Case Report
Volume 2 Issue 1 - 2020
Management of Concurrent Tracheo-esophageal Perforation
1Department of Otolaryngology – Head and Neck Surgery. Virginia Commonwealth University School of Medicine. Richmond, Virginia.
2Department of Otolaryngology – Head and Neck Surgery. Augusta University. Augusta, GA.
2Department of Otolaryngology – Head and Neck Surgery. Augusta University. Augusta, GA.
*Corresponding Author: Thomas S. Lee, MD, FACS, Associate Professor Division Chief of Facial Reconstructive & Trauma surgery Head & Neck Cancer Surgery Skull Base Surgery Department of Otolaryngology Virginia Commonwealth University.
Received: July 22, 2020; Published: August 01, 2020
Abstract
Anterior cervical discectomy and fusion surgery is a common and well described surgical procedure, with a well documented risk and complication profile. Here we present a case report of a patient with a concurrent tracheal and esophageal perforation in the setting of ACDF surgery. Our patient developed these complications secondary to hardware failure and underlying cervical osteomyelitis. We hope to not only increase awareness about an uncommon, potentially fatal, complication associated with ACDF surgery but also outline our management algorithm. Our particular patient underwent an initial surgery for tracheal perforation repair, involving the use of a locoregional flap which is outlined in detail. The patient subsequently underwent a second surgery for identification and repair of an underlying esophageal perforation, which utilized a pedicled muscle flap for surgical repair. Here we describe our perioperative management and surgical technique in managing complex complications arising in the setting of anterior cervical discectomy and fusion surgery.
Keywords: Trachea; Esophagus; Foreign body; Reconstruction
Introduction
Anterior cervical discectomy and fusion (ACDF) is a surgery which involves removal of a herniated or degenerated disc in the neck. The surgery involves removal of a vertebral disc with insertion of a bone graft which is fused to the surrounding vertebrae with metal plates and screws. ACDF surgery is typically employed for patients with degenerative, neoplastic, infective and traumatic cervical spine pathology. [1]
Complications associated with the surgery include hardware failure, esophagopharyngeal trauma, cranial nerve injury, mediastinitis, and pulmonary complications. [2] The reported incidence of hardware failure associated with ACDF surgery ranges from 5-35%. [3] Hardware failure typically includes screw loosening, screw breakage, plate breakage, or component migration. The concern with hardware failure is often subsequent esophageal, pharyngeal or tracheal injury.
Esophageal injury is a well documented complication associated with ACDF surgery secondary to retraction, instrumentation, and hardware failure/migration. The esophagus has been found to be the most common site of screw migration in hardware failure, with many reports of esophageal injury and perforation. [4, 5] The correlation with esophageal injury is likely related to close anatomic proximity of the esophagus and the cervical spine. Case reports have also been published showing delayed esophageal injury up to 9 years following ACDF surgery, usually secondary to hardware erosion. [6-7]
Airway complications secondary to ACDF surgery are considered to be extremely rare. They are typically thought to be related to acute pharyngeal edema from surgical manipulation, and almost never related to surgical hardware implantation. Wong et. al described a case of hardware dislodgement in an ACDF patient leading to prevertebral abscess formation and subsequent upper airway obstruction; however, this is an exceedingly rare occurrence. [3, 8-9]
Complications related to ACDF surgery are well documented in the literature. Here we present an exceeding rare case of a patient developing concurrent tracheo-esophageal perforation following ACDF surgery. Additionally, we outline our algorithm for the management and operative technique of this unique clinical entity.
Case Report
A 34-year-old woman presented to our institution with sepsis, recurrent epidural abscess, urinary tract infection, and systemic end organ failure. Six months prior she had had undergone anterior cervical discectomy and fusion (ACDF) with bony cage and plate placement from C4 to C7 following evacuation of a cervical abscess at outside hospital. Upon admission she was started on broad spectrum intravenous antibiotics and monitored closely.
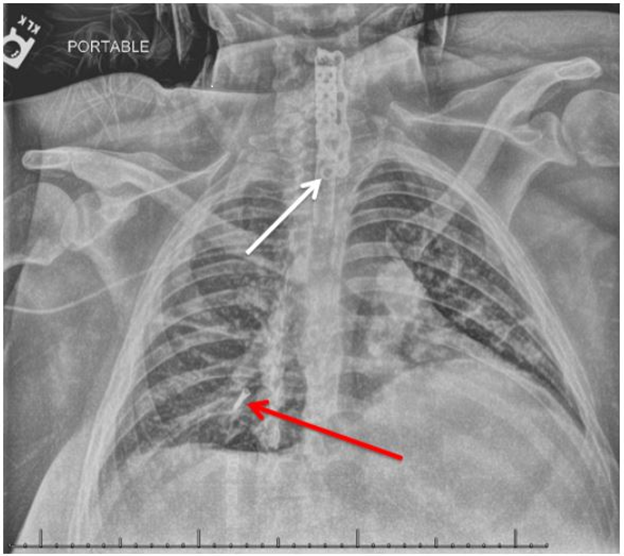
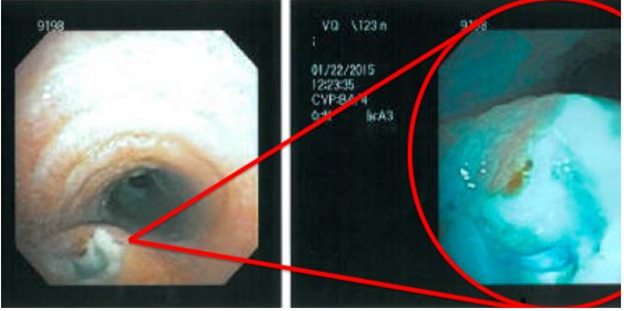
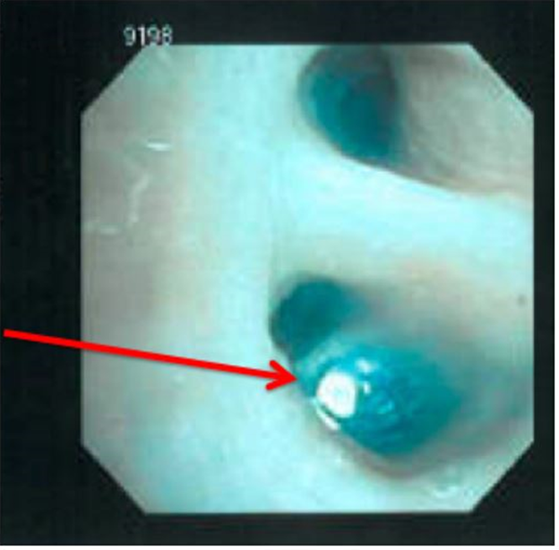
Nearly two months following admission she underwent a routine chest x-ray and was found to have metallic density at the right lung base. Additional imaging revealed a dislodged screw from an ACDF plate that had migrated through the trachea and settled in the posterior aspect of the right lower lobe. (Figure 1) An esophagram was obtained prior to surgical intervention of the tracheal injury which showed no evidence of esophageal perforation at the time. She later underwent a multi-disciplinary operative intervention involving spine surgery, interventional pulmonology and otolaryngology teams. During the surgery she underwent intubation with a flexible bronchoscope which demonstrated a tracheal defect in the posterolateral wall of the trachea with visible migrated spine hardware. (Figure 2). The screw was retrieved with a flexible bronchoscope by the interventional pulmonology team, following establishment of a secure airway. (Figure 3) The patient then underwent a left neck exploration by the otolaryngology and spine surgery teams. The exploration was performed medial to the carotid artery and lateral to the larynx. During the dissection we encountered grossly infected granulation tissue in the prevertebral space. The infected tissue was debrided, and the cervical hardware and bone graft cage were removed. She was ultimately left with a large vertebral body defect.
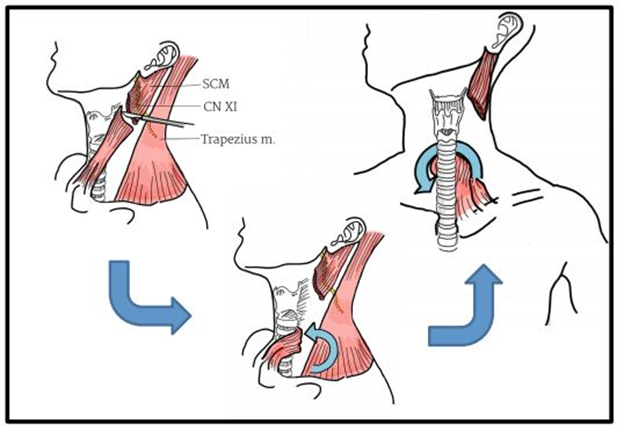
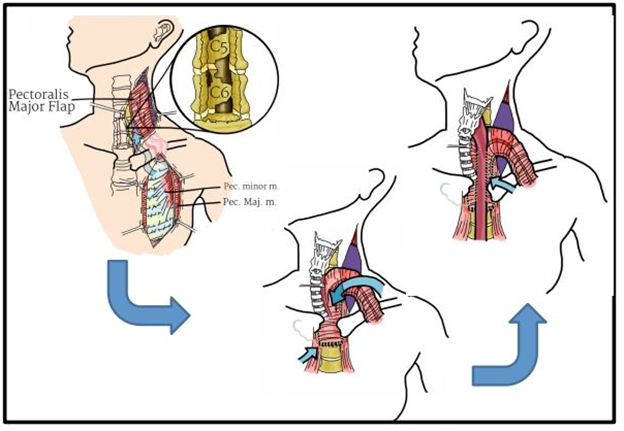
To address the tracheal perforation, we first ensured that the endotracheal cuff was located distal to the site of tracheal injury hoping to minimize pressure being applied on the repair. The tracheal defect was identified and repaired in a primary fashion. We utilized an inferiorly based sternocleidomastoid (SCM) flap to further reinforce the defect. (Figure 4) Additionally, at the time of surgery the spine surgery team applied a halo with cervical collar to provide stabilization until a delayed reconstruction could be performed. One week following the original surgery she underwent posterior cervical fusion and halo removal. Flexible bronchoscopy at the time of the second surgery showed a well healed tracheal defect, and the patient was extubated successfully.
Several days following the posterior cervical fusion the patient began endorsing dysphagia. A modified gastrografin swallow study was obtained which showed a posterior esophageal perforation at the level of the C5-6 vertebral bodies. (Figure 5) Conservative measures were initially employed, but a repeat esophagram 10 day later showed persistence of the esophageal leak and the decision was made to proceed with operative repair. Esophagoscopy at the time of surgery showed a small circular defect in the upper esophagus past the introitus. Neck exploration was again employed to identify and repair the defect at hand. During the dissection we identified the esophagus and found it to be scarred to a large vertebral bony defect where the cage had previously been. It appeared that the bony ledge of the vertebral defect had eroded into the esophagus. We ultimately decided to dissect free the esophagus, and drill down the vertebral body defect to ensure further complications would not ensue. Due to the size of the vertebral body bony defect and the degree of osteomyelitis present, we elected to place a pedicled myofascial flap in between the esophagus and the bony defect. The esophageal defect was primary closed, and a pedicled pectoralis flap was used to reinforce the esophageal perforation site. (Figure 6) Postop the patient progressed appropriately, a postop swallow study showed no further evidence of leak and the patient was discharged home.
Discussion
ACDF surgery is generally regarding as a safe surgical intervention with a low morbidity. Airway related complications postoperatively are exceedingly rare in ACDF surgery. Airway complications when they do occur are secondary to pharyngeal edema, hematoma formation, cerebrospinal fluid leak, angioedema, or abscess formation. [4, 8] To our knowledge this is the first report of airway compromise secondary to tracheal perforation. Risk factors for postoperative airway complications include prolonged operative time, surgery that exposed three or more vertebral levels, or operating at C4 or higher. [8, 9] Patients undergoing surgery in the upper cervical spine are at the highest risk for postoperative edema and careful airway observation is recommend in this patient population. [9]
Tracheobronchial injuries occur for many reasons including blunt or penetrating trauma, foreign body aspiration, toxic inhalation, or post procedure (tracheotomy, bronchoscopy, tracheal intubation). The mechanism of injury is thought to be pressure or contact against the posterior tracheal wall which lacks cartilage. [10] Patients with tracheal injuries often present with difficulty breathing, blood in the sputum, subcutaneous emphysema in the neck or chest, insufficient oxygenation, sternal discomfort, and penumomediastinum. [10] Tracheal injury management often varies based on location and severity of injury, but often includes some form of tracheal stenting, primary closure, or locoregional flap reconstruction. [11] In our practice, we tend to avoid tracheal stenting as it often causes significant granulation tissue formation within the tracheal lumen, and so we reserve it for more select circumstances. Our preference for tracheal injury repair is primary closure with the addition of a vascularized locoregional muscle flap. Additionally, we prefer either delayed extubation (~7 days) or tracheostomy placement in this patient population. Locoregional flap options for tracheal repair include sternohyoid or Sternocleidomastoid (SCM) flaps. Our preference is the SCM flap due to its pliability and versatility, the flap pedicle can be based superiorly or inferiorly depending on defect location. The flap has a reliable blood supply which aids in wound healing at the site of repair. This particular flap is associated with a low donor-site morbidity. Additionally, in the setting of ACDF in which patients may be in cervical collars to stabilize the neck, there isn’t significant concern of flap compression as would be the case for other reconstructive options.
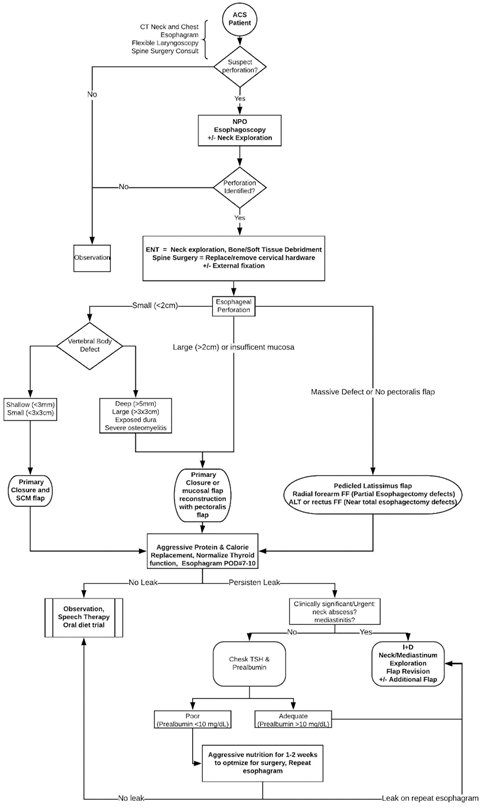
Esophageal injury secondary to ACDF surgery is a well-documented and understood complication. However, here we presented a patient with a delayed esophageal perforation secondary to esophageal erosion from a large vertebral body defect. This case further supports the need for prophylactic protection of the esophagus is high risk surgical patients. [2] We had assessed both preoperative and intraoperatively for an esophageal injury at the time of the initial surgery and no defect was identified. At the time of the second surgery we identified sharp bony edges associated with the vertebral body defect that we believe contributed to the injury. As a result of this case we have modified our treatment algorithm to utilize thicker muscle flaps for additional protection. We utilize the pectoralis muscle flap in this case to provide significant bulk and adequate coverage of the vertebral body defect. In instances of large esophageal perforations (>2cm), large vertebral body defects (deeper than 5mm or large than 5cm in length), or persistent defect despite intervention the pectoralis muscle flap provides a versatile alternative. It is extremely important in these instances to fill any evident dead space, as it can lead to poor tissue healing or a chronically infected wound. Additionally, of note anytime a pectoralis muscle flap is utilized for head and neck reconstruction and the patient needs a cervical collar, it is important to modify the collar as to not strangulate the blood supply as it transverses over the clavicle into the neck. Previous studies have suggested algorithms for the management of esophageal perforations; however, to our knowledge there is no standardized protocol. [6, 12-16] Here we present our treatment algorithm for esophageal defects in the setting of ACDF surgery. (Figure 7)
Conclusion
Here we present a unique case of a concurrent tracheo-esophageal perforation in patient with multiple complications following ACDF surgery. Additionally, here we highlight the importance of a multidisciplinary approach when treating a complicated patient population. We hope to add to the current body of literature and provide additional evidence to support our outlined treatment algorithm. With ACDF surgery like any other procedure it is important to discuss possible complications including prevertebral abscess, cervical osteomyelitis, hardware migration, and tracheo-esophageal perforation. Otolaryngologist may be asked to aid the treatment of these complicated patients, as they often developed chronically infected neck wounds and have grossly distorted cervical soft tissue anatomy. Primary focus should always be on securing a stable airway in this patient population, in our case we had performed a primary tracheal repair reinforced with a locoregional muscle flap. Our patient subsequently developed a delayed esophageal perforation, and we have outlined our treatment algorithm to increase awareness and provide surgical alternatives.
References
- Pompili A, Canitano S, Caroli F, Caterino M, Crecco M, Raus L, Occhipinti E. (2002). Asymptomatic esophageal perforation caused by late screw migration after anterior cervical plating: report of a case and review of relevant literature. Spine (Phila Pa 1976). Dec 1; 27(23): E499-502. Review.
- Capen DA, Garland DE, Waters RL. (1985). Surgical stabilization of the cervical spine. A comparative analysis of anterior and posterior spine fusions. Clin Orthop Relat Res. Jun;(196): 229-37.
- Wong DT, Fehlings MG, Massicotte EM. (2005). Anterior cervical screw extrusion leading to acute upper airway obstruction: case report. Spine (Phila Pa 1976). Nov 15; 30(22): E683-6.
- Salis G, Pittore B, Balata G, Bozzo C. (2013). A rare case of hypopharyngeal screw migration after spine stabilization with plating. Case Rep Otolaryngol. 2013: 475285.
- Sahjpaul RL. (2007). Esophageal perforation from anterior cervical screw migration. Surg Neurol. Aug; 68(2): 205-9.
- Rueth N, Shaw D, Groth S, Stranberg S, D'Cunha J, Sembrano J, Maddaus M, Andrade R. (2010). Management of cervical esophageal injury after spinal surgery. Ann Thorac Surg. Oct; 90(4): 1128-33.
- Lu DC, Theodore P, Korn WM, Chou D. (2008). Esophageal erosion 9 years after anterior cervical plate implantation. Surg Neurol. Mar; 69(3): 310-2; discussion 312-3.
- Sagi HC, Beutler W, Carroll E, Connolly PJ. (2002). Airway complications associated with surgery on the anterior cervical spine. Spine (Phila Pa 1976). May 1; 27(9): 949-53.
- Andrew SA, Sidhu KS. (2007). Airway changes after anterior cervical discectomy and fusion. J Spinal Disord Tech. Dec; 20(8): 577-81.
- Austin RD. Thoracotomy for tracheal disruption after traumatic intubation: a case report. AANA J. 2010 Oct; 78(5): 400-4.
- Ch'ng S, Wong GL, Clark JR. (2013). Reconstruction of the trachea. J Reconstr Microsurg. 2014 Mar; 30(3): 153-62.
- Kuppusamy MK, Hubka M, Felisky CD, Carrott P, Kline EM, Koehler RP, Low DE. (2011). Evolving management strategies in esophageal perforation: surgeons using nonoperative techniques to improve outcomes. J Am Coll Surg. Jul; 213(1):164-71; discussion 171-2.
- Jiang J, Yu T, Zhang YF, Li JY, Yang L. (2012). Treatment of cervical esophageal perforation caused by foreign bodies. Dis Esophagus. Sep- Oct; 25(7): 590-4.
- Wierzbicka M, Bartochowska A, Banaszewski J, Szyfter W. (2013). Cervical oesophageal and hypopharyngeal perforations after anterior cervical spine surgery salvaged with regional and free flaps. Neurol Neurochir Pol. Jan-Feb; 47(1): 43-8.
- Anandaswamy TC, Pujari VS, Shivanna S, Manjunath A. (2012). Delayed pharyngoesophageal perforation following anterior cervical spine surgery: An incidental finding. J Anaesthesiol Clin Pharmacol. Jan;28(1):139- 40.
- Fujioka M, Oka K, Kitamura R, Yakabe A. (2009). Cervical osteomyelitis and epidural abscess treated with a pectoralis major muscle flap. Surg Neurol. Dec; 72(6):761-4; discussion 764.
Citation: Nima Vahidi, Luke W. Edelmayer, Aasif Kazi, Thomas S. Lee. (2020). Management of Concurrent Tracheo-esophageal Perforation. Journal of Otolaryngology - Head and Neck Diseases 2(1). DOI: 10.5281/zenodo.3977829
Copyright: © 2020 Thomas S. Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.