Research Article
Volume 2 Issue 1 - 2020
Usefulness of Dexmedetomidine in Drug-Induced Sleep Endoscopy
1Departament of Otolaryngology. Hospital General de Occidente, SSJ, Zapopan, Jalisco, México.
2Departament of Otolaryngology. Hospital Constitución, ISSSTE, Monterrey, Nuevo León, México.
2Departament of Otolaryngology. Hospital Constitución, ISSSTE, Monterrey, Nuevo León, México.
*Corresponding Author: Flores-Ochoa JR, Departament of Otolaryngology. Hospital General de Occidente, SSJ, Zapopan, Jalisco, México.
Received: July 01, 2020; Published: July 10, 2020
Abstract
Background: Obstructive sleep apnea (OSA) should be considered a public health problem, since it affects 9-28% of women and 24-26% of men in the general population. The first line of treatment is still Positive Airway Pressure (PAP). However, given the need to offer specific treatment and alternatives besides PAP it is important to assess the airway in a dynamic way as well as in a safe environment that is similar to physiological sleep. This is why Drug-Induced Sleep Endoscopy (DISE) has become an essential tool in some of the cases.
Objective: To assess the Bispectral Index (BIS) as well as heart rate, blood pressure, oxygen saturation, patient satisfaction and to register possible incidents during the administration of dexmedetomidine in DISE by placing the patient in three different positions (supine, right lateral recumbent, left lateral recumbent) long enough to obtain diagnostic information.
Materials and Methods: 40 patients with OSA were included. These patients had maladaptation criteria or poor adherence to treatment with PAP, or were pre-surgical patients. These patients underwent DISE with dexmedetomidine. Vital signs and bispectral index (BIS) were monitored at all times during the procedure.
Results: The initial BIS was 81.4±3.5. During the procedure the BIS value was 61.4 ± 4.7 and the final measurements were 97.6±5.7. The use of topical intranasal medications or drugs to reduce nasal secretions was not necessary. It was possible to identify obstructive events in all the performed procedures, which had a recovery time average of 9.85±2.8 minutes. These events lasted for 36.07 ±1.5 on average with a 92.5% satisfaction.
Conclusion: The use of dexmedetomidine for DISE allows to mimic sleep, which allows the observation of apneic events in patients with OSA. At the same time, the BIS verification provides the security of slight sedation with a minimum possibility for complications and a high satisfaction rate. The possibility to perform these studies for enough time and without the need to use drugs to reduce nasal secretions, allows the physician to perform maneuvers with mandibular advancement devices (MAD) and positive airway pressure (PAP) equipment.
Background
Among the sleep-related breathing disorders, obstructive apnea syndrome is a subgroup with the highest prevalence of harmful effects due to cardiovascular risk. [1]It is estimated that in the last years this syndrome has come to affect 9-28% of women and 24-26% of men in the general population, [2] keeping a strong association with different comorbidities such as obesity, hypertension, diabetes mellitus, and insomnia turning it into a public health problem. [3,4]
Thanks to the technological improvements and the interest of a number of health areas on this condition diagnosis and integral management of the patient with OSA are more accessible than ever. A variety of therapeutic measures can be offered, such as hygienic-dietetic measures and promotion of exercise, MAD, PAP, airway surgery, and surgeries to reduce body mass index. Nowadays, the first-line treatment is PAP. However, not all patients manage to adapt to the equipment, which is why it is necessary to offer alternatives. [5] This is the reason why the technical directed assessment is essential to identify upper airway anatomy during the mimicry of sleep as well as to measure the therapeutic intraoral equipment and identify maladaptation causes to the pressure equipment. [6,7]
Drug-induced sleep endoscopy is better than the airway assessment in awake patient, including simulation maneuvers and non-dynamic imaging techniques. This technique was first defined by Croft and Pringle in 1991 and it is indicated pre-surgically, to measure the mandibular advancement, finding causes of maladaptation to PAP, and of failure of previous surgical treatments. [8]
Traditionally, midazolam was used as the sleep inductor during endoscopy, and according to some authors, snoring was accomplished in approximately 90-95% of the patients with OSA. Other investigators used propofol instead, a sedative-hypnotic drug with a short half-life, which caused less respiratory depression compared to benzodiazepines and less adverse effects like nausea and headaches. [9]
The term "conscious sedation" refers to a slightly depressed level of consciousness that allows the patient to keep a permeable airway and respond appropriately to physical stimulation and verbal interactions. “Deep sedation” refers to an unconscious status accompanied by a partial loss of the airway protective reflexes, included the ability to follow verbal instructions. [10]
In this study, the authors administered dexmedetomidine (a stereoisomer derived from medetomidine, which stimulates α-2 adrenergic receptors) as a sedative-hypnotic drug to perform endoscopy under medication’s effects to mimic sleep with the intention of trying a different alternative, as proposed by Lugo,et al. [11]
Scheinin and his team found that the average time dexmedetomidine stays in plasma is 1.6-1.7 hours, it has an elimination half-life of 1.6-2.6 hours, total plasma clearance of 0.7-0.9 l/hr/kg and apparent volume of distribution of 2.1-2.6 l/kg. It binds to plasmatic proteins in 94% and 95% of its metabolism occurs in the liver (by hydroxylation and N-methylation) and in the kidney. It provides its antinociceptive effect by acting on α-2 adrenergic receptors in the spinal cord and the sedative-hypnotic effect occurs by decreasing the release of acetylcholine when it binds to this same receptors in the locus coeruleus, which is associated with the transition from the vigil to sleep. [12, 13]
Our objective was to assess the administration of dexmedetomidine as a sleep inductor drug and to corroborate the sedation degree during the procedure using BIS while the patient is being positioned in different planes.
Materials and Methods
This is an observational and descriptive study. All patients previously signed a written informed consent form. 40 patients older than 18 years with the diagnosis of obstructive sleep apnoea were included (Apnea Link plus, ResMed, Germany). The patients were non-invasively monitored in the recovery room (type 1 monitoring) to obtain basal hemodynamic parameters and peripheral vascular access. Bispectral monitoring was added in the operating room, which was previously conditioned with soft light, in silence, and warm temperature (BIS, Covidien, Ireland). The bispectral monitoring generates an indicator that comes from an electroencephalographic signal with power analysis and a temporary domain that optimizes the correlations of the anesthesia’s clinical effects through algorithms to obtain the bispectral index. [14]
When BIS values are between 65-75, memory function is decreased significantly as well as the probability of explicit memory. BIS values between 50-60 indicate a greater anesthetic effect and deep sedation level. These values indicate a reduced cerebral metabolic rate that is caused by most of the hypnotic drugs, however, other changes in cerebral metabolism can be produced due to factors different to the drug administration, for example, temperature. [15, 16]
The influence of BIS-controlled anesthesia presents as its principal goals to reduce the amount of drug administered, to minimize the duration of the recovery period, to decrease the number of intraoperative awakenings, and to increase the patients’ satisfaction level. [14, 15]
The sedation degree is crucial in recreating the events without causing respiratory depression. dexmedetomidine gathers the ideal characteristics for this purpose, such as the absence of respiratory depression without having to modify the airway, provides sedation and analgesia, neurovegetative protection, and the fact that an antagonist drug (atipamezole) is available to revert its undesirable effects or to block its action. [12]
The procedure started with an impregnation dose of 1mg/kg of dexmedetomidine to be infused in 20 minutes and continued with the maintenance dose of 0.5 mg/kg/h. In the operating room the patient was held in supine, right lateral recumbent and left lateral recumbent positions, and if necessary, measurements of intraoral devices or concomitant PAP were performed while the episodes were monitored with the flexible endoscope at all times (Olympus, United States). The authors tried to reach at least a 10 minute period with the patient in each position and not to use topical nasal anesthesia or any other drugs to reduce the production of mucus. Dexmedetomidine’s infusion was maintained during the whole procedure and was suspended at the end of it. We quantified the total duration of the procedure.
Patients were transferred to the recovery room and Ramsay’s sedation scale was measured. The patient was asked for pain during the procedure using the analog visual scale of pain and whether or not there was amnesia of the procedure. Furthermore, the length of stay in the recovery room was also registered.
Results
40 patients with a confirmed diagnosis of obstructive sleep apnea syndrome were included. (Table 1) The average patient age was 54 ± 20.7 (45-66 years) 65% of the patients were men (26/40). The SPSS software was used by the authors for the statistical analysis. The positioning of the patient in the three different planes (supine, right lateral recumbent, left lateral recumbent) was possible in all the cases, which allowed the authors to verify the patient’s anatomy and its dynamism, as well as to measure intraoral devices and airway pressure equipment in some cases. (Figure 1)
| Obstructive sleep apnea syndrome | Mild | Moderate | Severe |
| Men | 7 | 9 | 10 |
| Women | 7 | 5 | 2 |
| Body Mass Index | 30±3.4 | 29±4.7 | 34.5±4.8 |
| Age | 50.3±6.5 | 56.2±2.9 | 53.6±5.4 |
Table 1: Included patients in this study arranged by gender and stratification of the disease.
Vital signs (heart rate, arterial pressure, oxygen saturation, and BIS) were registered in three different moments: before, during, and after the procedure and were evaluated with measures of central tendency. (Tabla 2).
| Variable | Initial | Trans | Final |
| Heart rate (bpm) | 54-92 | 51-82 | 53-81 |
| 71.4±2.4 | 65.7±2.3 | 68.5±2.4 | |
| Mean arterial pressure (mmHg) | 67-90 | 65-86 | 65-86 |
| 76.8±3.6 | 72.7±6.8 | 78.7±6.7 | |
| Oxygen saturation (%) | 95-98 | 70-94 | 93-97 |
| 93±94 | 82.1±7.36 | 95.3±0.80 | |
| Bispectral index (%) | 65-85 | 59-71 | 96-98 |
| 81.4±3.5 | 61.4±4.7 | 97.6±5.7 |
Table 2: Vital signs before, during, and after the procedure.
Recovery time was quantified in minutes, starting the moment the dexmedetomidine infusion was suspended and ending at the moment of the patient’s discharge from the recovery room. The mean time was 9.85±2.8 minutes, with a minimum of 7 and a maximum of 13 minutes.
Prior to discharge, the existence of amnesia was evaluated through interrogatory; only three patients (7.5%) referred to recall the procedure.
The mean duration of the nasendoscopy studies was 36.07±1.5 minutes (minimum 30 and maximum of 40 minutes), topical nasal anesthetics were not necessary and neither were drugs to reduce nasal discharge. It was possible to position the patient in the three different planes in all cases.
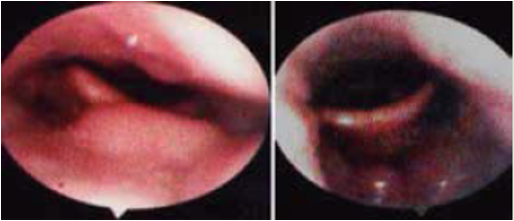
Figure 1: Nasendoscopy with the patient in a supine position, it is possible to observe the important involvement of the soft palate that causes anteroposterior obstruction (A). In the same patient, lying in left lateral recumbent position. It is visible the notorious improvement in regards to the soft palate; however, the involvement of the lingual tonsils is appreciated (B).
The correlation between the bispectral index, recovery time, and patient satisfaction was done by χ2 analysis and Pearson; values < 0.05 were considered statistically significant, with a confidence interval of 95%. (Table 3)
| Bispectral Index | ||||||
| Initial | During the procedure | Final | Recovery time | Patient’s Satisfaction | ||
| BIS I | Pearson’s correlation | 1 | .416 | .421 | .474 | -.262 |
| P. (bilateral) N | 40 | .073 40 |
0.63 40 |
.050 40 |
.251 40 |
|
| BIS T | Pearson’s correlation | .417 | 1 | .415 | .171 | .106 |
| P. (bilateral) N | .066 40 |
40 | .064 40 |
.463 40 |
.656 40 |
|
| BIS F | Pearson’s correlation | .419 | .417 | 1 | -.062 | .472 |
| P. (bilateral) N | .069 40 |
.062 40 |
40 | .789 40 |
.032 40 |
|
| Recovery time | Pearson’s correlation | .441 | .172 | -.067 | 1 | .087 |
| P. (bilateral) N | .046 40 |
.462 40 |
.794 40 |
40 | .726 40 |
|
| Patient’s satisfaction | Pearson’s correlation | -.262 | .104 | .478 | -.086 | 1 |
| P. (bilateral) N | .253 40 |
.656 40 |
.032 40 |
.727 40 |
40 | |
BIS: Bispectral index; I: Initial; T: during the procedure; F: at the end of the procedure.
Table 3: Variables correlation.
Table 3: Variables correlation.
Discussion
OSA is the result of one or more sites of obstruction or collapse in some fenotypes. There is an imbalance in some point between the dilatator and constrictor forces and the muscle groups that participate or stop participating until blockage or obstruction is generated.
The goals of conscious sedation are to provide analgesia, anxiolysis, sedation and hypnosis, and at the same time to maintain the cardiorespiratory stability and to keep the recovery time short with minimun incidence of collateral effects. Bispectral index is helpful to monitor the adequate sedation level while respecting this purposes.
Dexmedetomidine can be used in different medical areas thanks to its high efficacy, safety and conscious sedation index, allowing the patient to be calm and cooperative, breathing spontaneously with low risk of bronchoaspiration given that there are barely any nasal secretions. Even at high doses, the airway does not suffer any modifications that could be held responsible for the obstruction of airflow in the majority of the procedures, specifically in sedated endoscopy, which provides enough time to perform the necessary studies, device measurements and positions.
In the patients of this study it was possible to identify snoring and apnea episodes with hemodynamic stability in 100% of the cases. The variations that occurred were not statistically significant: three patients (7.5%) present bradycardia without other alterations, which ceased when the infusion rate was decreased in 40%, thus there was no need to administer atropine. Overall, patient’s comfort and satisfaction was 95%.
The current use of DISE not only provides anatomical information but also helps the measurement of intraoral devices (MAD, in the author’s experience) looking for candidate patients and searching the cause of poor adherence or suboptimal results with the use of PAP (figure 2 and 3).
Figure 2: During DISE it is possible to move the patient and find which patients are candidates for MAD.

Figure 3: During DISE it is possible to locate causes of lack of adaptation to the pressure devices.
Conclusions
In general, positive airway pressure is the first choice of treatment for obstructive sleep apnea. However, there are other alternatives for patients that do not accomplish optimal parameters, do not wish to use positive pressure equipment or have other specific needs. At first, the main target of drug-induced sleep endoscopy was to find the anatomical characteristics that would allow the physician to use the least amount of events and surgical areas with the highest result rate, especially when visualizing the hypopharyngeal area.
In this study, dexmedetomidine was used and patients were monitored with type 1 monitoring and BIS with the aim of corroborating the sedation degree that permitted the appreciation of apneic episodes as well as to move the patient during the procedure. The usefulness and safety of this drug were confirmed.
Further studies with dexmedetomidine are required to confirm whether or not there are changes in sleep architecture, as demonstrated with propofol and midazolam. It is known that this diagnostic procedure is not completely physiological but it’s understood that it represents the best option thanks to the dynamism and sedation degree that it offers. Our results show that the administration of dexmedetomidine in DISE is a safe and reproducible option that eliminates the need for local anesthesia and drugs to reduce secretions, making it possible to perform the study for as long as required.
References
- Montserrat J, Puertas F. Patología Básica del Sueño. Elsevier. (2015). Capitulo 6; Síndrome de apneas durante el sueño: 83-112.
- Jehan S, Auguste E, Zizi F, Pandi-Perumal S, Gupta R. (2016). Obstructive Sleep Apnea: Women´s Perspective. Journal Sleep Medicine Disord. 3(6).
- Foster G, Sanders M, Millman R, Zammit G, et al. (2009). Obstructive Sleep Apnea among obese patientes with type 2 diabetes. Diabetes Care 32: 1017-1019.
- Marin J, Agusti A, Villar I, Forener M, Nieto D, et al. (2012). Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 307: 1378-1384.
- Plaza G, Baptista P, O´Connor C. Sleep Disordered Breathing. Amplifon. (2017). Chapter 25; Treatment Algorithm for Obstructive Sleep Apnea-Hypopnea Syndrome 527-545.
- Hohenhorts W, Ravesloot M, Kezirian E, de Vries N. (2012). Drug-induced sleep endoscopy in adults with sleep disordered breathing: Technique and the VOTE calssification system. Operative Thechniques in Otolaringology 23: 11-18.
- Carrasco M, Martínez L, Vaz de Castro J, Matarredona-Quiles s, Dalmau-Galofre J. (2019). Drud-induced Sleep Endoscopy a Tool for Surgical Planning. Current Otorhinolaryngology. Springer Nature.
- Esteller E, Vila J, Vilaseco I, Diaz M, Carrasco M, et al. (2018). Guía de Práctica Clínica sobre Exploración Física de la Vía Aérea Superior en el SAHOS del Adulto. Sociedad Española de Sueño.
- Kotecha B, De Vito A. (2018). Drug indiced sleep endosocpy: its role in evaluation of upper airway obstruction and patient selection for surgical and non-sugical treatment. Journal of Thoracic Diseas. 10(Suppl 1): S40-S47.
- Hernandez L, (2004). Sedación consciente e inconsciente. Revista Mexicana de Anestesiologia. 27: 95-97.
- Lugo R, Puon A, Guzman K, et al. (2012). Dexmedetomidina en la fibroscopia de sueño bajo sedación en pacientes con trastornos respiratorios del dormir. Acta de Otorrinolaringología y Cirugía de Cabeza y Cuello 40: 279-285.
- Scheinin H, Karhrvaara S, Olkkola KT, et al. (1992). Pharmacodynamics and pharmacokinetics of intramuscular dexmedetomidine. Clin Pharmacol Ther. 52:537-546.
- Sánchez E, Chávez O, Hernández D. (2006). Dexmedetomidina en anestesia pediátrica. Anestesia en México. 18: 112-119.
- Punjasawadwong Y, Boojeungmonkol N, Phongchiewboon A. (2007). Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database System Rev. 4: 38-43.
- Tardio R, Sejas J, Castellon V, Bustamante C, Orozco A. (2010). Utilidad del índice biespectral en la monitorización de la conciencia durante la anestesia general. Rev Científica Ciencia Médica. 12: 69-7.
Citation: Flores-Ochoa JR, Lugo Saldaña R. (2020). Usefulness of Dexmedetomidine in Drug-Induced Sleep Endoscopy. Journal of Otolaryngology - Head and Neck Diseases 2(1).
Copyright: © 2020 Flores-Ochoa JR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
