Case Report
Volume 2 Issue 3 - 2020
The Tunneled Epidural Catheter Can Provide Timely Analgesia for Refractory Cancer Pain – A Case Report
MD PhD, Department of pain medicine, Division of Anaesthesiology, Critical Care Pain medicine, The University of Texas MD Anderson Cancer Center, USA
*Corresponding Author: Billy Huh, MD PhD, Department of pain medicine, Division of Anesthesiology, Critical Care Pain medicine, The University of Texas MD Anderson Cancer Center, USA.
Received: April 15, 2020; Published: April 24, 2020
Abstract
Epidural analgesia has been used successfully in labor, postoperative, and chronic pain. Although in-dwelling epidural catheter carries the risk of infections, the tunneled epidural catheter can provide not only timely but also extended analgesia for cancer patients. The intrathecal pump has largely replaced short term epidural catheter use in cancer patients. The purpose of this case report is to demonstrate that epidural catheter remains an indispensable tool in managing refractory cancer pain not responding to systemic opioids.
Keywords: Cancer pain; Epidural analgesia; Catheter-associated infection
Introduction
Epidural analgesia has long been used to provide pain control in the acute perioperative setting. The duration of catheter placement rarely exceeds seven days for concerns of catheter-associated infection. However, some patients require prolonged analgesia, and tunneled epidural catheter has been used successfully to provide extended analgesia with minimal catheter-associated adverse events. We here present a case of tunneled epidural catheter used for a cancer patient undergoing radiation therapy to demonstrate that this remains an invaluable tool in managing cancer pain refractory to systemic opioids.
Case Description
The patient is a 35-year-old male with myxoid liposarcoma of the left proximal thigh with metastases to the left psoas muscle, liver, pancreas, lungs, and spine. He has extensive metastatic tumors from the cervical spine to sacrum, with significant lesions at vertebral bodies with epidural spread resulting in Bilsky type III cord compression at T10, T11, and L3 (Figure 1). He has severe positional back pain and bilateral distal lower extremity weakness as sequelae. The patient was undergoing radiation therapy; however, he could not tolerate supine position because of pain despite a large dose of oral and parenteral opioids therapy along with adjuvant medications. Chronic pain service was consulted and decided to place a tunneled epidural catheter for pain control.
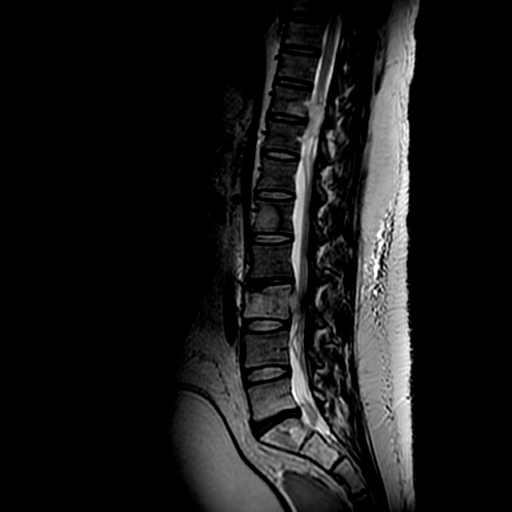
Figure 1: Thoracic and Lumbar MRI shows multiple metastatic lesions and epidural tumors causing cord compression.
The patient was taken to the operating room, and a thoracic epidural catheter was placed under fluoroscopy guidance. Patient in a prone position, the epidural space was accessed via mid-line L1-L2 interlaminar space using 17 gauge Tuohy needle. Under the fluoroscopy guidance, the Arrow® TheraCath® epidural catheter with a wire-reinforced body with a soft spring-wire tip was advanced to the T11 vertebral level until resistance was felt. The further attempt to advance the catheter resulted in a loop formation at L1. (Figure 2) Then a 5 mm vertical incision was made at skin from the Touhy entry site inferiorly, and a second Touhy was advanced subcutaneously from 8 cm inferior-lateral to the midline incision site. When the second Touhy needle tip was visualized, the midline Tuohy was slowly removed under the fluoroscopy guidance while maintaining the catheter tip location at T11. Then the catheter end was passed through the second Tuohy needle tip in a retrograde manner followed by removal of the second Touhy needle. The skin was closed with 4.0 Prolene, and the catheter was secured using Tegaderm and tapes.

Figure 2: Intraoperative fluoroscopic image demonstrates the epidural catheter tip at the level of T11 inferior boarder. Note the curved catheter at distal end due to resistance when catheter was advanced.
The patient reported significantly improved analgesia with continuous epidural infusion using bupivacaine-hydromorphone 0.075%-10mcg/ml mixture. Interestingly his pain was temporarily worsened with an epidural bolus dose, likely owing to the acute increase in epidural pressure. His pain improved after the infusion rate was increased from 8ml/hr to 10ml/hr. Visual analog scale (VAS) score decreased from 5-8/10 to 0-4/10 before and after epidural catheter placement, respectively. Patient was continued on systemic opioids and adjuvant therapy and showed no sign of respiratory depression, hypotension, or altered mental status. He had no worsening of lower extremity weakness. He successfully completed five radiation treatment sessions. The epidural catheter was removed 13 days after placement without signs of infection or hematoma. The patient was discharged to a rehabilitation facility.
Discussion
Since its introduction to North America in 1942, epidural analgesia has been widely used in thoracic, abdominal and obstetric surgeries, with improved postoperative pain control and decreased morbidity and mortality, shortened hospital stay, fewer thromboembolic incidents, and better pulmonary outcomes [1-3]. The safety of epidural catheters has been of great interest among anesthesiologists since catheter-related infections can vary from superficial skin infection at the insertion site to meningitis and epidural or spinal abscess requiring surgical intervention. The incidence of spinal epidural abscess after epidural analgesia varies from 0.05% to 0.11% [4,5]. Risks of infection are associated with underlying disease, multiple skin punctures before catheter placement, and sterile technique. Studies have suggested that prolonged catheter duration is associated with increased infection. The optimal duration of catheter placement has yet to be defined. American Society of Anesthesiology Task Force on Infectious Complications Associated with Neuraxial Techniques advises that epidural catheters should not remain in situ longer than clinically necessary [6].
The tunneled epidural catheter was introduced in the late 1980s to provide prolonged analgesia for both cancer and non-cancer pain [7-9]. The efficacy of tunneling to decrease infection is controversial. While some authors argue that prolonged epidural catheter analgesia should be reserved for cancer patients with a short life expectancy due to high infection rate [10], other studies have shown that tunneled epidural catheter can be used safely for an extended period of time [11,12]. Bomberg et al. conducted a retrospective study in 22,411 patients receiving thoracic epidural analgesia between 2007 and 2014 and concluded that tunneling is associated with fewer catheter-related infections (4.5 vs. 5.5%, P < 0.001) [13]. It should be noted that the aforementioned study was conducted in hospitalized patients who most likely were examined frequently. Bubeck et al., cultured 409 caudal or lumbar epidural catheters and found a positive correlation between bacterial colonization and redness at the catheter entry site [14]. Therefore, it is crucial for both providers and patients to remain high vigilance for signs of superficial infection or inflammation.
With the advancement of neuromodulation techniques, the popularity of tunneled epidural analgesia has decreased in recent years. However, those implanted devices are more invasive, costly, and carry higher risks for adverse events. Moreover, it can be technically challenging in patients with a spinal tumor or previous back surgeries. The tunneled epidural catheter remains a useful modality. It can provide timely analgesia with minimum invasiveness for cancer patients with refractory pain that prevent them from undergoing treatment, or for terminally ill patients with short life expectancy [15,16] who would not be a candidate for implanted devices. The routine use of fluoroscopy can increase the success rate of epidural catheter placement [17] and should be encouraged. Moreover, every effort should be made to perform an aseptic technique, decrease procedure time, and inspect the catheter site daily to prevent infections.
Conclusion
The tunneled epidural catheter can be a useful therapy for patients in need of prolonged analgesia. The risk of infection is low if the catheter is managed with vigilance.
References
- Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, Wu CL (2003). Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA, 290: 2455-2463.
- Ballantyne JC, Carr DB, deFerranti S, Suarez T, Lau J, Chalmers TC, Angelillo IF, Mosteller F (1998). The cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 86(3):598–612.
- Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S (2000). Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overviews of randomised controlled trials. BMJ 321: 1493.
- Wang LP, Hauerberg J, Schmidt JF (1999). Incidence of spinal epidural abscess after epidural analgesia: A national 1-year survey. Anesthesiology 91:1928–36.
- Christie IW, McCabe S (2007). Major complications of epidural analgesia after surgery: Results of a six-year survey. Anaesthesia 62:335–41.
- Practice Advisory for the Prevention, Diagnosis, and Management of Infectious Complications Associated with Neuraxial Techniques: An Updated Report by the American Society of Anesthesiologists Task Force on Infectious Complications Associated with Neuraxial Techniques and the American Society of Regional Anesthesia and Pain Medicine (2017). Anesthesiology 126(4):585-601.
- Malone BT, Beye R, Walker J (1985). Management of pain in the terminally ill by administration of epidural narcotics. Cancer. 55(2):438-40.
- Aldrete JA (1997). Extended epidural catheter infusion with analgesics for patients with noncancer pain at their homes. Regional Anesthesia 22(1):35-42.
- Blomberg SG (1994). Long-term home self-treatment with high thoracic epidural anesthesia in patients with severe coronary artery disease. Anesth Analg. 79(3):413-21.
- Smitt PS, Tsafka A, Teng-van de Zande F, van der Holt R, Elswijk-de Vries I, Elfrink E, van den Bent MJ, Vecht CJ (1998). Outcome and complications of epidural analgesia in patients with chronic cancer pain. Cancer. 83(9):2015-22.
- Du Pen SL, Peterson DG, Williams A, Bogosian AC (1990). Infection during chronic epidural catheterization: diagnosis and treatment. Anesthesiology 73: 905–9.
- Aram L, Krane EJ, Kozloski LJ, Yaster M (2001) Tunneled epidural catheters for prolonged analgesia in pediatric patients. Anesth Analg. 92(6):1432–1438.
- Bomberg H, Kubulus C, Herberger S, Wagenpfeil S, Kessler P, Steinfeldt T, Standl T, Gottschalk A, Stork J, Meissner W, Birnbaum J, Koch T, Sessler DI, Volk T, Raddatz A (2016). Tunnelling of thoracic epidural catheters is associated with fewer catheter-related infections: a retrospective registry analysis. Br J Anaesth. 116(4):546–553.
- Bubeck J, Boos K, Krause H, Thies KC (2004). Subcutaneous tunneling of caudal catheters reduces the rate of bacterial colonization to that of lumbar epidural catheters. Anesth Analg. 99(3):689-93.
- Chambers WA (2008). Nerve Blocks in Palliative Care. Br J Anaesth. 101(1):95-100.
- Padalia RB, Reeves CJ, Shah N, Patel AA, Padalia DM. (2017). Case report: bilateral tunneled epidural catheters to prevent unilateral analgesia for cancer-related pain. Local Reg Anesth. 10:79–82.
- Parra MC, Washburn K, Brown JR, Beach ML, Yeager MP, Barr P, Bonham K, Lamb K, Loftus RW (2017). Fluoroscopic Guidance Increases the Incidence of Thoracic Epidural Catheter Placement Within the Epidural Space: A Randomized Trial. Reg Anesth Pain Med. 42(1):17–24.
Citation: Yinan Chen, Dalya N. Elhady, Ngoc B. Truong and Billy Huh. (2020). The Tunneled Epidural Catheter Can Provide Timely Analgesia for Refractory Cancer Pain – A Case Report. Journal of Medical Research and Case Reports 2(3). DOI: 10.5281/zenodo.3769034
Copyright: © 2020 Billy Huh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
