). |
Table 4: NCCN Guideline-Recommended Treatments for Cervical Cancer.
Case Reports: Adult and Pediatric Populations
Case Report 1: Adult Population
Patient: A 45-year-old woman with cervical cancer and HIV.
Case Report 1: Adult Population
Patient: A 45-year-old woman with cervical cancer and HIV.
Presentation: Diagnosed with Stage IIB cervical cancer after presenting with pelvic pain and abnormal bleeding. She had a 10-year history of HIV, well-controlled on antiretroviral therapy (ART), with a viral load <200 copies/mL.
Treatment: The patient received cisplatin-based chemoradiation while continuing ART. Dose adjustments were made to prevent nephrotoxicity, and prophylactic antibiotics were used to minimize infection risks.
Outcome: The patient tolerated treatment well, with no severe adverse events. Post-treatment imaging showed no residual tumor, and her viral load remained undetectable. The patient’s overall survival (OS) at two years remains excellent [25].
Case Report 2: Pediatric Population
Patient: A 16-year-old girl with recurrent cervical cancer and poorly controlled Type 1 diabetes.
Patient: A 16-year-old girl with recurrent cervical cancer and poorly controlled Type 1 diabetes.
Presentation: Presented with fatigue, weight loss, and persistent vaginal bleeding. She was found to have a recurrent cervical tumor despite previous treatment with surgery and chemotherapy. Her HbA1c was 10.2%, reflecting poor glycemic control.
Treatment: A second-line treatment regimen of carboplatin and paclitaxel was initiated, alongside a multidisciplinary approach to improve her diabetes management with insulin adjustments and dietary counseling.
Outcome: Glycemic control improved significantly during therapy (HbA1c reduced to 7.8%), and her treatment response was partial remission. However, she experienced peripheral neuropathy, managed with dose reductions and supportive care [26].
Case Report 3: Adult Population
Patient: A 52-year-old woman with cervical cancer, obesity (BMI 35), and hypertension.
Patient: A 52-year-old woman with cervical cancer, obesity (BMI 35), and hypertension.
Presentation: Diagnosed with Stage IIIB cervical cancer after reporting severe pelvic pain and heavy vaginal bleeding. Comorbidities included poorly controlled hypertension and obesity.
Treatment: Treated with concurrent chemoradiation using cisplatin. The hypertension was managed with ACE inhibitors, and a supervised weight management program was introduced during treatment.
Outcome: Despite initial challenges with blood pressure control, her hypertension stabilized, and she completed therapy without major interruptions. Post-treatment imaging showed significant tumor shrinkage. [20]
Case Report 4: Pediatric Population
Patient: A 14-year-old girl with cervical adenocarcinoma and underlying systemic lupus erythematosus (SLE).
Patient: A 14-year-old girl with cervical adenocarcinoma and underlying systemic lupus erythematosus (SLE).
Presentation: Presented with persistent pelvic pain and abnormal discharge. Her SLE was stable on low-dose corticosteroids and hydroxychloroquine.
Treatment: Managed with a combination of surgery and radiation therapy. Immunotherapy was considered but deferred due to concerns about exacerbating her autoimmune condition. Close monitoring for SLE flare-ups was performed during treatment.
Outcome: The patient experienced mild radiation cystitis, managed with supportive care. Her SLE remained stable throughout therapy, and follow-up scans showed no evidence of disease at one year [27].
Disclaimer
This paper was financially supported by Nexus Alliance Biopharma (www.NexusAllianceBiopharma.com). Nexus Alliance provided logistical support and grant funding for the development of this paper; however, the authors were not directly compensated by Nexus Alliance for their contributions. The content, analysis, and conclusions presented are solely those of the authors and do not necessarily reflect the views or positions of Nexus Alliance Biopharma. Compliance Statement Nexus Alliance Biopharma operates in full compliance with U.S. federal laws and regulations, including those enforced by the Department of Justice (DOJ), the Department of the Treasury’s Office of Foreign Assets Control (OFAC), and other relevant regulatory bodies. Nexus Alliance affirms that: 1. None of its principles reside in Russia, China, Hong Kong, or any sanctioned nation, including Cuba, Iran, North Korea, Sudan, or Syria. 2. It does not and will not engage with the governments of Russia, China, Hong Kong, or any sanctioned nations. 3. It strictly adheres to U.S. laws and guidelines, including the Export Administration Regulations (EAR), International Traffic in Arms Regulations (ITAR), the Foreign Corrupt Practices Act (FCPA), and all applicable sanctions and trade restrictions. This disclaimer reflects the organization’s commitment to ethical practices, compliance, and transparence.
References
- World Health Organization (WHO). Cervical Cancer Factsheet. Published 2020. Accessed from: https://www.who.int/
- Liu G, Kong L, Zhang J. (2020). Impact of comorbidities on cancer prognosis: A meta-analysis. Asian Pac J Cancer Prev. 21(2): 433-442.
- Chumduri C, Gurumurthy RK, Meyer TF. (2016). Regulation of host cell survival during bacterial infection: A focus on the interplay between apoptosis and autophagy. Cell Death Differ. 23(5): 761-770.
- Koh WJ, Abu-Rustum NR, Bean S, et al. (2022). Cervical cancer, version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 20(1): 96-121.
- American Cancer Society. Managing Comorbidities in Cancer Care. Published 2021. Accessed from: https://www.cancer.org/
- Kulasingam SL, Havrilesky L, Ghebre R, Myers ER. (2011). Screening for cervical cancer: A decision analysis for the US Preventive Services Task Force. J Clin Epidemiol. 64(12): 1478-1485.
- Bray F, Ferlay J, Soerjomataram I, et al. (2018). Global cancer statistics: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 68(6): 394-424.
- Denny L, de Sanjose S, Mutebi M. (2017). Cervical cancer: Prevention and treatment. Am Soc Clin Oncol Educ Book. 37: 449-457.
- Bray F, Jemal A, Grey N, Ferlay J, Forman D. (2012). Global cancer transitions according to the Human Development Index (2008–2030): A population-based study. Lancet Oncol. 13(8): 790-801.
- Garon EB, Rizvi NA, Hui R, et al. (2015). Pembrolizumab for the treatment of non–small-cell lung cancer. N Engl J Med. 372(21): 2018-2028.
- Han H, Guo W, Shi W, et al. (2017). Hypertension and breast cancer survival: A meta-analysis. Sci Rep. 7(1): 44877.
- World Health Organization (WHO). Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. Published 2016. Accessed from: https://www.who.int
- American Diabetes Association (ADA). (2022). Standards of Medical Care in Diabetes. Diabetes Care. 45(Suppl 1): S1-S264.
- National Heart, Lung, and Blood Institute (NHLBI). Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel. Published 2013. Accessed from: https://www.nhlbi.nih.gov
- Whelton PK, Carey RM, Aronow WS, et al. (2017). ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 71(19): e127-e248.
- Hernandez BY, Wilkens LR, Zhu X, Thompson PJ. (2019). Comorbidities and survival disparities among patients with invasive cervical cancer. Cancer.125(7): 1129-1137.
- Beavis AL, Gravitt PE, Rositch AF. (2017). HIV infection and cervical cancer: A systematic review of the epidemiology and mechanisms. Cancer Epidemiol Biomarkers Prev. 26(9): 1270-1274.
- Denny L, Anorlu R, Sankaranarayanan R. (2012). Cervical cancer: The impact of control strategies in low- and middle-income countries. Int J Gynaecol Obstet. 119(Suppl 1): S60-S66.
- Basen-Engquist K, Bodurka-Bevers D, Fitzgerald MA, et al. (2001). Reliability and validity of the Functional Assessment of Cancer Therapy–Cervix (FACT-Cx) in measuring health-related quality of life in patients with cervical cancer. Gynecol Oncol. 81(2): 179-184.
- Tewari KS, Sill MW, Long HJ, et al.? (2014). Improved survival with bevacizumab in advanced cervical cancer. N Engl J Med. 370(8): 734-743.
- Long HJ, Bundy BN, Grendys EC, et al. (2005). Randomized phase III trial of cisplatin with or without topotecan in carcinoma of the uterine cervix: A Gynecologic Oncology Group Study. J Clin Oncol. 23(21): 4626-4633.
- Escudero-Esparza A, Kalchishkova N, Mitchell H, Johnson P. (2021). Biomarkers in cervical cancer: From diagnosis to therapeutic targets. Front Oncol. 11: 647512.
- Saslow D, Solomon D, Lawson HW, et al. (2012). American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 62(3): 147-172.
- De Vuyst H, Clifford GM, Nascimento MC, Madeleine MM, Franceschi S. (2009). Infection with human immunodeficiency virus and human papillomavirus: A meta-analysis of the risk of cervical cancer. Cancer Epidemiol Biomarkers Prev. 18(4): 1066-1083.
- Chiang CL, Border S, Jenkins C. (2018). The impact of HIV on treatment outcomes in patients with cervical cancer. J Glob Oncol. 4: 1-7.
- Duarte-Franco E, Franco EL, Ferenczy A. (2001). Prospects for controlling cervical cancer at the turn of the century. Curr Oncol Rep. 3(1): 41-46.
- Berg SL, Blaney SM, Adamson PC. (2013). Childhood cancer in the context of chronic conditions: Challenges and opportunities. J Clin Oncol. 31(5): 585-590.
Citation: Timothy Allen, Nepton Sheikh-khoni, Ariella Allen, Yasmin Allen and Nasrin Momeni. (2025). A Comprehensive Diagnostic and Treatment Framework for Cervical Cancer Patients with Comorbidities. Journal of Biotechnology and Immunology 7(1).
Copyright: © 2025 Timothy Allen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.