Case Report
Volume 1 Issue 1 - 2019
Unilateral Blepharoptosis in Patient with Graves Orbitopathy: A Case Report
1Medical Director, Otorhinolaryngologist and Facial Surgeon, Topmedical Mexico
2Otolaryngologist and Facial Surgeon, Private Practice Mexico
3Otolaryngologist and Fellowship in Facial Surgery, Topmedical Mexico
2Otolaryngologist and Facial Surgeon, Private Practice Mexico
3Otolaryngologist and Fellowship in Facial Surgery, Topmedical Mexico
*Corresponding Author: Torres-Vasconcelos R, Medical Director, Otorhinolaryngologist and Facial Surgeon, Topmedical Mexico.
Received: April 04, 2019; Published: April 16, 2019
Abstract
Background: Palpebral ptosis is the fall of the upper lid edge greater than 1.5 mm, down the sclero-corneal limbus in its upper zone.
Objective: The purpose of this report is to present a clinical case of a patient who comes to consultation with aesthetic disconformity of the eyelids, with a history of Graves' disease.
Materials and Methods: We present a clinical case of a 49 years old patient who progressively presented right unilateral palpebral ptosis associated with non-active Graves' orbitopathy. Surgical treatment and postoperative results are presented.
Results: The patient underwent an endoscopic orbital decompression of 2 walls and after 6 months, an upper blepharoplasty combined with levator aponeurosis repair was performed, presenting a functional and esthetic improvement.
Introduction
Palpebral ptosis is the fall of the upper lid edge greater than 1.5 mm, down the sclero-corneal limbus in its upper zone and slightly higher in the nasal sector. It is accompanied by isolation of the eyelid and, sometimes, disappearance of its fold, which causes discomfort to the patient due to its aesthetic and functional limitations; it can be present at birth (congenital ptosis) or develops in the course of life (acquired ptosis). It can affect one or both eyes. [1,3]
It has been classified in an indistinct way by different authors, attending to the moment of its appearance, its cause, the function of the levator palpebrae superior muscle, based on the degree of drooping of the eyelid, among other aspects. They are grouped into myogenic, aponeurotic, neurogenic, mechanical and traumatic. [2,4]
Congenital
- Congenital ptosis isolated
- Congenital myasthenic syndromes
- Transient neonatal myasthenia (myasthenic mother)
- Blepharophimosis
- Anomalous synkinesias
Structural
- Dehiscence of the elevator (senile)
- Tumors of orbits or eyelids (pseudoptosis)
- Dermatocalasia
- Lax eyelid syndrome
- Eyelid edema (pseudoptosis)
Sympathetic innervation
- Horner síndrome
Muscle
- Myotonic dystrophies
- Chronic progressive external ophthalmoplegia
- Other mitochondrial diseases
- Oculopharyngeal muscular dystrophy
- Dysthyroid disease (Graves’ disease)
Neuromuscular junction
- Myasthenia gravis
- Lambert Eaton síndrome
- Common ocular motor nerve
Central
- Cortical ptosis
- Hemifacial spasm (pseudoptosis)
- Essential Blepharospasm (pseudoptosis)
- Apraxia of the ocular opening (pseudoptosis)
Congenital palpebral ptosis accounts for approximately 80% of palpebral ptosis. of the remaining 20%, the involutive or senile palpebral ptosis remains the most frequent worldwide. [5-6]
Non-Active Graves' Orbitopathy
The treatment of non-active GO is of the surgical-rehabilitating type.
The treatment of non-active GO is of the surgical-rehabilitating type.
Traditionally a gradual and orderly scheme for the surgical rehabilitation of patients is recommended, doing surgery by stages, according to the needs of the patient, in the following way:
- Orbital decompression (bone and fat).
- Restrictive strabismus.
- Eyelid surgery (retraction).
- Blepharoplasty-periorbital lipectomy.
In the case that will be presented next, is corresponds to a blepharoptosis of muscular origin secondary to Graves' orbitopathy that is rare.
Case Presentation
We present the case of a 49-year-old male entrepreneur with a genetic load for diabetes mellitus type 2.
We present the case of a 49-year-old male entrepreneur with a genetic load for diabetes mellitus type 2.
In 2012 he was diagnosed with hyperthyroidism (noting the onset of exophthalmos) managed medically with thyroid inhibitors, responding poorly. On November 20, 2012, he underwent total thyroidectomy and sustitution therapy, remaining in good general condition, except for constant headaches.
In 2017, in addition to exophthalmos, he begins with a progressive fall of the right upper eyelid, as well as vertical strabismus.
He presented with us on July 24, 2018 a consultation assessment due to aesthetic discomfort due to exophthalmos and "fall" of the upper right eyelid, with muscle fatigue and headache in the frontal region of right predominance as his main discomforts.
A simple tomography study was requested and, based on the findings, it was decided to perform bilateral orbital decompression and he was scheduled to upper eyelid lift surgery 6 months after decompression.
On August 8, 2018, orbital decompression of two walls is performed by combined approach. After this procedure, the patient reported that the headache disappeared and he noticed improvement in the appearance of his eyes.
Due to the good result of the decompression, and having elapsed 6 months, it is agreed with the patient to perform the surgery of reinsertion of the levator muscle tendon of the upper right eyelid, taking place on February 20, 2019.
The follow-up of the patient shows a favorable evolution, recovering symmetry between the free edge of both upper eyelids, decreasing the limitation to the visual field imposed by the right blepharoptosis and improving the quality of life of the patient.
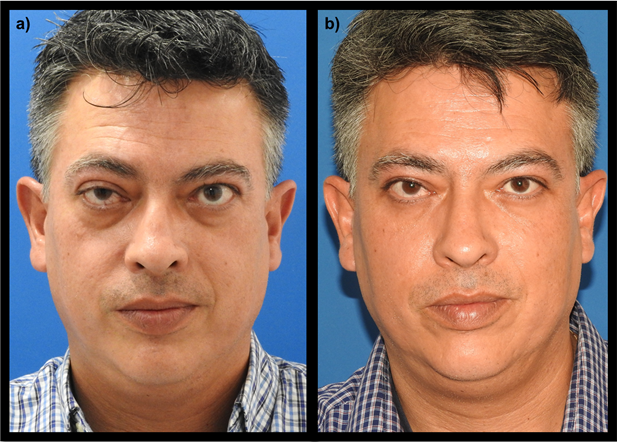
Figure 1: Front view of the patient’s face
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
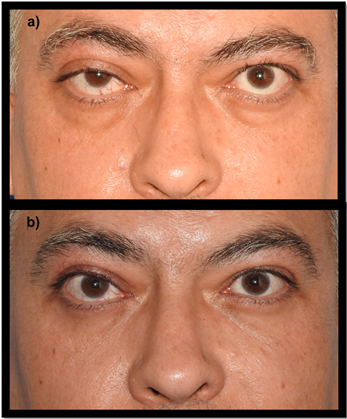
Figure 2: Frontal approach of the periocular region
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
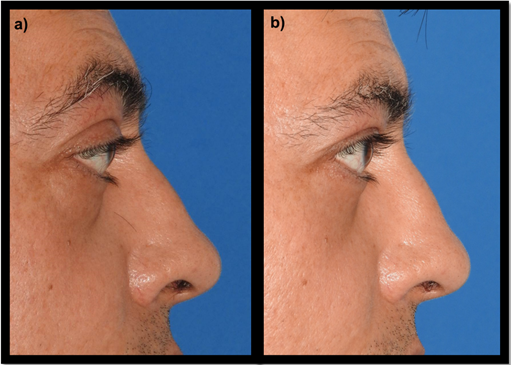
Figure 3: Lateral approach of the right periocular region
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
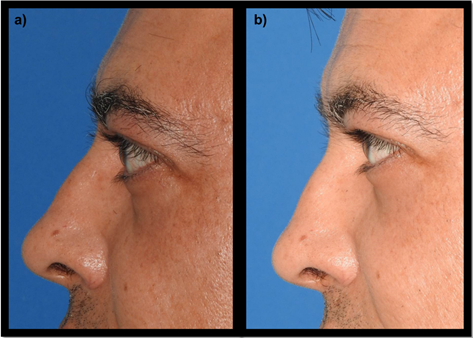
Figure 4: Lateral approach of the left periocular region
a) Prior orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift

Figure 5: Left oblique view of the patient’s face
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift

Figure 6: Right oblique view of the patient’s face
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
a) Prior to orbital decompression and reinsertion of the upper eyelid elevator
b) Postoperative result at 6 weeks after reinsertion of the upper eyelid lift
Discussion
Blepharoptosis associated with Graves' orbitopathy is a rare condition. We consider very important that the management of this condition must be in stages.
It is recommended that eyelid surgery in Graves' Orbitopathy be performed at the beginning or at the end of the treatment of non-active Orbitopathy. At the beginning of the disease, tarsorrhaphy may be necessary to allow corneal protection urgently as a temporary measure while undergoing medical treatment. On the other hand, palpebral surgery at the end of the course of the disease is also performed to improve eyelid retraction for cosmetic and functional purposes as eye protection. [7-9]
In general eye rehabilitation, eyelid surgery should be delayed 1 year after the control of hyperthyroidism and at least 6 months after the eye disease stabilizes. [8]
Conclusion
In the case of our patient he did not present ocular retraction but ptosis of the right upper eyelid, given this situation and assessing that muscle function was preserved, it was decided to first perform orbital decompression of two walls, then wait for the inflammatory period in order to have more predictable results, and at 6 months upper blepharoplasty combined with levator aponeurosis repair was performed. The patient presented improvement in aesthetics and function.
References
- Morris CL, Morris WR, Fleming JC. (2011). A histological analysis of the Müllerectomy: redefining its mechanism in ptosis repair. Plast Reconstr Surg. 127(6): 2333-41.
- Hwang K, Huan F, Kim DJ, Hwang SH. (2010). Size of the superior palpebral involuntary muscle (Müller muscle). J Craniofac Surg 21(5): 1626-9.
- Marcet MM, Meyer DR, Greenwald MJ, Roth S, Selva D. (2013). Proximal Tarsal Attachments of the Levator Aponeurosis: Implications for Blepharoptosis Repair. Ophthalmology [internet]. Sep. [citado 12 feb. 2014];120(9):[aprox. 6 p.]. Disponible en:
- De Sanctis U. Blepharoptosis. Minerva Chir. (2013) Dec.;68(6 Suppl. 1):37-47. Marcus MM. Proximal Tarsal Attachments of the Levator Aponeurosis. Ophthalmology. 2013;120:1924-9.
- Marcus MM. (2013). Proximal Tarsal Attachments of the Levator Aponeurosis. Ophthalmology.120: 1924-9.
- Waqar S, McMurray C, Madge SN. (2010). Transcutaneous blepharoptosis surgery-advancement of levator aponeurosis. Open Ophthalmol J [internet]. Dec. [citado 14 mayo 2014];4:[aprox. 5 p.]. Disponible en: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041000/?report=classic
- Gorman CA, Waller RR, Dyer JA: The eye and orbit in thyroid disease, 1984, Raven Press.
- Burch HB, Wartofsky L. (1993). Graves’ ophthalmopathy: current concepts regarding pathogenesis and management. Endocr Rev 14(6): 747–793.
- Bahn RS. (2003). Clinical review 157: Pathophysiology of Graves’ ophthalmopathy: the cycle of disease. J Clin Endocrinol Metab 88 (5): 1939–1946.
Citation: Torres-Vasconcelos R, Navarro-Anaya G and Bernal-Carreón MA. (2019). Unilateral Blepharoptosis in Patient with Graves Orbitopathy: A Case Report. Journal of Otolaryngology - Head and Neck Diseases 1(1).
Copyright: © 2019 Torres-Vasconcelos R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
