Research Article
Volume 4 Issue 1 - 2023
Intramedullary Fixation of the Pubis in Unstable Pelvis
Universidad Católica Argentina, Facultad de Medicina, Av. Alicia Moreau de Justo 1500, PC1107 Ciudad Autónoma de Buenos Aires, Argentina
Hospital General de Agudos Juan A. Fernández, Cerviño 3356, PC 1425, Ciudad Autónoma de Buenos Aires, Argentina
Hospital General de Agudos Juan A. Fernández, Cerviño 3356, PC 1425, Ciudad Autónoma de Buenos Aires, Argentina
*Corresponding Author: Ana L. Douglas Price, Adress: Cerviño 3356, third floor, PC 1425, Ciudad Autónoma de Buenos Aires, Argentina.
Received: January 15, 2023; Published: January 26, 2023
Abstract
Introduction: Fractures and injuries to the pelvic ring account for 2-8% of all fractures, but in the presence of polytrauma it amounts to 20-25% of cases.
The patient with pelvic trauma and pelvic instability requires multidisciplinary treatment, consisting of orthopedic surgeons, general surgeons, emergency physician, and interventional radiologists.
The aim of this work is to describe the technical steps of trans-symphysial fixation of the pubic symphysis, to avoid complications of the procedure and reduce the incidence of fixation failures.
Surgical Technique: We describe de Surgical Technique for pubic symphysis diastasis with two screws.
Discussion: In pelvic trauma, many treatments have been reported on restoration of the anatomy of pubic symphysis, the appropriate strategy remains controversial.
At our institution, we recommend percutaneous trans symphyseal fixation surgery in cases of Young and Burgess grade II and III instability, given the mechanical and hemodynamic instability they generate. This is associated with posterior sacroiliac instabillity, to obtain fixation of the posterior ring, also with percutaneous technique and by means of a 6.5 mm iliosacral screw.
Conclusion: Fixation of symphysis with a crossed screw, between both pubic bones, is usually sufficient to stabilize the unstable pelvis
Keywords: Young and Burgess grade II and III; hemodynamic instability; Symphysis diastasis; Trans-symphysial fixation, pubic symphysis
Introduction
Fractures and injuries to the pelvic ring account for 2-8% of all fractures, but in the presence of polytrauma it amounts to 20-25% of cases. [1, 2]
Pelvic injuries occur when an excessive force is applied to the human body, and for this reason other extrapelvic injuries are often added to polytrauma, which can usually cause bleeding (chest 15%, intra-abdominal 32%, long bones 40%) and compromise the hemodynamic status of the patient. [3]
Wang et al. have published, in a study of 1566 patients with pelvic trauma, that the total mortality rate was 9.96% and 74% of the patients died in the first 24 hours, secondary to massive bleeding. [4] In patients with associated pelvic fracture and hemodynamic instability, a mortality of 40% has been reported. [5]
The patient with pelvic trauma and pelvic instability requires multidisciplinary treatment, consisting of orthopedic surgeons, general surgeons, emergency physician, and interventional radiologists. This comprehensive treatment and in a single treatment institution, optimizes the result for the control of the patient's bleeding. [6-9]
The orthopedic surgeon who belongs to the multidisciplinary treatment team must acquire the necessary skills to be able to perform pelvic fixation procedures quickly and effectively to reduce the risk of death of the polytraumatized patient.
Pubic trans-symphysial fixation is complex to perform and requires multiple tips to carry it out efficiently, due to this, this paper describes the indications for the procedure, patient selection and surgical technique to achieve adequate bone fixation of the pubis symphysis.
Once hemodynamic stabilization has been achieved, the treatment performed at our institution for Anterior Posterior Compression (APC) injuries with an opening greater than 2.5 cm is percutaneous fixation of the sacroiliac joint in supine position and anterior closure of the pelvic ring. It is carried out, by performing a pubic trans-symphysial fixation, by means of one or two percutaneous screws.
The aim of this work is to describe the technical steps of trans-symphysial fixation of the pubic symphysis, to avoid complications of the procedure and reduce the incidence of fixation failures.
Surgical Technique
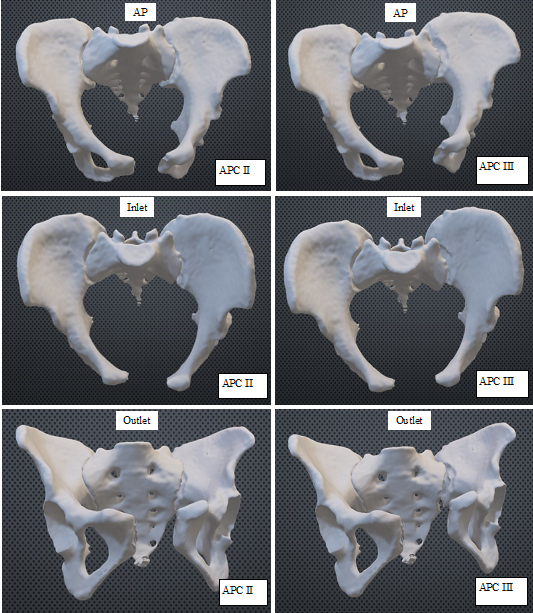
Selection of the patient to treat: Young and Burgess grade II and III Figure 1
Selection of the patient to treat: Young and Burgess grade II and III Figure 1
Contraindication: Obese patient. Osteoporosis of the pubis
Corridors Description
First Corridor: The entry point is at the pubic tubercle. The direction is from superior to inferior, lateral to medial with angulation of 25 to 35 degree with respect de pubic bone. The exit orifice is in the contralateral pubis, on the inner edge of the obturator foramen, but the cortex should not go through more than 2 mm to avoid neurovascular damage. The diameter of the screw must be determined by the anteroposterior width of the pubic bone.
Second corridor: The entry point of the corridor is 1,5 cm below the pubic tubercle and two centimeters lateral to the pubic symphysis. The direction of the corridor is from lateral to medial with a slight inclination from anterior to posterior, toward the contralateral pubis This corridor does not have an exit hole since the tip of the screw ends up in the body of the contralateral pubis. The diameter of the screw is 4mm and the length is approximately 45mm.
Patient position: Patient must be placed in the radiolucent surgical table in supine position on a pad 5 centimeters high, giving hip extension to allow the correct instrument position. Urinary catheter must be placed so the bladder is empty an avoid injuries to it.
Radiological control of the reduction of the pubic symphysis: The pubic symphysis joint must be clearly observed through the C-arm, in AP position, inlet and outlet view, to visualize the reduction of the symphysis joint. Must check that all views before starting the surgery.
Reduction of pelvic displacement: To complete the reduction of the diastasis, must done external manual pressure of both iliac bones. If the reduction in the C-Arm is confirmed in the three positions mentioned above, we proceed to percutaneous fixation using the cross screw.
If the desired reduction is not achieved, two Schanz screws are placed intramedullary in both iliac crests, the anterior in the proximal third of the iliac crest and the posterior in the posterior third of the iliac crest. This location of the Schanz, facilitates the reduction of the pubic symphysis in the three planes of space, by compressing the iliac crests with those nails as a joystick, making sure the exact reduction at pubic junction, by checking the bilateral symmetry of the hemipelvis at superficial and deep pelvic ring. The posterior sacroiliac joint is closed by percutaneous screws using 6,5mm canulated screw either 16 or 32.
First corridor Screw
At this point in the surgical technique, we must perform the first damage control maneuver, which consists of manually detecting the external inguinal ring, to avoid inadvertent injury by the surgeon when the first k-wire is placed. Figure 2
At this point in the surgical technique, we must perform the first damage control maneuver, which consists of manually detecting the external inguinal ring, to avoid inadvertent injury by the surgeon when the first k-wire is placed. Figure 2
The index finger is inserted through the scrotal sac up to find the inguinal ring, which is an anatomical structure in the anterior wall of the abdomen that houses the ilioinguinal nerve, the genital branch of the Genito femoral nerve, and the spermatic cord (in the male) or the round ligament (in the female).
Placing the K-wire
Once the inguinal ring entry point is identified, the K-wire entry point is medial to the pubic tubercle, the procedure must be done under fluoroscopy in the three views. The outlet view gives the exact frontal orientation in the pubic body, the direction of the nail inside the body of the pubic bone. The inlet view allows us to observe the anterior and posterior cortex of the symphysis and avoid damaging the urinary bladder. Figure 3
Once the inguinal ring entry point is identified, the K-wire entry point is medial to the pubic tubercle, the procedure must be done under fluoroscopy in the three views. The outlet view gives the exact frontal orientation in the pubic body, the direction of the nail inside the body of the pubic bone. The inlet view allows us to observe the anterior and posterior cortex of the symphysis and avoid damaging the urinary bladder. Figure 3
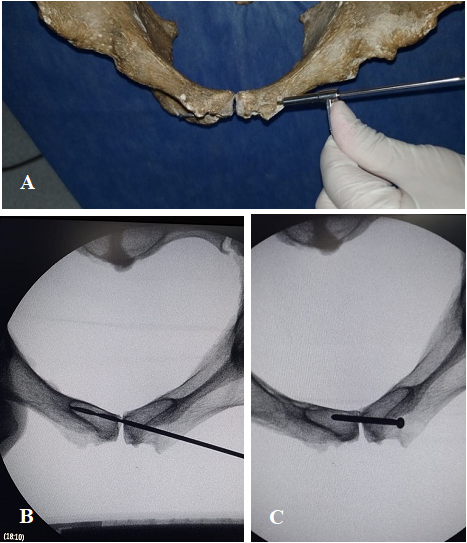
Figure 3: Inlet view to identify anterior and posterior aspects of symphysis and avoid damaging the urinary bladder. A, Entry point on pelvic bone model. B, Drilling first corridor. C, Screw position on inlet view.
Skin incision
Once the entry point for the placement of the K-wire is located, a 1.5 cm incision is made at said anatomical point, to avoid skin damage in the placement of the fixation screw.
Once the entry point for the placement of the K-wire is located, a 1.5 cm incision is made at said anatomical point, to avoid skin damage in the placement of the fixation screw.
Kirschner Pin Placement
A 3.2mm guidewire is inserted angled at 25 degrees from superior to inferior at pubic tubercule and pointing to the inferior end of the contralateral pubis. Percutaneous drilling is continued under constant fluoroscopy control. At the exit point, once the canal has been prepared, we prefer to use a 4.5mm cannulated cortical screw or a 4 mm cannulated cancellous bone screw, our preference is to use a single screw. Figure 4
A 3.2mm guidewire is inserted angled at 25 degrees from superior to inferior at pubic tubercule and pointing to the inferior end of the contralateral pubis. Percutaneous drilling is continued under constant fluoroscopy control. At the exit point, once the canal has been prepared, we prefer to use a 4.5mm cannulated cortical screw or a 4 mm cannulated cancellous bone screw, our preference is to use a single screw. Figure 4
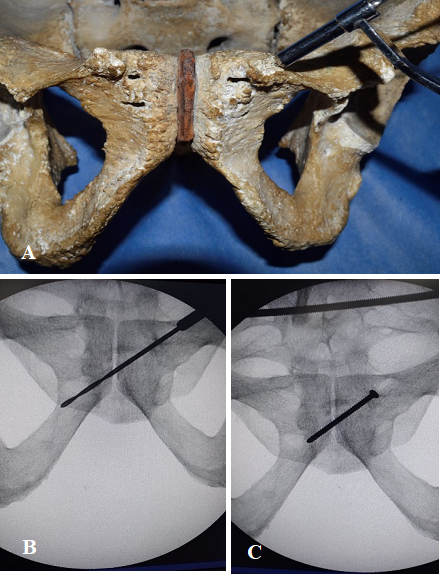
Figure 4: Outlet view to determine top to bottom direction on symphysis. A, Entry point on pelvic bone model. B, Drilling first corridor. C, Screw position on outlet view.
It is very important to avoid repeated drilling so as not to damage the spongy pubic bone that allows screw fixation and can create a large hematoma in a closed space which ends up in the scrotum sac as has been seen in a few patients.
The placement of the second screw in the pubis is controversial, due to the following reasons.
- The pubis is a small anatomical structure, especially in women, and the first screw placed in the first corridor often makes it difficult to access the second corridor.
- Anatomically, in males, the inguinal canal contains the spermatic cord, which includes the vas deferens, the testicular artery, and the genital branch of the genitofemoral nerve, from the pelvic cavity to the scrotum; in females, the inguinal canal transmits the round ligament of the uterus and the ilioinguinal nerve to the labia majora. These structures are in danger with this technique. [10]
- The distal exit of the screw, is risky in the obturator foramen with the possibility of damage to the obturator canal and the obturator’s neurovascular bundle (where the vein, artery and obturator nerve are located)
The listed problems can be solved doing a preoperative planning to see the feasibility of placing the second screw. When the second screw is introduced, it must reach the distal cortex, without going through it. Figure 5 Requires a preoperative CT scan to assess possible space for the second corridor. When choosing the site of introduction, the situation of the spermatic cord or round ligament must be verified with the ultrasound, to avoid damage to the anatomical structures. The placement of the screw should preferably be carried out by three-dimensional navigation, to pass through the second corridor without problems and do not cross the second bone cortex. Figure 6 Finally, when the second screw is inserted, the obturator canal must be controlled with the ultrasound to avoid injury the obturator neurovascular bundle.
Discussion
In pelvic trauma, pubic symphysis diastasis is typically associated with a high-energy mechanism of injury. [11] Although many treatments have been reported on restoration of the anatomy of pubic symphysis, the appropriate strategy remains controversial. [12]
Pubic symphysis diastasis is often a result of anterior-posterior compression injury based on the Young and Burgess Classification system. The injuries are classified into three types, i.e., APC-I (slight widening of pubic symphysis or anterior sacroiliac joint, or both); APC-II (widened anterior sacroiliac joint >2.5 cm, disrupted anterior sacroiliac, Sacro tuberous, and sacrospinous ligaments, intact posterior sacroiliac ligaments); and APC-III (complete sacroiliac joint disruption with lateral displacement, disrupted anterior sacroiliac, sacrotuberous, and disrupted posterior sacroiliac ligaments). [13, 14]
Antero-posterior compression injuries type II and III are rotationally unstable and combined (rotational and vertical instability) respectively. Open reduction and internal fixation using plate and screw system has been widely accepted as the standard treatment. [15, 16]
However, the technique needs extensive exposure of the pubic symphysis, resulting in more complications, such as blood loss, neural and vascular injuries, wound problems, and heterotopic bone formation. [17]
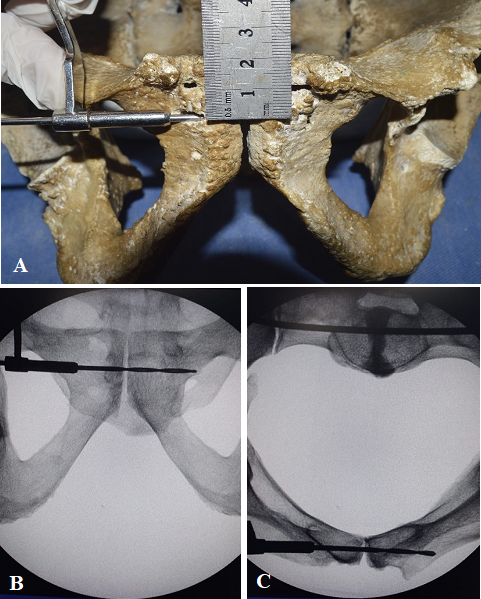
Figure 5: Second corridor A, Entry point on pelvic bone model. B, Outlet view and C, Inlet view. Drill and screw must avoid going through distal cortex.
At our institution, we recommend percutaneous trans symphyseal fixation surgery in cases of Young and Burgess grade II and III instability, given the mechanical and hemodynamic instability they generate. This is associated with posterior sacroiliac fixation, to obtain fixation of the posterior ring, also with percutaneous technique and by means of a 6.5 mm iliosacral screw.
The polytraumatized pelvic patient requires comprehensive treatment, performed by a multidisciplinary team of specialists, because hemodynamic instability at the time of admission or in its early evolution, can lead to patient death. [18-20]
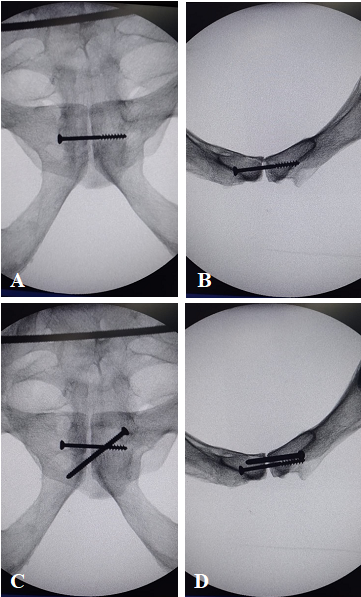
Figure 6: A, Outlet and B, inlet view, screw placed on second corridor. C and D, Outlet and Inlet views of cross crews placed on both corridors.
It has been reported that the mortality in pelvic polytraumatized patients, who present hemodynamic instability, reaches 30 or 40% of them. [21]
Management of hemodynamic instability is carried out according to the guidelines proposed by the American College of Surgeons Advanced Trauma Life Support (ATLS). [22]
The ATLS guidelines recommend using a sheet, or a pelvic binder applied at the level of the greater trochanters of the femur to produce sufficient temporary fixation for the unstable pelvis to control intrapelvic bleeding, especially in prehospital phase. [22]
In our Trauma center, we perform the placement of the C-clamp, in order to stabilize the pelvis in the anterior and posterior plane. [23, 24]
The use of the C-clamp leads to the closure of the bleeding surfaces caused by the pelvic trauma, allowing of clot maturation and hemodynamic control of the patient. The structure of the C-clamp allows to subsequently carry out all the necessary abdominal, vascular, pulmonary and bone fixation surgeries in the patient. [24-27]
In cases of an hemodynamically unstable patient with blunt pelvic trauma, associated with a mechanically unstable pelvis, and who does not respond to initial fluid resuscitation, the use of the C clamp is useful for hemodynamic stabilization of the trauma patient since it generates compression of the posterior sacroiliac joint. [28-30]
This device allows an intensified visualization of the sacroiliac joint and symphysis pubis and facilitates percutaneous stabilization of both joints, thus achieving definitive mechanical stability of the pelvis. [31] The sacroiliac joint is first stabilized percutaneously with the patient in the supine position.
Percutaneous stabilization of the pubic symphysis is carried out consecutively once the sacroiliac joint has been reduced and fixed.
Mu et al. reported that good pelvic ring stability is achieved when pubic diastasis is treated percutaneously with one or two screws. [32]
Cano et al., published a study on intact cadaveric, with the pubic symphysis fixed with plates and screws and trans-pubian screws (cross screws) subjected to an axial load of 300 N and demonstrated that in vitro the cannulated screws had the ability to resist rotational forces. [33] The authors also showed that before an axial load of 600N, the displacement of the cannulated screw was 0.643 mm and the plate was 0.408 mm and therefore that both fixing systems were efficient to support the load. [33] When the stress analysis was evaluated, it showed that the maximum stress of the cross-pubis screw was 30.92 MPa, while the plate amounts to 1846 MPa. This decrease in biomechanical stress presented by the cross screw is because the trans symphysial screw is an intramedullary osteosynthesis. [33] The trans symphysial pubic screw is as efficient as the plate to support the axial load, and has less biomechanical stress, it also has a shorter surgical time, with less blood loss and skin complications, due to this it is our choice of treatment. [32, 34]
In addition, Yu et al. have shown that both the plate and the trans-pubian screw are efficient for the reduction of the pubic symphysis and with the same functional result, without significant differences in implant failure and revision surgeries. [35]
Giannoudis et al. published postoperative complications with the use of an osteosynthesis plate for pubic diastasis, those are suprapubic pain, neurogenic impotence, and dyspareunia. [36]
Implant failure is common in pubic diastasis plating and varies in different studies from 28 to 75% of patients. The revision rate of these loosenings is very low and varies from 0.7 to 3.6% of the cases with loosening of the implant. [11, 37-39]
A study published this year by Tseng et al. shows that the male sex is the only cause that is positively correlated with implant failure. It is probably due to the differences in physical activities between both sexes. [40] The pubic symphysis joint has little movement under the usual physiological loads, being a 2-mm shift and 1-degree rotation in adults. [41]
Cavalcanti Kußmaul et al. published that symphyseal plating as a rigid osteosynthesis and prevents normal mobility symphyseal joint. [42]
The use of a single crossed screw between both pubis, provided antirotating and antishearing forces, allowing minimal joint movement. [43]
The placement of the second screw in the second corridor is controversial and should preferably be performed with the use of a three-dimensional browser along with the use of an ultrasound to avoid injury to the anatomical elements of the region. [43-45]
Conclusion
Hemodynamic and mechanical stabilization of the pelvis is essential for the treatment of pelvic trauma and can improve patient survival, especially in the first hours of trauma. Percutaneous stabilization of the posterior sacroiliac joint with one or two screws and the pubic symphysis with a crossed screw is usually sufficient reconstruction to achieve pelvic stability.
References
- Pereira GJC, Damasceno ER, Dinhane DI, Bueno FM, Leite JBR, Ancheschi BDC. ? (2017). Epidemiology of pelvic ring fractures and injuries. Rev Bras Ortop.;52(3): 260-9.
- Pizanis A, Pohlemann T, Burkhardt M, Aghayev E, Holstein JH. (2013). Emergency stabilization of the pelvic ring: Clinical comparison between three different techniques. Injury. 44(12): 1760-4.
- Heetveld MJ, Harris I, Schlaphoff G, Balogh Z, D'Amours SK, Sugrue M. (2004). Hemodynamically unstable pelvic fractures: recent care and new guidelines. World J Surg. 28(9): 904-9.
- Wang H, Robinson RD, Moore B, Kirk AJ, Phillips JL, Umejiego J, et al ? (2016). Predictors of early versus late mortality in pelvic trauma patients. Scand J Trauma Resusc Emerg Med. 24: 27.
- White CE, Hsu JR, Holcomb JB. (2009). Haemodynamically unstable pelvic fractures. Injury. 40(10): 1023-30.
- Dyer GS, Vrahas MS. (2006). Review of the pathophysiology and acute management of haemorrhage in pelvic fracture. Injury. 37(7): 602-13.
- Miller PR, Moore PS, Mansell E, Meredith JW, Chang MC. (2003). External fixation or arteriogram in bleeding pelvic fracture: initial therapy guided by markers of arterial hemorrhage. J Trauma. 54(3): 437-43.
- Sadri H, Nguyen-Tang T, Stern R, Hoffmeyer P, Peter R. (2005). Control of severe hemorrhage using C-clamp and arterial embolization in hemodynamically unstable patients with pelvic ring disruption. Arch Orthop Trauma Surg. 125(7): 443-7.
- Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR. (2007). Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: a paradigm shift. J Trauma. 62(4): 834-9; discussion 9-42.
- S. S, H. E, J.C. H, D. J, A. W. Inguinal canal. In: S S, editor. (2005). Gray’s anatomy: the anatomical basis of clinical practice. 39 ed. Edinburgh, Scotland: Elsevier Churchill Livingstone; p. 1109–11.
- Putnis SE, Pearce R, Wali UJ, Bircher MD, Rickman MS. (2011). Open reduction and internal fixation of a traumatic diastasis of the pubic symphysis: one-year radiological and functional outcomes. J Bone Joint Surg Br. 93(1): 78-84.
- Bircher MD. (1996). Indications and techniques of external fixation of the injured pelvis. Injury. 27 Suppl 2: B3-19.
- Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS, Jr., Poka A, et al. (1990). Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 30(7): 848-56.
- Liu Z, Wang K, Zhang K, Zhou J, Zhang Y. (2014). Minimally invasive surgery (MIS) of anterior ring fracture combined with pubic symphysis separation. Med Sci Monit. 20: 1913-7.
- Varga E, Hearn T, Powell J, Tile M. (1995). Effects of method of internal fixation of symphyseal disruptions on stability of the pelvic ring. Injury. 26(2): 75-80.
- Simonian PT, Schwappach JR, Routt ML, Jr., Agnew SG, Harrington RM, Tencer AF. (1996). Evaluation of new plate designs for symphysis pubis internal fixation. J Trauma. 41(3): 498-502.
- Matta JM. (1996). Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res. (329): 88-96.
- Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. (2014). Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 96-B(8): 1090-7.
- Balogh Z, Caldwell E, Heetveld M, D'Amours S, Schlaphoff G, Harris I, et al. (2005). Institutional practice guidelines on management of pelvic fracture-related hemodynamic instability: do they make a difference? J Trauma. 58(4): 778-82.
- Parry JA, Smith WR, Moore EE, Burlew CCC, Mauffrey C. (2021). The past, present, and future management of hemodynamic instability in patients with unstable pelvic ring injuries. Injury. 52(10): 2693-6.
- Park CH, Lee JW, Kim BS, Cho MR, Song SK. (2022). Prolonged ileus in traumatic pelvic ring injury patients who underwent arterial angio-embolization: A retrospective study. Medicine (Baltimore). 101(39): e30684.
- Committee on Trauma ACoS. Advanced Trauma Life Support. 10 ed. Committee on Trauma ACoS, editor. Chicago, IL, USA2018.
- Dahners LE, Jacobs RR, Jayaraman G, Cepulo AJ. (1984). A study of external skeletal fixation systems for unstable pelvic fractures. J Trauma. 24(10): 876-81.
- Pohlemann T, Krettek C, Hoffmann R, Culemann U, Gansslen A. (1994). [Biomechanical comparison of various emergency stabilization measures of the pelvic ring]. Unfallchirurg. 97(10): 503-10.
- Ganz R, Krushell RJ, Jakob RP, Kuffer J. (1991). The antishock pelvic clamp. Clin Orthop Relat Res. (267): 71-8.
- Pohlemann T, Culemann U, Gansslen A, Tscherne H. (1996). [Severe pelvic injury with pelvic mass hemorrhage: determining severity of hemorrhage and clinical experience with emergency stabilization]. Unfallchirurg. 99(10): 734-43.
- Ghanayem AJ, Stover MD, Goldstein JA, Bellon E, Wilber JH. (1995). Emergent treatment of pelvic fractures. Comparison of methods for stabilization. Clin Orthop Relat Res. (318): 75-80.
- Gewiess J, Luedi MM, Schnuriger B, Tosounidis TH, Keel MJB, Bastian JD. (2022). Effect of C-Clamp Application on Hemodynamic Instability in Polytrauma Victims with Pelvic Fracture. Medicina (Kaunas). 58(9).
- Schutz M, Stockle U, Hoffmann R, Sudkamp N, Haas N. (1996). Clinical experience with two types of pelvic C-clamps for unstable pelvic ring injuries. Injury. 27 Suppl 1: S-A46-50.
- Rommens PM, Hofmann A, Hessmann MH. (2010). Management of Acute Hemorrhage in Pelvic Trauma: An Overview. Eur J Trauma Emerg Surg. 36(2): 91-9.
- Hoch A, Zeidler S, Pieroh P, Josten C, Stuby FM, Herath SC, et al. (2021). Trends and efficacy of external emergency stabilization of pelvic ring fractures: results from the German Pelvic Trauma Registry. Eur J Trauma Emerg Surg. 47(2): 523-31.
- Mu WD, Wang H, Zhou DS, Yu LZ, Jia TH, Li LX. (2009). Computer navigated percutaneous screw fixation for traumatic pubic symphysis diastasis of unstable pelvic ring injuries. Chin Med J (Engl). 122(14): 1699-703.
- Cano-Luis P, Giraldez-Sanchez MA, Martinez-Reina J, Serrano-Escalante FJ, Galleguillos-Rioboo C, Lazaro-Gonzalvez A, et al. (2012). Biomechanical analysis of a new minimally invasive system for osteosynthesis of pubis symphysis disruption. Injury. 43 Suppl 2: S20-7.
- Chen L, Zhang G, Song D, Guo X, Yuan W. (2012). A comparison of percutaneous reduction and screw fixation versus open reduction and plate fixation of traumatic symphysis pubis diastasis. Arch Orthop Trauma Surg. 132(2): 265-70.
- Yu KH, Hong JJ, Guo XS, Zhou DS. (2015). Comparison of reconstruction plate screw fixation and percutaneous cannulated screw fixation in treatment of Tile B1 type pubic symphysis diastasis: a finite element analysis and 10-year clinical experience. J Orthop Surg Res. 10:151.
- Giannoudis PV, Chalidis BE, Roberts CS. (2008). Internal fixation of traumatic diastasis of pubic symphysis: is plate removal essential? Arch Orthop Trauma Surg. 128(3): 325-31.
- Kankanalu P, Orfanos G, Dwyer J, Lim J, Youssef B. (2021). Can locking plate fixation of symphyseal disruptions allow early weight bearing? Injury. 52(10): 2725-9.
- Morris SA, Loveridge J, Smart DK, Ward AJ, Chesser TJ. (2012). Is fixation failure after plate fixation of the symphysis pubis clinically important? Clin Orthop Relat Res. 470(8): 2154-60.
- Collinge C, Archdeacon MT, Dulaney-Cripe E, Moed BR. (2012). Radiographic changes of implant failure after plating for pubic symphysis diastasis: an underappreciated reality? Clin Orthop Relat Res. 470(8): 2148-53.
- Tseng KY, Lin KC, Yang SW. (2022). The radiographic outcome after plating for pubic symphysis diastasis: does it matter clinically? Arch Orthop Trauma Surg.
- Becker I, Woodley SJ, Stringer MD. (2010). The adult human pubic symphysis: a systematic review. J Anat. 217(5): 475-87.
- Cavalcanti Kussmaul A, Schwaabe F, Kistler M, Gennen C, Andress S, Becker CA, et al. (2022). Novel minimally invasive tape suture osteosynthesis for instabilities of the pubic symphysis: a biomechanical study. Arch Orthop Trauma Surg. 142(9): 2235-43.
- Yao F, He Y, Qian H, Zhou D, Li Q. (2015). Comparison of Biomechanical Characteristics and Pelvic Ring Stability Using Different Fixation Methods to Treat Pubic Symphysis Diastasis: A Finite Element Study. Medicine (Baltimore). 94(49): e2207.
- Yoong P, Duffy S, Marshall TJ. The inguinal and femoral canals: (2013). A practical step-by-step approach to accurate sonographic assessment. Indian J Radiol Imaging. 23(4): 391-5.
- Yoshida T, Nakamoto T, Kamibayashi T. (2017). Ultrasound-Guided Obturator Nerve Block: A Focused Review on Anatomy and Updated Techniques. Biomed Res Int.; 2017: 7023750.
Citation: Nosratollah Vatani, Federico Isobe Minoru, Jorge Vargas, Ana L. Douglas Price and Horacio A. Caviglia. (2023). Intramedullary Fixation of the Pubis in Unstable Pelvis. Journal of Orthopaedic and Trauma Care 4(1).
Copyright: © 2023 Ana L. Douglas Price. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.