Review Article
Volume 3 Issue 1 - 2021
Obstructive Sleep Apnea (OSA) as a Cause of Sleep Disorders
Department of Otorhinolaryngology, Head and Neck Surgery, Faculty of Medicine, Andalas University, Padang, Indonesia
*Corresponding Author: Yayan Akhyar, Department of Otorhinolaryngology-Head and Neck Surgery, Faculty of Medicine, Andalas University, Padang, Indonesia.
Received: May 22, 2021; Published: June 03, 2021
Abstract
Introduction: OSA is a medical disorder characterized by repeated episodes of the upper airway closure during sleep. The correct diagnosis of OSA is essential, through a complete clinical history and thorough evaluation of the anatomical area of the upper airway.
Literature Review: The inability to recognize OSA can adversely affect health conditions, as this disease is associated with significant morbidity and mortality. Obesity is a major risk factor for the incidence of OSA. Surgical management was considered in patients with AHI> 15 events / hour and unable to tolerate or reject CPAP.
Conclusion: Identifying the pattern and pathophysiology of airway obstruction in OSA is essential. The gold standard examination for OSA is polysomnography. An initial oropharyngeal anatomical evaluation to predict success management of OSA patients is necessary.
Keywords: Drug-induced sleep endoscopy; Obstructive sleep apnea; Upper airway; Endoscopy
Introduction
Sleep disorder breathing (SDB) is a condition with the manifestation of snoring, which can be caused by upper airway resistance syndrome (UARS), obstructive sleep apnea hypopnea syndrome (OSAHS), and obstructive sleep apnea (OSA). [1,2] OSA is a medical disorder characterized by repeated episodes of the upper airway closure during sleep. It is a common, often unrecognized, medical disorder characterized by repeated episodes of closure of the upper airway during sleep. [3] These episodes result in stopping or significant reduction of airflow in ongoing breathing attempts. [4]
The prevalence of OSA depends on the population of cases studied; atrial fibrillation 32-49%, myocardial infarction 60-65%, persistent arterial hypertension 64-83%, heart failure 50-68%, obesity 71-78%, and stroke 50-70% . [4] An estimated 14% in men and 5 % in women. A higher prevalence was also found in patients with diabetes mellitus type 2. [4,5] OSA is very rare in nonobesity and pre-menopausal women. The prevalence of OSA is also reported to increase with age, especially in people over 60 years of age. [6]
Various clinical prediction methods are used to assist in diagnosing patients with OSA probability, [7] including the Sleep Apnea Clinical Score, Epworth Sleepiness Scale (ESS), Berlin Questionnaire, STOP-Bang, Cricomental Distance, OSA50, Elbow Sign Questionnaire and checklists from the American Society. of Anesthesiologists. This instrument has been validated in a population with a high prevalence. Nonetheless, ESS is the most widely used although it does not accurately identify patients with OSA, it is useful for evaluating subjective sleep disturbances and treatment response. [8]
Obstructive Sleep Apnea
The correct diagnosis of OSA is essential and the assessment procedure should provide a complete clinical history as well as a thorough evaluation of the anatomical area of the upper airway. Polysomnographic studies are considered the gold standard for diagnosing sleep apnea, [9] because they can provide complete information on the severity of OSA, the patient's clinical status, and possible complications. [10] OSA is generally the result of anatomically multilevel obstruction of the upper airway. Imaging such as computed tomography (CT-Scan) or magnetic resonance imaging (MRI), cephalometric studies, as well as drug-induced sleep endoscopy (DISE), and even analysis of snoring sounds can help provide information in the diagnostic evaluation of OSA. It is important to have an efficient and non-invasive evaluation strategy to detect anatomical abnormalities of patients with OSA in planning treatment and surgery. [11,12]
The correct diagnosis of OSA is essential and the assessment procedure should provide a complete clinical history as well as a thorough evaluation of the anatomical area of the upper airway. Polysomnographic studies are considered the gold standard for diagnosing sleep apnea, [9] because they can provide complete information on the severity of OSA, the patient's clinical status, and possible complications. [10] OSA is generally the result of anatomically multilevel obstruction of the upper airway. Imaging such as computed tomography (CT-Scan) or magnetic resonance imaging (MRI), cephalometric studies, as well as drug-induced sleep endoscopy (DISE), and even analysis of snoring sounds can help provide information in the diagnostic evaluation of OSA. It is important to have an efficient and non-invasive evaluation strategy to detect anatomical abnormalities of patients with OSA in planning treatment and surgery. [11,12]
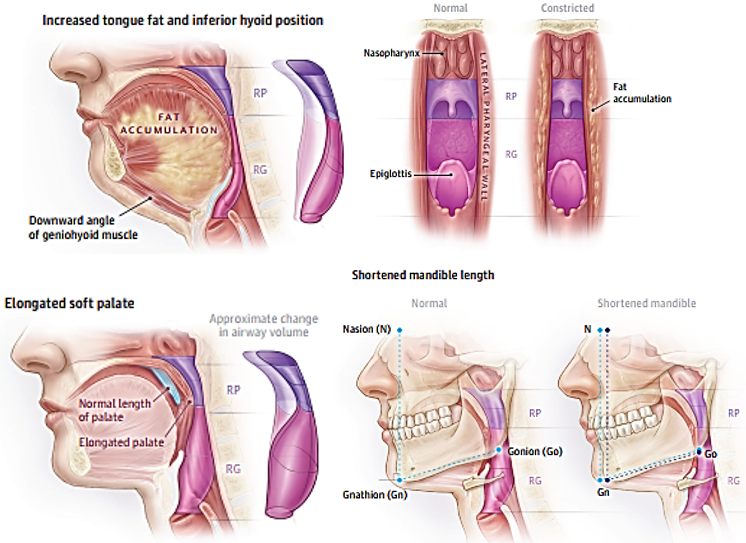
Obesity is a major risk factor for the incidence of OSA. [5,13–16] Changes in the anatomy of the mole palate, mandibular abnormalities, and deposition of fat in the pharynx during sleep in obese patients will increase the risk factors for upper airway obstruction (Figure 1). [16] Central obesity is associated with decreased lung volume, resulting in decreased caudal traction in the upper airway. This causes an increase in the incidence of pharyngeal collapse. [2] Patients with a BMI> 40 have an increase in the incidence of sleep apnea by 40-90%. Genetic predisposition and family history also play a role in OSA. A history of OSA in the first lineage family will increase the risk factors to 1.5–2 times. Obesity is closely related to family history, so the incidence of OSA cannot be separated. [9]
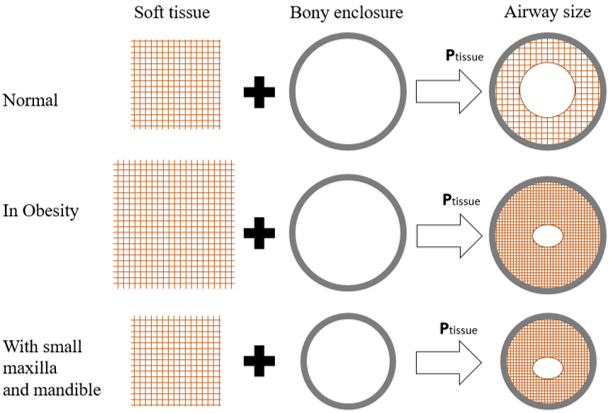
The factors most commonly associated with OSA in adults and children are upper airway collapse, narrowed lumen size, and skeletal abnormalities (Figure 2). [9,17] Despite these considerations, adults and children may have different etiologic factors that predispose them. the occurrence of OSA. [17] The peak incidence in children is the preschool age range of 2-5 years according to the period when the adenoid glands and palatine tonsils show maximal development compared to the oropharyngeal space. [15] Although adenoid hypertrophy is a significant risk factor for OSA in children, none absolute relationship between the size of the palatine tonsils and adenoids and the severity of respiratory distress during sleep. Obesity is becoming an increasingly important and common risk factor for OSA in children and during adolescence. [18]
The oropharynx and hypopharynx are easy to collapse due to the absence of bone or cartilage structures that support lumen patency. Factors that facilitate the collapse of these structures are muscle activity, the ability to collapse the intrinsic airway, and an active and passive mechanical nervous system. [2] When humans breathe, negative intrathoracic pressure is formed, thereby reducing the transverse area of the pharynx. [9]
In the last decade, there have been significant advances in understanding the pathophysiology of OSA. There are four main traits or phenotypes that contribute to OSA: [1,14]
- Anatomical obstruction of the narrow or collapsed upper airway
- Low Arousal threshold
- Inadequate response of the airway dilator muscles during sleep
- Unstable or overly sensitive breathing control, a concept called high loop gain.
Other factors that can contribute to the pathophysiology of OSA include head posture and vascular supply to the mucosa and tissues around the airway, and genetic factors. Changes in blood pressure and/or vascularization of the pharyngeal muscles can affect airway stability and patency. The mucosal blood flow causes constriction if it swells. On the other hand, neck flexion and extension affects the upper airway mechanism because the axis of rotation for extension and flexion is behind the upper airway. Thus, changes in sleeping position, especially supine, can increase upper airway collapse and predispose to OSA especially in adults. OSA has been shown to significantly run in families. Genetic factors tend to determine the anatomy of the upper airway, neuromuscular activity, and stability of ventilation control; these factors produce the phenotype of the OSA syndrome. [9] Upper airway permeability is influenced by a balance between the factors that play a role at collapse and the factors that keep the airway patency maintained, which is called the “the balance of pressure concept”. This balance involves pharyngeal skeleton, compliance with airway collapse, negative intraluminal pressure, external pressure, and extra lumen positive pressure (Figure 3). [2,9]
Compliance or ability to collapse of the airway, depending on changes in airway volume and changes in airway pressure (δV/δP). Negative intraluminal pressure in the airway (intraluminal pressure), which comes from inspiratory muscles such as the diaphragm, intercostal muscles can constrict the airway. Pressure on the external pharyngeal wall for example compression on the lateral pharynx and submandibular fat, and the large tongue against the small oral cavity. Extra lumen positive pressure is influenced by abduction contraction of the pharyngeal dilator muscle. [2,9]
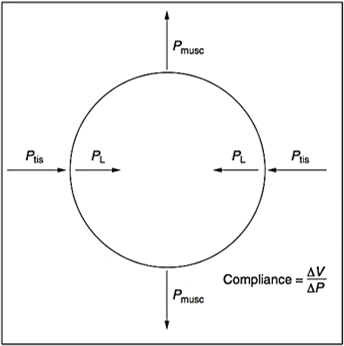
Figure 3: Upper airway caliber determinant. PL = intraluminal pressure; Ptis = tissue pressure around the pharyngeal wall; Pmusc = pressure exerted by the pharyngeal dilator muscles; V = change in volume; P = change in pressure [9]
The two main symptoms of respiratory distress during sleep are snoring and manifestations of drowsiness. [19] However, patients with snoring alone are poor predictors of OSA. Therefore, it must be correlated with other accompanying clinical features. Likewise, the absence of snoring does not rule out OSA. [9] Other symptoms that can be manifestations of OSA in adults and children are listed in Table 1. Symptoms and clinical features of findings in patients have a sensitivity and specificity of 60% in identifying OSA patients. [19]
| Adult | Children |
| The main symptoms | |
|
|
| Other symptoms | |
|
|
| Sign | |
|
|
Table 1: Symptoms and signs of sleep apnea in adults and children [19].
A number of investigative modalities have been used to approach the diagnosis of upper airway obstruction in patients with OSA, including examination; Muller's maneuvers, cephalometry, computed tomography (CT), magnetic resonance imaging (MRI), acoustic reflectometry, sleep video fluoroscopy (SVF), and DISE. [20] The gold standard examination for OSA is polysomnography. Polysomnography, first described in 1965 by Gastaut, is used to diagnose and assess the degree of sleep fragmentation and severity of OSA, but does not provide information regarding the degree and degree of airway collapse. [21,22] It is considered the reference standard for diagnosing OSA, but it is expensive and requires special resource. Polysomnography measures or estimates the Apnea-Hypopnea Indexs (AHI), a measure of the number of events of apnea or hypopnea per hour during sleep. AHI is used to diagnose and assess the severity of OSA. [23]
Apnea is defined as cessation of airflow in the nose and mouth for 10 seconds or more with arterial oxygen desaturation of 2% to 4%. Apnea is divided into central, obstructive or mixed. The difference between central and obstructive apnea is very important in determining the most appropriate treatment. [1,9] During obstructive apnea, the patient exhibits attempts at breathing without being able to ventilate due to upper airway obstruction, whereas central apnea occurs without any attempt at ventilation. Mixed apnea initially begins without ventilation effort (as a 'central' pattern), and ends as a barrier with resumption of ventilation efforts. Hypopnea is defined as a decrease in airflow for 10 seconds or more with a concomitant decrease in arterial oxygen saturation. The exact amount of desaturation for hypopnea varies in the literature. In clinical practice, it may not be necessary to distinguish apnea from hypopnea if the two have similar pathophysiological consequences. It is recommended to associate these two events in the form AHI. [9]
The AHI, also called the Respiratory Disturbance Index (RDI), refers to the total number of episodes of apnea and hypopnea per hour of sleep. It was calculated by dividing the total number of apnea / hypopnea during the recording period by the total sleep time. The American Academy of Sleep Medicine (AASM) sets a threshold of 15 events per hour with or without symptoms or 5 events per hour with symptoms for the diagnosis of OSA.23 OSA severity based on AHI is grouped into: [1,13,24]
- AHI <5: normal
- 5 <AHI <15: light
- 15 <AHI <30: moderate
- AHI ≥ 30: heavy
Because a broad spectrum of pharyngeal dysfunction is found in OSA, evaluation of the location of the obstruction and its severity in patients with OSA is very important in selecting the method of treatment. There are four treatment options for OSA, including continuous positive airway pressure (CPAP), oral devices, surgery, and lifestyle modification. [20] The standard treatment for OSA is positive upper airway pressure, usually given in a continuous mode, known as CPAP therapy. CPAP acts like a pneumatic splint that opens the upper airway, regardless of the location of the obstruction. [25,26] Because up to 50% of patients with OSA cannot tolerate CPAP, alternative treatments, such as upper airway stimulation, oral equipment (mandibular advancement device), and or surgery may be required. [27]
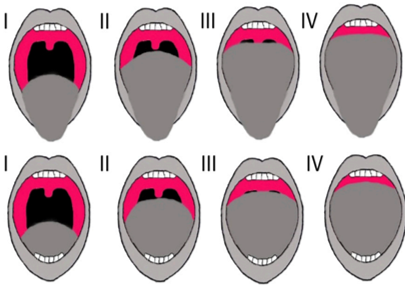
Surgical management was considered in patients with AHI> 15 events/hour and unable to tolerate or reject CPAP. [28] The most commonly performed surgical procedure to treat OSA is uvulopalato-pharyngoplasty (UPPP), but systematic reviews show UPPP success rate of only 45% in management. OSA. [29] Selection of preoperative patients who may respond to surgery is both a need and a priority. This requires a detailed assessment of the patient's anatomy. [11,30] An initial oropharyngeal anatomical evaluation to predict success in OSA patients is necessary. This method can separate patients who would benefit from UPPP alone from patients requiring multilevel surgical intervention. [11] The modified Mallampati (MM) and Friedman tongue position (FTP) clustering systems are the most commonly used systems (Figure 4). [11,30]
Friedman et al, [11] reported on the grading system (Table 2) and the significance of this grouping on the outcome of UPPP measures in OSA patients. The percentage of successful management of OSA with UPPP at stage 1 was 80.6%, stage 2 was 37.9%, and stage 3 was 8.1%
| Stage | FTP | Tonsil | BMI |
| 1 | I, II | 3 or 4 | <40 |
| 2 | I, II, III, atau IV | 0,1 or 2 or 3 or 4 | <40 |
| 3 | III atau IV | 0, 1 or 2 | <40 |
| 4* | I-IV | 0-4 | >40 |
| * All patients with significant craniofacial or anatomical abnormalities. | |||
Table 2: Friedman staging system based on FTP, tonsils, and BMI [11].
Conclusion
Identifying the pattern and pathophysiology of airway obstruction in OSA is essential. The gold standard examination for OSA is polysomnography. An initial oropharyngeal anatomical evaluation to predict success management of OSA patients is necessary.
References
- Sarber KM, Lam DJ, Ishman SL. (2021). Sleep Apnea and Sleep Disorders. In: Flint PW, Francis HW, Haughey BH, eds. Cummings Otolaryngology - Head And Neck Surgery. 7th ed. Elsevier Inc 215-235.
- Rachmawati EZK, Arief W, Tamin S, Yunizaf R, Fardizza F. (2018). Patogenesis dan diagnosis gangguan napas saat tidur dengan Drug Induce Sleep Endoscopy (DISE). Oto Rhino Laryngol Indones. 47(2): 193-203.
- Korson R, Guilleminault C. (2017). Sleep Disorders Medicine. In: Chokroverty S, ed. Sleep Disorders Medicine. 4th ed. Springer 567-596.
- Kamasová M, Václavík J, Kociánová E, Táborský M. (2018). Obstructive sleep apnea in outpatient care – What to do with? Cor Vasa. 60(3): e274-80.
- Franklin KA, Lindberg E. (2015). Obstructive sleep apnea is a common disorder in the population-A review on the epidemiology of sleep apnea. J Thorac Dis. 7(8): 1311-1322.
- Semelka M, Wilson J, Floyd R. (2016). Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Am Fam Physician. 94(5): 355-361.
- Kapur VK, Auckley DH, Chowdhuri S, et al. (2017). Clinical practice guideline OSA american academy. J Clin Sleep Med. 13(3): 479-504.
- Laratta CR, Ayas NT, Povitz M, Pendharkar SR. (2017). Diagnosis and treatment of obstructive sleep apnea in adults. Cmaj. 189(48): E1481-88.
- Aghoutan H, Alami S, Diouny S, Bourzgui F. (2015). Orthodontic Considerations in Obstructive Sleep Apnea — State of the Art. In: Motamedi MH, ed. A Textbook of Advanced Oral and Maxillofacial Surgery Volume 2. IntechOpen Limited 361-391. doi:10.5772/59086
- Dumitrescu N, Sarafoleanu C. (2018). Drug-induced sleep endoscopy – decisional factor in obstructive sleep apnea treatment. Rom J Rhinol. 8(30): 77-85.
- Friedman M, Salapatas AM, Bonzelaar LB. (2017). Updated Friedman Staging System for Obstructive Sleep Apnea. Adv Otorhinolaryngol. 80: 41-48.
- Kezirian EJ, Weaver EM. (2014). Hypopharyngeal and Skeltal surgery for OSA. In: Johnson JT, Rosen CA, eds. Bailey ’s Head and Neck Surgery Otolaryngology. Vol 2. 5th ed. Lippincott Williams&. Wilkins 2206-2219.
- Patel SR. (2019). Obstructive sleep apnea. Ann Intern Med. 171(11): ITC81-96.
- Osman AM, Carter SG, Carberry JC, Eckert DJ. (2018). Obstructive sleep apnea: current perspectives. Nat Sci Sleep. 10:21-34.
- Alsubie HS, BaHammam AS. (2017). Obstructive Sleep Apnoea: Children are not little Adults. Paediatr Respir Rev. 21: 72-79.
- Gottlieb DJ, Punjabi NM. (2020). Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA - J Am Med Assoc. 323(14): 1380-1400.
- Chan KC, Au CT, Hui LL, Ng S kwan, Wing YK, Li AM. (2019). How OSA Evolves From Childhood to Young Adulthood: Natural History From a 10-Year Follow-up Study. Chest. 156(1): 120-130.
- Bue A Lo, Salvaggio A, Insalaco G. (2020). Obstructive sleep apnea in developmental age . A narrative review International Classification of Sleep Disorders. Eur J Pediatr. 179(3): 357-365.
- Woodson BT, Boonwan A, Phillips JM. (2016). Sleep Medicine and Surgery. In: Wackym PA, Snow JB, eds. Ballenger’s Otorhinolaryngology Head and Neck Surgery 18. 18th ed. PMPH-USA; 1279-1294.
- Kim JY, Han SC, Lim HJ, Kim HJ, Kim JW, Rhee CS. (2020). Drug-induced sleep endoscopy: A guide for treatment selection. Sleep Med Res. 11(1): 1-6.
- Yegïn Y, Çelik M, Kaya KH, Koç AK, Kayhan FT. (2017). Comparison of drug-induced sleep endoscopy and Müller’s maneuver in diagnosing obstructive sleep apnea using the VOTE classification system. Braz J Otorhinolaryngol. 83(4): 445-450.
- Balu R, Mol VKS, Menon UK. (2019). Usefulness of Drug-induced Sleep Endoscopy to Diagnose Laryngeal Cause in Obstructive Sleep Apnea Patients. Int J Phonosurgery Laryngol. 9(2): 40-42. doi:10.5005/jp-journals-10023-1174
- Qaseem A, Dallas P, Owens DK, Starkey M, Holty JEC, Shekelle P. (2014). Diagnosis of obstructive sleep apnea in adults: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 161(3): 210-220.
- Parajuli BD, Mandal L, Koirala M, Bhattarai AS, Neupane Y, Shrestha A. (2019). Drug Induced Sleep Endoscopy for Obstructive Sleep Apnea Syndrome: An Initial Experience in a Tertiary Level Centre. JIOM Nepal. 41(3): 83-85.
- Blumen M, Bequignon E, Chabolle F. (2017). Drug-induced sleep endoscopy: A new gold standard for evaluating OSAS? Part I: Technique. Eur Ann Otorhinolaryngol Head Neck Dis. 134(2): 101-107.
- Carrasco-Llatas M, Matarredona-Quiles S, De Vito A, Chong KB, Vicini C. (2019). Drug-Induced Sleep Endoscopy: Technique, Indications, Tips and Pitfalls. Healthcare. 7(3): 93-102.
- Charakorn N, Kezirian EJ. (2016). Drug-Induced Sleep Endoscopy. Otolaryngol Clin North Am. 49(6): 1359-1372.
- Thuler E, dos Santos Junior V, Sayuri Yui M, Tominaga Q, Rabelo FAW. (2020). Correlation between drug-induced sleep endoscopy criteria for patient selection and transoral robotic surgery outcomes in obstructive sleep apnea treatment. Aust J Otolaryngol. 3(June): 20-20.
- He M, Yin G, Zhan S, et al. (2019). Long-term Efficacy of Uvulopalatopharyngoplasty among Adult Patients with Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. Otolaryngol - Head Neck Surg (United States). 161(3): 401-411.
- Yu JL, Rosen I. (2020). Utility of the modified Mallampati grade and Friedman tongue position in the assessment of obstructive sleep apnea. J Clin Sleep Med. 16(2): 303-308.
Citation: Yayan Akhyar and Novialdi. (2021). Obstructive Sleep Apnea (OSA) as a Cause of Sleep Disorders. Journal of Otolaryngology - Head and Neck Diseases 3(1).
Copyright: © 2021 Yayan Akhyar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.