Review Article
Volume 2 Issue 2 - 2020
The Management of Periprosthetic Greater Trochanter Fractures: A Review
Guy’s and St Thomas’ NHS Foundation Trust, Westminster Bridge Road, London, SE1 7EH
*Corresponding Author: William D Groom, Guy’s and St Thomas’ NHS Foundation Trust, Westminster Bridge Road, London, SE1 7EH.
Received: November 13, 2020; Published: November 23, 2020
Abstract
Introduction: Despite periprosthetic greater trochanter fractures being a common injury, relatively little has been published specific to their management. This review explores the available evidence, including 6 case series detailing information regarding fracture classification, indications for fixation and fixation methods.
Materials and Methods: A literature search of Embase and MEDLINE databases from 1946 to March 2020 was conducted using a broad search strategy to identify all relevant published data.
Results: Six level IV studies alongside several case reports were identified and included in this review.
Conclusions: Comprehensive guidance based purely on quantative data is not possible, due to limited published evidence. However, this review collates and summarises the currently available evidence on how and when to treat these injuries, including a treatment algorithm.
Keywords: Greater Trochanter Fracture; Periprosthetic; Fixation; Management
Introduction
Much has been published regarding fixation of the greater trochanter (GT) with regards to primary and revision hip arthroplasty. The majority of these studies concern the reattachment of an osteotomized trochanter in the acute setting [1]. There are also published series dating back 80 years regarding the management of greater trochanter fractures in native hips [2,3]. Fractures of the GT after total hip replacement are relatively common, occurring in 3-5% of patients [4,5]. It is recognised that management of these fractures presents a challenge in terms of timing and method of intervention and, indeed, whether to intervene at all [6]. To the authors’ knowledge, there has been no published review on the available evidence. Our aim is to summarise the published data in order to help inform management of these fractures.
Materials and Methods
Literature Search
To identify all relevant material available relating to the diagnosis, classification and management of periprosthetic GT fractures, a literature search was conducted by the authors independently. The Embase and MEDLINE databases were searched for journal articles and abstracts on this topic from 1946 to March 2020. Only articles available in English were included.
To identify all relevant material available relating to the diagnosis, classification and management of periprosthetic GT fractures, a literature search was conducted by the authors independently. The Embase and MEDLINE databases were searched for journal articles and abstracts on this topic from 1946 to March 2020. Only articles available in English were included.
The keywords used were:
- “greater trochant*” AND “fractur*”
- “fixation*” OR “treatment*” OR “manag*”
- 1. and 2.
Eligibility Criteria
Both authors assessed each article based on the titles and abstracts and if eligibility was not clear, the entire article was read. The studies were included for analysis based on the following criteria:
Both authors assessed each article based on the titles and abstracts and if eligibility was not clear, the entire article was read. The studies were included for analysis based on the following criteria:
- The study must involve multiple patients with GT fractures with hemiarthroplasty or total hip replacement in situ
- The study must include rationale for the decision made to treat operatively or non-operatively
- The study must include outcomes for the selected treatment method
- If other periprosthetic fracture types were included in the study, data specific to the GT fractures must be reported
1. The study must be published in English
Results
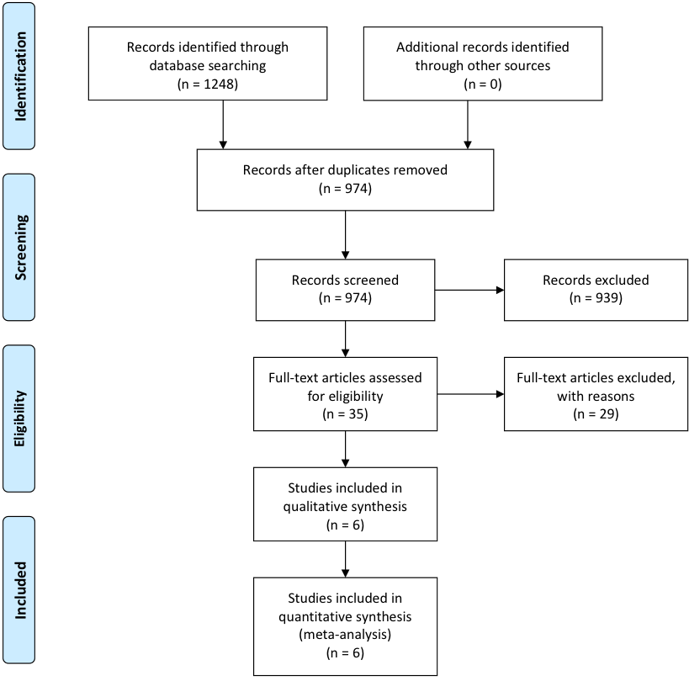
This produced 974 articles (Figure 1), of which 939 articles were excluded based on titles and abstracts. The full text of the remaining 35 articles were reviewed and the bibliographies of these were then reviewed for relevant citations. 29 of these studies were excluded as they did not meet the eligibility criteria. The 6 remaining studies were all retrospective case series including data specific to the management of periprosthetic GT fractures [4-9]. The management of 119 periprosthetic GT fractures in total were reviewed (Table 1).
| Study | Type of Hip Surgery | Number of GT Fractures | Female % | Mean Age/Range | Mean Follow-up | Osteolysis |
| Brun & Maansson (2013) | Reverse hybrid THR | 26 | 81 | 41-86 | N/A | N/A |
| Hendel et al. (2002) | Primary THR (uncemented, cemented and hybrid) or revision | 21 | 100 | 68 (59-75) | N/A | N/A |
| Hseih et al. (2005) | Uncemented THR | 23 | N/R | 51 | 48 months | All |
| Pritchett (2001) | Primary THR (uncemented, cemented & hybrid), hemiarthroplasty | 30 | 70 | 69 (48-84) | 40 months | N/A |
| Stewart et al. (2017) | N/A | 8 | N/R | N/R | 30 months | N/R |
| Tetreault & McGrory (2016) | Primary and revision THR | 11 | N/R | N/R | 42 months | Some cases |
Table 1: Case series identified specific to the management of periprosthetic GT fractures (N/R- data not reported).
Diagnosis
Acute fractures of the greater trochanter typically present with sudden onset lateral hip pain with or without a limp or Trendelenburg lurch [5]. There may be no or only minor trauma preceding the onset of symptoms, with patients often describing a sudden onset on walking or twisting. Up to 60% of patients are asymptomatic [6]. The surgical approach for the initial arthroplasty does not appear to be a risk factor for developing these fractures [4]. These injuries are most commonly diagnosed by plain radiography alone, although if there is a suspicion of extension distally and potential stem instability, computed tomography (CT) may be carried out [10].
Acute fractures of the greater trochanter typically present with sudden onset lateral hip pain with or without a limp or Trendelenburg lurch [5]. There may be no or only minor trauma preceding the onset of symptoms, with patients often describing a sudden onset on walking or twisting. Up to 60% of patients are asymptomatic [6]. The surgical approach for the initial arthroplasty does not appear to be a risk factor for developing these fractures [4]. These injuries are most commonly diagnosed by plain radiography alone, although if there is a suspicion of extension distally and potential stem instability, computed tomography (CT) may be carried out [10].
Classification
Brun and Maansson [4] proposed a classification system based on fracture pattern, divided into three groups:
Type 1: Fracture of the medial tip of the greater trochanter created at the time of the femoral neck osteotomy
Type 2: An avulsion-type fracture of only the medial tip of the greater trochanter
Type 3: A complete fracture of the greater trochanter (displaced or undisplaced)
Brun and Maansson [4] proposed a classification system based on fracture pattern, divided into three groups:
Type 1: Fracture of the medial tip of the greater trochanter created at the time of the femoral neck osteotomy
Type 2: An avulsion-type fracture of only the medial tip of the greater trochanter
Type 3: A complete fracture of the greater trochanter (displaced or undisplaced)
In their study, comparing the patient reported outcomes of these three fracture patterns with data from the Swedish and New Zealand hip registers, no significant changes in all measured values were reported for types 1 and 2. Type 3 fractures, however, produced significantly higher pain scores and lower Oxford Hip Score values than would be expected.
This classification does not consider several potentially significant features of this type of fracture. Pritchett highlighted the importance of fracture displacement in both patient reported outcome and potential to achieve union [6].
The second important feature to take into account is the bone quality of the fragment. Hsieh reported a significant proportion of delayed fractures through osteolytic cysts secondary to polyethylene wear particles[7]. Not only does this have implications for the technique that may be required for fixation of the fracture itself, but also raises questions about whether revision of the prosthesis is required [11].
The final factor to consider is whether instability of the hip joint is an issue. If the fracture leads to dislocation or was caused by a dislocation, the threshold for surgical intervention is significantly lowered [11].
Indications for Fixation
Historically, isolated GT fractures have been viewed as relatively benign injuries with early case series reporting that healing occurs regardless of treatment, with return to normal function in 2 months [2,3]. It is now more commonly accepted that outcomes can be significantly worsened in the presence of such a fracture [4].
Historically, isolated GT fractures have been viewed as relatively benign injuries with early case series reporting that healing occurs regardless of treatment, with return to normal function in 2 months [2,3]. It is now more commonly accepted that outcomes can be significantly worsened in the presence of such a fracture [4].
Pritchett recommended fixation based on the following indications[6]:
- Dislocation or instability of the prosthesis
- Severe limp or pain
- Displacement of the trochanter fracture of >2cm (compared with the contralateral hip)
That paper also reported that pain and limping resolved spontaneously in half of symptomatic fractures over a few months. There was not thought to be any adverse consequence in delayed treatment.
Hamadouche proposed a treatment algorithm for management of greater trochanter non-union which incorporated a positive Trendelenburg sign alongside fracture displacement, limp, pain and instability as a key factor when deciding whether fixation is necessary [12].
Method of Fixation
Multiple techniques for greater trochanter fixation have been described, although most published literature concerns fixation of an osteotomised trochanter, rather than following a fracture. There are several difficulties in directly comparing management options in these two distinct situations as important factors in bone healing may differ including blood supply, soft tissues and potential fibrous interposition [6]. However, due to a lack of evidence relating specifically to the management of periprosthetic greater trochanter fractures, considering fixation options for the greater trochanter in all circumstances is necessary.
Multiple techniques for greater trochanter fixation have been described, although most published literature concerns fixation of an osteotomised trochanter, rather than following a fracture. There are several difficulties in directly comparing management options in these two distinct situations as important factors in bone healing may differ including blood supply, soft tissues and potential fibrous interposition [6]. However, due to a lack of evidence relating specifically to the management of periprosthetic greater trochanter fractures, considering fixation options for the greater trochanter in all circumstances is necessary.
Historically, iatrogenic greater trochanter fractures observed intra-operatively have been fixed with mono or multifilament wires alone. In a case series of 15 patients with this complication, Hendel noted a 100% union rate with this method of fixation [5]. However, wire breakage has been reported in up to 20% of cases and catastrophic migration to the popliteal fossa and left side of the heart have been recorded [1].
Cable plating is another option which has been developed through several iterations. The first generation consisted of an H-shaped gripping device which was seated on the greater trochanter attached to several cables that passed medially. The updated second generation incorporated a filament bundle pattern, allowing provisional cable fixation. The current, third, generation is more anatomical and allows more uniform cable compression [13]. Unfortunately, in the setting of greater trochanter fractures, non-union rates as high as 35% have been reported, with cable failure in 29% of cases [8]. The quality of reduction and corresponding bony apposition has been noted as a key factor in the success of this method of fixation.
Locking plates are another described option, although little evidence is available on outcomes following fracture. An in vitro study comparing multifilament wires, cable plates and locking plates did not show any mechanical advantage in terms of compression, distraction loading and failure load tests between cable and locking plates, although both plates were superior to wires alone [14]. As part of a wider case series using this technique, Tetreault reported a union rate of 89% in 9 patients following periprosthetic fracture. The main complication of this technique is ongoing trochanteric pain, in 19% of patients [9].
Finally, in the presence of significant osteolysis, bone grafting together with revision of implants should be considered. In a case series of 19 patients with greater trochanter fracture secondary to osteolysis undergoing revision of implants, morselised femoral head bone graft was used together with monofilament wires [15]. 94% union was reported in this study. Demineralised bone matrix has been shown to be another useful adjunct [16].
Post-operatively, a range of protocols were used ranging from no restrictions of mobility to 6 weeks of non-weight bearing with no active hip abduction.
| Study | % Treated Non-operatively | Non-union % | Management | Complications |
| Brun & Maansson (2013) | 73 | N/A | Bed rest/protected weight bearing 3-4 weeks | Pain or limp in 70% of type 3 fractures |
| Hendel et al. (2002) | 29 | 33 (associated with dislocation | 2 weeks bed rest | Limp & pain |
| Hseih et al. (2005) | 83 | 21 | Crutch walking/activity restriction | 63% revised within 3 years |
| Pritchett (2001) | 70 | 50 | No restrictions | 29% of patients had persistent pain and limp |
| Stewart et al. (2017) | 0 | N/A | N/R | N/R |
| Tetreault & McGrory (2016) | 0 (all had failed non-op) | N/A | N/R | N/R |
Table 2: Results for fixation of periprosthetic GT fractures (N/R- data not reported).
| Study | % Fixed | Fixation Method | Non-union % | Post-op Management | Complications |
| Brun & Maansson (2013) | 27 | K-wires & cerclage or claw plate | N/A | N/A | N/R |
| Hendel et al. (2002) | 71 (all seen intra-operatively) | Wire fixation | 0 | N/A | Limp & pain |
| Hseih et al. (2005) | 17 | N/A- combined with revision | 0 | N/A | N/R |
| Pritchett (2001) | 30 | Cables/wire/ethibond suture | N/A | No restrictions | N/R |
| Stewart et al. (2017) | 100 | Cable plate | 35% | 6 weeks toe- touch/non-weight bearing and no abduction | Implant failure, infection, lateral hip pain |
| Tetreault & McGrory (2016) | 100 | Locking plate | 9% | Touch weight bearing for 4 weeks then partial weight bearing for 2 weeks, no abduction for 6 weeks | Trochanteric pain, 1 dislocation |
Table 3: Results for non-operative management of periprosthetic GT fractures (N/R- data not reported).
Discussion
Currently, there is limited data available to clinicians to aid decision making when confronted with an acute periprosthetic greater trochanter fracture. Published evidence consists of relatively small case series (level 4 evidence), often with limited sample sizes, and only 6 deal exclusively with this clinical problem (Tables 2 and 3). As a result, some extrapolation must be made from the available evidence relating to greater trochanter osteotomies and the fixation of non-unions. Even this data only consists of case series [1] so guidance based purely on quantative evidence is not possible.
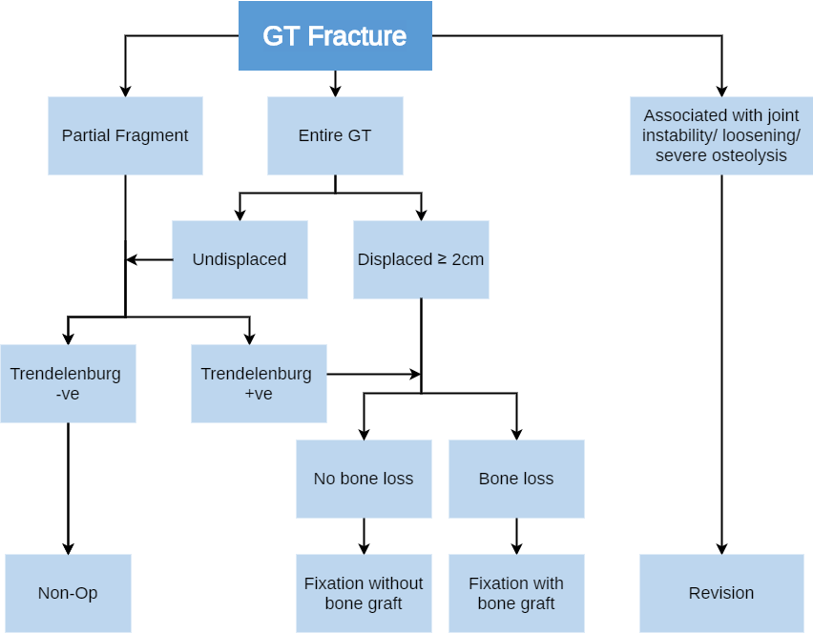
Based on the available evidence, the authors would recommend management of these injuries according to the algorithm in Figure 2. As with any periprosthetic fracture, consideration must first be given to whether the prosthesis remains viable or whether revision surgery is required. In symptomatic patients, the size of fracture fragment, fragment displacement, bone stock and presence of Trendelenburg’s sign should all be taken into account when considering fixation.
Conclusion
Based on the limited data available in the literature, it is not possible to firmly recommend a specific fixation method but clearly a frank discussion with the patient is required regarding potential benefits and risks of surgery, as well as timing of surgery. Many of these studies have reported high complication rates following surgery and, with so little quantative data available, the ultimate decision will rely on patient and surgeon preference.
References
- Mei XY, Gong YJ, Safir OA, Gross AE, Kuzyk PR. (2018). Fixation Options Following Greater Trochanteric Osteotomies and Fractures in Total Hip Arthroplasty: A Systematic Review. JBJS Rev. 6(6):e4.
- Merlino, A.F., Nixon JE. (1939). Isolated Fracture of the Greater Trochanter. Int J Surg. 1969;52:117-124.
- Milch H. Avulsion Fractures of the Greater Trochanter. Arch Surg. 38, 334-350.
- Brun, O-C. L, Maansson L. (2013). Fractures of the greater trochanter following total hip replacement. HIP Int. 23(2):143-146.
- Hendel D, Yasin M, Garti A, Weisbort M, Beloosesky Y. (2002). Fracture of the greater trochanter during hip replacement: A retrospective analysis of 21/372 cases. Acta Orthop Scand. 73(3):295-297.
- Pritchett JW. (2001). Fracture of the greater trochanter after hip replacement. Clin Orthop Relat Res. (390):221-226.
- Hsieh PH, Chang YH, Lee PC, Shih CH. (2005). Periprosthetic fractures of the greater trochanter through osteolytic cysts with uncemented MicroStructured Omnifit prosthesis: Retrospective analyses of 23 fractures in 887 hips after 5-14 years. Acta Orthop. 76(4):538-543.
- Stewart AD, Abdelbary H, Beaulé PE. (2017). Trochanteric Fixation With a Third-Generation Cable-Plate System: An Independent Experience. J Arthroplasty. 32(9):2864-2868.e1.
- Tetreault AK, McGrory BJ. (2016). Use of locking plates for fixation of the greater trochanter in patients with hip replacement. Arthroplast Today. 2(4):187-192.
- Giaretta S, Momoli A, Porcelli G, Micheloni GM. (2019). Diagnosis and management of periprosthetic femoral fractures after hip arthroplasty. Injury. 50:S29-S33.
- McGrory BJ. (2016). Use of locking plates for fixation of the greater trochanter in patients with hip replacement. Tech Orthop. 2013.
- Hamadouche M, Zniber B, Dumaine V, Kerboull M, Courpied JP. (2004). Reattachment of the ununited greater trochanter following total hip arthroplasty. J Bone Joint Surg Am. 86 A Suppl(Pt 2):112-118.
- Patel S, Soler JA, El-Husseiny M, Pegg DJ, Witt JD, Haddad FS. (2012). Trochanteric Fixation Using a Third-Generation Cable Device-Minimum Follow-Up of 3 Years. J Arthroplasty. 27(3):477-481.
- Sariyilmaz K, Korkmaz M, Özkunt O, et al. (2016). Comparison of fixation techniques in Vancouver type AG periprosthetic femoral fracture: A biomechanical study. Acta Orthop Traumatol Turc. 50(3):373-378.
- Wang JW, Chen LK, Chen CE. (2006). Surgical treatment of fractures of the greater trochanter associated with osteolytic lesions. Surgical technique. J Bone Joint Surg Am. 88 Suppl 1:250-258.
- Peretz JI, Chuang MJ, Cerynik DL, Johanson NA. (2009). Treatment of Symptomatic Greater Trochanteric Fracture After Total Hip Arthroplasty. J Arthroplasty. 24(5): 825.e1-825.e4.
Citation: William D Groom and Jerome A Davidson. (2020). The Management of Periprosthetic Greater Trochanter Fractures: A Review. Journal of Orthopaedic and Trauma Care 2(2). DOI: 10.5281/zenodo.4288609
Copyright: © 2020 William D Groom. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.