Mini Review
Volume 3 Issue 1 - 2021
The Role of Upper Airway Evaluation by Drug-Induced Sleep Endoscopy (DISE) on Obstructive Sleep Apnea (OSA)
Department of Otorhinolaryngology, Head and Neck Surgery, Faculty of Medicine, Andalas University, Padang, Indonesia
*Corresponding Author: Yayan Akhyar, Department of Otorhinolaryngology-Head and Neck Surgery, Faculty of Medicine, Andalas University, Padang, Indonesia.
Received: May 22, 2021; Published: July 01, 2021
Abstract
Introduction: DISE can provide important information about the dynamics of the patient's airway which may alter treatment recommendations. DISE is a diagnostic method used for evaluation of the upper airway, favored by patients and physicians because of its short duration and clear results.
Literature Review: DISE is a flexible fiberoptic endoscopic examination performed during sleep induced by a sedative agent that facilitates trans-nasal endoscopy into the pharynx without waking the patient up. The advantages of DISE include not only the ability to visualize multiple levels of the upper airway, but also provide a close-up view of the anatomy and physiology of the upper airway during sleep.
Conclusion: DISE is recommended to obtain information in determining the combination of management procedures in OSA. Propofol is the sedative agent of choice in the DISE procedure. DISE examination is a valid, dynamic, safe, and easy to perform examination, and is closest to the state of sleep.
Keywords: Drug-induced sleep endoscopy; Obstructive sleep apnea; Upper airway; Endoscopy
Drug-Induced Sleep Endoscopy
DISE is a flexible fiberoptic endoscopic examination performed during sleep with the induction of a sedative agent that facilitates trans-nasal endoscopy into the pharynx without waking the patient. It was first described by Croft and Pringle in 1991. [1] This procedure allows better exploration of the nasal and pharyngeal state during sleep and can evaluate the possible site of collapse/cause of obstruction in OSA. Relatively fast and simple procedure which can be performed on an outpatient basis. [2,3] Is a diagnostic technique that allows for 3-dimensional visualization of the anatomy of an upper airway obstruction. [4]
DISE is a flexible fiberoptic endoscopic examination performed during sleep with the induction of a sedative agent that facilitates trans-nasal endoscopy into the pharynx without waking the patient. It was first described by Croft and Pringle in 1991. [1] This procedure allows better exploration of the nasal and pharyngeal state during sleep and can evaluate the possible site of collapse/cause of obstruction in OSA. Relatively fast and simple procedure which can be performed on an outpatient basis. [2,3] Is a diagnostic technique that allows for 3-dimensional visualization of the anatomy of an upper airway obstruction. [4]
DISE can provide important information about the dynamics of the patient's airway which may alter treatment recommendations. [5] The identification and characterization of the area evaluated during the examination can assist the surgeon in developing a plan of action with a view to improving the outcome of surgery. Patients who may benefit from the use of oral devices can also be identified because this method allows assessing the effect of mouth closure and jaw thrust during the examination. [6] A detailed evaluation of the degree, degree, and pattern of obstruction in OSA patients will lead to the choice of surgical technique and results of better management. [5,7]
The advantages of DISE include not only the ability to visualize various levels of the airway to assess the potential for collapse, but also that this method provides an approximation of the anatomical and physiological state of the upper airway during sleep. [6,8] It is also advantageous because it is performed in real time in correlation. By measuring oximetry rather than providing a static image, as is done in the Muller maneuver examination technique and several other diagnostic measures. [8] Although there is no consensus on standardization in clinical examination, the type of sedative agent and classification system used, the results obtained strongly recommend DISE in determining area of obstruction in a patient with OSA. DISE reported is a valid, dynamic, safe, and easy to perform check. [9]
Evaluation of the Upper Airway with DISE
Various classifications have been reported such as Bachar, Boudewns, Chan, Fishman, Sleep Endoscopy Rating Scale (SERS), Velum, Oropharynx and lateral pharyngeal wall, Tongue base and Epiglottis (VOTE) and Nasal, Oropharynx, Hypopharynx, Larynx (NOHL) to describe the findings. DISE. [10] Although there is no consensus, the VOTE classification and NOHL classification are the most widely used. [11,12]
Various classifications have been reported such as Bachar, Boudewns, Chan, Fishman, Sleep Endoscopy Rating Scale (SERS), Velum, Oropharynx and lateral pharyngeal wall, Tongue base and Epiglottis (VOTE) and Nasal, Oropharynx, Hypopharynx, Larynx (NOHL) to describe the findings. DISE. [10] Although there is no consensus, the VOTE classification and NOHL classification are the most widely used. [11,12]
The VOTE classification combines the four main structures that contribute to upper airway obstruction in most patients namely the velum, lateral oropharyngeal wall, tongue base, and epiglottis (Figure 1). [12,13] The NOHL classification provides an overview that includes the nose, oropharynx, hypopharynx, and larynx. These two classifications shared most of the parameters for identifying the location, degree of collapse, and pattern of upper airway obstruction (Table 1). The NOHL classification has the advantage of providing additional coverage of information on nasal obstruction. In contrast, other studies have shown that the VOTE classification provides a more comprehensive picture in the assessment of the pharynx and epiglottis. [14] The relationship between the severity of OSA and the number of sites affected is significant according to the VOTE classification. [12]
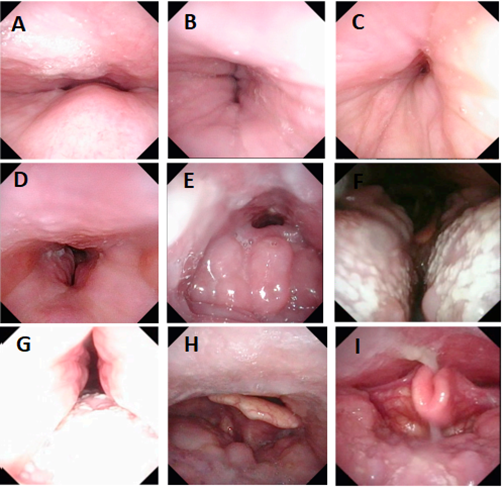
Figure 1: Overview of collapses observed in various areas. (A) Velum A-P. (B) Lateral velum. (C) Circular velum. (D) Lateral oropharynx. (E) Base of A-P tongue due to lymphoid hypertrophy. (F) The base of the tongue is sideways, noting that the base of the tongue is curved like a book. (G) Concentricity of the base of the tongue, there is A-P movement of the tongue and the lateral walls also contribute to collapse. (H) Epiglottis A-P. (I) Lateral epiglottis [13].
Qualitative assessment of the degree of upper airway collapse in the VOTE classification is divided as follows: [6,15]
- None; usually without vibration of the structures involved and airway narrowing of less than 50% compared to dimensions during non-apnea
- Partial; vibration, 50-75% narrowing
- Complete; obstruction, more than 75% narrowing, and no airflow.
It is sometimes difficult to group between the three categories above, because sometimes the findings of collapse and vibration of the upper airway in the OSA patient who are evaluated may change during the examination. [13] Although evaluation of the degree of obstruction has been shown to have moderate reliability. At one level, the area of the upper airway is found partial collapse (vibration, snoring), while at the level of another area there may be complete collapse. [6]
| Structure | Degree | Configuration | |||
| VOTE | Velum Lateral wall of the oropharynx Base of tongue Epiglottis |
0: absent 1: partial 2: complete |
Anteroposterior Not visible Anteroposterior Anteroposterior |
Lateral Lateral Not visible Lateral |
Concentric Not visible Not visible Not visible |
| Obstruction | Level | Configuration | |||
| NOHL | Nose Oropharynx Hypopharynx Larynx (supraglottic) |
1:0-25% 2:25-50% 3:50-75% 4:75-100% + / - |
- Anteroposterior Anteroposterior - |
- Lateral Lateral - |
- Concentric Concentric - |
Table 1: Assessment of the VOTE and NOHL classification systems on the DISE findings. [14].
DISE examination is a fairly simple examination, but there are several things that must be considered before and after doing this action: [6,13]
- Security; if DISE is not performed in the operating room, check to make sure that basic resuscitation equipment is available (oxygen supply, bag-valve mask)
- Sedation; sedation level is very important. The patient should not respond to verbal stimuli but still be able to respond to pain stimuli.
- Patience; sedation levels cannot be reached too quickly (within 2 or 3 minutes). If a sedative is injected too quickly, the patient will be overexposed, causing severe upper airway collapse without snoring. Ideally, the upper airway should be observed while the patient is snoring. Although rare, some patients do not snore significantly.
- Management of secretions; if too much saliva, it may be difficult to observe the airway collapse that is observed. Cleansing secretions by endoscopic suction is the best option. If that is not possible, then careful suction with the cannula through the mouth or nose can be performed. Avoid the possibility of injuring the mucosa because a proper DISE examination cannot be done in the presence of blood.
- Maneuvers; Chin lift and jaw thrust (Esmarch's maneuver) should still be performed in every patient, even if there is no collapse of the tongue base or when MAD is not considered a treatment option. It should be remembered that there are different types of the base of the tongue, and the top of the tongue overlaps the palate. Some palatal collapses are caused by the tongue. This maneuver can help distinguish true or not palatal collapse. Other maneuvers should also be considered (lateral position and nasopharyngeal tube insertion) as these can provide valuable additional information.
- Classification; although there is no consensus, a classification system is useful for reporting findings. This will help to compare the results between the patients examined and learn from the experiences of other centers.
- Duration; DISE takes about 15-30 minutes. Longer observations are useless, because the upper airway becomes full of saliva due to inhibition of deglutition by propofol.
- Writing reports; The post-DISE procedure report should state the sedation level, lowest oxygen saturation, sedative agent used (including the method of administration and dose used to achieve the target sedation level), findings in the upper airway, and maneuvers during the DISE examination.
- Adjunctive therapeutic agents; local anesthetics and nasal decongestants are not recommended, nor is the use of atropine in order to reduce upper airway secretions.
Outcome DISE on OSA
DISE's goal is to guide the selection of OSA management. The most important outcome is perhaps the relationship between the DISE findings and the results of the various examinations and interventions. Various studies have examined such questions. One study showed that DISE can change management recommendations in 78% of cases. [15] Each of the imaging findings on DISE examination has an important role in determining which combination of surgical procedures can be an option for a particular patient. [8,16] Alternative CPAP treatment suggested from DISE findings and the results of the polysomnogram (Table 2). In some cases, the patient may need more than one alternative for management that yields satisfactory results. [8]
DISE's goal is to guide the selection of OSA management. The most important outcome is perhaps the relationship between the DISE findings and the results of the various examinations and interventions. Various studies have examined such questions. One study showed that DISE can change management recommendations in 78% of cases. [15] Each of the imaging findings on DISE examination has an important role in determining which combination of surgical procedures can be an option for a particular patient. [8,16] Alternative CPAP treatment suggested from DISE findings and the results of the polysomnogram (Table 2). In some cases, the patient may need more than one alternative for management that yields satisfactory results. [8]
| DISE Findings | OSA Severity | Alternative management |
| Palatal flutter/vibration | UARS, mild, moderate, severe | Palatal stiffening (pillar implant; RF ablation) |
| Uvular prolapse | UARS, mild, moderate, severe | Partial uvulectomy |
| Partial or total collapse of the palate, AP (banana shaped lumen) | Moderate to severe | UPPP |
| Partial or total palate collapse, concentric (funnel shaped lumen) | Moderate to severe | Expansion Pharyngoplasty |
| Tonsillar collapse | UARS, mild, moderate, severe | Tonsillectomy |
| Lateral oropharyngeal wall collapse | Moderate to severe | Expansion pharyngoplasty; oral appliance |
| Partial or total lingual tonsil compression | UARS, mild, moderate, severe | Reduction of lingual tonsils |
| Partial or complete collapse of the tongue, macroglossia | Mild | Mild RF ablation of the base of the tongumilde; SMILE procedures; oral appliance |
| Moderate-severe | Partial glossectomy; upper airway stimulation; oral appliance | |
| Partial or total collapse of the tongue, normal tongue size, poor tongue tension | Mild-moderate | Genioglossal Advance-ment; oral appliance |
| Severe | Stimulation of the upper airway | |
| Partial or complete collapse of the tongue, class II / III malocclusion, open bite, retrognathia | Moderate-severe | Maxillo-mandibular advancement (MMA) |
| Epiglottic collapse, open vallecula and no tongue depression | UARS, mild, moderate, severe | Partial epiglottectomy |
| Epiglottic collapse, closed vallecula and tongue compression | Mild, moderate, severe | Hyoid suspension |
| * RF= radiofrequency; SMILE=Submucosal minimally-invasive lingual excision | ||
Table 2: Suggested alternative (non-CPAP) management of DISE findings and polysomnogram results on OSA. [8]
The results obtained from DISE can help predict a positive response to surgical intervention; therefore, it has been generally accepted as an important part of the surgical evaluation of OSA. It is recommended to offer DISE in order to minimize and optimize procedures for the identification and evaluation of OSA patients. 5 In conjunction with CPAP, DISE can provide a better understanding of the need to regulate higher CPAP pressure in the subgroup of patients with OSA. At the same time, DISE can be a tool to identify the indications for oral appliance therapy or surgery to lower the level of CPAP titration needed. The findings on DISE can provide important data for use in prospective decision making in OSA patients, including potential combination therapy, to improve the clinical effectiveness of management.
DISE limitation
There are several limitations of DISE as an evaluation tool for OSA: [11,14]
There are several limitations of DISE as an evaluation tool for OSA: [11,14]
- Natural sleep is not reproduced accurately in duration or quality
- In contrast to polysomnography, DISE does not reflect information throughout the night. Therefore, the findings in DISE could be a brief overview of the incidence of sleep at night.
- Unlike SVF, the entire airway cannot be seen all at once on DISE.
- Standardization of sedation and evaluation procedures is still limited. Although some standardization procedures for the use of sedatives on hospital-based DISE and evaluation systems have been established.
- There is no gold standard validation for the findings and classification used.
Conclusion
Identifying the pattern and pathophysiology of airway obstruction in OSA is essential. DISE is a diagnostic tool by assessing areas of vibration and upper airway obstruction during sleep which is recommended for patients with OSA to obtain information that plays an important role in determining the combination of management procedures. Propofol is the sedative agent of choice in the DISE procedure. DISE examination is a valid, dynamic, safe, easy to perform examination, and is the closest to anatomical and physiological conditions during sleep in people with OSA.
References
- Baldassari CM, Lam DJ, Ishman SL, et al. (2021). Expert Consensus Statement: Pediatric Drug-Induced Sleep Endoscopy. Otolaryngol - Head Neck Surg (United States). Published online 1-14.
- Blumen M, Bequignon E, Chabolle F. (2017). Drug-induced sleep endoscopy: A new gold standard for evaluating OSAS? Part I: Technique. Eur Ann Otorhinolaryngol Head Neck Dis. 134(2): 101-107.
- Cheong CS, Loke W, Thong MKT, Toh ST, Lee C-H. (2021). The Emerging Role of Drug-Induced Sleep Endoscopy in the Management of Obstructive Sleep Apnea. Clin Exp Otorhinolaryngol. 17(4): 1-10.
- Yalim SD. (2018). Drug-Induced Sleep Endoscopy and Our Cl?n?cal Exper?ences. J Pharm Res Int. 22(5): 1-4.
- Ghazizadeh S, Moore K, Kiai K, Mendelsohn AH. (2020). Drug-Induced Sleep Endoscopy Performed in the Endoscopy Suite: A Resource Utilization Analysis. Otolaryngol - Head Neck Surg (United States). 162(3): 386-391.
- Hohenhorst W, Ravesloot MJL, Kezirian EJ, De Vries N. (2012). Drug-induced sleep endoscopy in adults with sleep-disordered breathing: Technique and the VOTE Classification system. Oper Tech Otolaryngol - Head Neck Surg. 23(1): 11-18.
- Gazzaz MJ, Isaac A, Anderson S, Alsufyani N, Alrajhi Y, El-Hakim H. (2017). Does drug-induced sleep endoscopy change the surgical decision in surgically naïve non-syndromic children with snoring/sleep disordered breathing from the standard adenotonsillectomy? A retrospective cohort study. J Otolaryngol - Head Neck Surg. 46(1): 1-8.
- Kohn JL, Boyd Gillespie M. (2015). Drug-induced Sleep Endoscopy. Oper Tech Otolaryngol - Head Neck Surg. 26(2): 66-73.
- Viana A da C, Thuler LCS, Araújo-Melo MH de. (2015). Drug-induced sleep endoscopy in the identification of obstruction sites in patients with obstructive sleep apnea: A systematic review. Braz J Otorhinolaryngol. 81(4): 439-446.
- Williamson A, Ibrahim SR, Coutras SW, Carr MM. (2020). Pediatric Drug-Induced Sleep Endoscopy: Technique and Scoring System. Cureus. 12(10): e10765-71.
- Hong S-N, Won T-B, Kim J-W, Lee CH, Rhee C-S. (2016). Upper Airway Evaluation in Patients with Obstructive Sleep Apnea. Sleep Med Res. 7(1):1-9.
- Viana A da C, Mendes DL, de Andrade Lemes LN, Thuler LCS, Neves DD, de Araújo-Melo MH. (2017). Drug-induced sleep endoscopy in the obstructive sleep apnea: comparison between NOHL and VOTE classifications. Eur Arch Oto-Rhino-Laryngology. 274(2): 627-635.
- Carrasco-Llatas M, Matarredona-Quiles S, De Vito A, Chong KB, Vicini C. (2019). Drug-Induced Sleep Endoscopy: Technique, Indications, Tips and Pitfalls. Healthcare. 7(3): 93-102.
- Kim JY, Han SC, Lim HJ, Kim HJ, Kim JW, Rhee CS. (2020). Drug-induced sleep endoscopy: A guide for treatment selection. Sleep Med Res. 11(1): 1-6.
- Charakorn N, Kezirian EJ. (2016). Drug-Induced Sleep Endoscopy. Otolaryngol Clin North Am. 49(6): 1359-1372.
Citation: Yayan Akhyar and Novialdi. (2021). The Role of Upper Airway Evaluation by Drug-Induced Sleep Endoscopy (DISE) on Obstructive Sleep Apnea (OSA). Journal of Otolaryngology - Head and Neck Diseases 3(1).
Copyright: © 2021 Yayan Akhyar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
