Research Article
Volume 3 Issue 1 - 2022
Immediate Short-term Outcomes of Distal Radius Metaphyseal Fractures in Children
1MBChB (UKZN), FC Orth (SA), PG Diploma Health Research (OX), Fellow in Tumour and Sepsis unit Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, 7 York road Parktown, Johannesburg
2MBChB (UCT), orthopaedic registrar University of the Witwatersrand, 7 York road Parktown, Johannesburg
3MBChB (Wits), FC Orth (SA), orthopaedic specialist Chris Hani Baragwanath Academic Hospital University of the Witwatersrand, 7 York road Parktown, Johannesburg
4MBChB (Natal), FCS Orth (SA), MSc(Med)(Wits), orthopaedic Head of department University of the Witwatersrand, 7 York road Parktown, Johannesburg
2MBChB (UCT), orthopaedic registrar University of the Witwatersrand, 7 York road Parktown, Johannesburg
3MBChB (Wits), FC Orth (SA), orthopaedic specialist Chris Hani Baragwanath Academic Hospital University of the Witwatersrand, 7 York road Parktown, Johannesburg
4MBChB (Natal), FCS Orth (SA), MSc(Med)(Wits), orthopaedic Head of department University of the Witwatersrand, 7 York road Parktown, Johannesburg
*Corresponding Author: Philani Ntombela, MBChB (UKZN), FC Orth (SA), PG Diploma Health Research (OX), Fellow in Tumour and Sepsis unit Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, 7 York road Parktown, Johannesburg.
Received: May 20, 2022; Published: May 31, 2022
Introduction
Distal radius fractures are one of the commonest fractures in children [1]. Thirty percent (30%) to 40% of paediatric fractures occur in the forearm [2]. Fractures in the distal third of the forearm account for 75% to 84% [1,2]. This is followed by diaphyseal fractures and fractures to the growth plate respectively [3]. Management of these fractures has many controversies. These range from manipulation under anaesthesia (MUA) and casting alone versus the use of percutaneous pinning; the use of an above-elbow cast versus a forearm cast and the acceptable limits in cases of re-displacement. The aim of this project is to determine the immediate short-term outcomes of management in children treated for distal radius fractures. The distal radius is responsible for 80% of forearm growth and 40% overall upper extremity growth [4]. As a result, some studies report a radial and dorsal angular deformity up to 39° and 22° volar angulation with complete displacement to correct fully in children up to 10 years old [5]. Wim VAN Leemput reported an average of 7.5 months duration for remodelling in children with an open physis [6]. Major complications following distal radius fractures are rare [4], the commonly reported complication being the high rate of re-displacement (29–48%) [3,7]. McLauchlan in his randomized controlled trial (RCT) reported 21% of fractures to re-displace early after reduction [8]. Even after an anatomical reduction, loss of reduction (LOR) was observed in 24.6% [9]. A systematic review found percutaneous pinning to have a positive effect on maintaining the initial reduction and reducing fracture complication rate [10]. However, the decision for insertion of Kirchner-wires (k-wires) is not without controversy. Indications are unclear.
Authors mention that radiological malunion does not always correlate with loss of function and caution that, indiscriminate use of K-wires in all cases should be avoided [4]. In a study by Mazzini, dorsal comminution, mechanism of injury, an intact ulna and 3-point index were not found to be significant risk factors [1] Patients with initial coronal translation of 10% or more were 2.4 times more likely to lose reduction, and patients with residual sagittal translation ≥10% were 2.7 times more likely to lose reduction [1]. Wim VAN Leemput added ipsilateral ulna fracture and obliquity of the fracture to the risks for re-displacement and says that up to 25% of these re-displace in the first 24 hours of casting [6]. This is said to be improved by K-wire insertion, suggesting that the wire prevented displacement during application of the cast [8]. While McLauchlan acknowledges that the indications for K-wires vary, he observed that complications from the use of percutaneous wires were few and minor and no detrimental clinical effect at assessment at three months were found [8]. However, the use of percutaneous pinning is not benign. Further to this, no difference in terms of functional outcome when closed reduction and casting was compared to closed reduction and pinning was observed [1]. Pien Hellebrekers advises that even if re-displacement is seen during follow-up and this displacement is within the acceptable limits to allow remodelling without surgery [2]. A significant finding by a systematic review was that the superior results of function and radiographs seen with pinning seem to be short-lived, as all differences disappeared after completion of remodelling. No cost advantages have been found in the addition of percutaneous pinning group compared with the casting group [10]. Other reported complications of K-wire fixation include hypertrophic scarring, wire migration and neurapraxia [8,9]. Migration of K-wires occurred in 3.9% of children in a series by Fernandez [9]. Great merit does however exist for advocates of percutaneous pinning. Loss of position in the cast has been shown to be the most crucial factor affecting the position at union [8]. The same study reported 14 of 33 fractures in the cast-alone group lost position and those fewer radiographs were required in the K-wire group during follow-up [8]. A low success rate (58.8%) with closed reduction and cast alone was reported by Pien Hellebrekers [2].
However, markers of success were not clearly stated in this report. Ehab, I state that in total, 30% of the complete fractures were unstable in their report [5]. Loss of reduction in the cast is associated with a poorer outcome of malunion [8]. The epidemiological profile of this injury is consistent throughout literature. They account for up to 45% of all paediatric fractures [4]. We also know that they occur more often than diaphyseal fractures, girls are less frequently affected than boys and the most common cause of accidents is falling on an outstretched hand [9,11,12]. Forty-five percent (45%) involved the dominant side and 55% were on the non-dominant side [5]. Overall associated complications are rare and non-union is uncommon. The excellent remodelling potential allows for some degree of displacement to be accepted [1,9].
Patients and Methods
We conducted a retrospective study of patients who received treatement for distal radius metaphyseal fractures at Chris Hani Baragwanath Academic Hospital (CHBAH). The review period was from June 2018 to May 2019. The minimum follow-up period was 8 weeks post treatment.
We included patients that presented within 48 hours of the injury, close fractures, and patients under the age of 16 years. Patients with growth plate injuries, open injuries and bilateral fractures were excluded. We also excluded patients who received initial definitive treatment from other centres and those with inadequate medical records.
Extracted data included patient demographics; mechanism of injury (MOI); hand dominance; side of injury; pre-treatment fracture displacement; post-treatment fracture position after immediate treatment; post-treatment fracture position at union; treatment modality; type of POP used (above-elbow versus below-elbow); pin tract sepsis; fracture union. Once the data was extracted, it was assigned a study number. The use of personal identifying data was kept to the necessary minimum and patient confidentiality was protected. Our outcomes of interest were as listed:
- Time to union
- Rate of significant loss of reduction (LOR)
- Re-operation rate
- Complications of POP
- Rate of pin-tract sepsis
Cast indexes evaluation was not examined in this study but would be an important parameter to assess in future projects. Union was defined based on clinical and radiological findings. This was defined as a painless wrist with evidence of callus formation on radiographs (3 cortices). Significant LOR was defined as any loss of position that required an added intervention i.e., re-manipulation or k-wire insertion at follow-up. There was no precise definition used for pin-tract sepsis and this was left to the discretion of the treating surgeon at the time. All k-wires were left unburied. Patients that had k-wire insertion also received a below-elbow POP. Complications of POP were described as those directly linked to the use of the cast regardless of whether additional treatment was required because of this.
The treatment protocol followed depended on the selected treatment choice. Patients under the age of 8 years, treated with a cast were kept in it for 4 weeks regardless of the type of cast. This was kept for 6 weeks in patients who were 9 years and older. However, the cast was converted to a below-elbow cast at 3 weeks if an above-elbow cast had been used in this group. The period of keeping k-wires also followed the same age pattern as described for the cast-only group. Treatment was instituted by specialists in training and the chosen method was at their discretion.
The Pearson’s chi-squared test was used to analyse differences between groups of patients as decided by the treatment modality received. An independent sample t-test was also used to analyse continuous variables e.g., Patient’s age. The level of signi?cance was set at p < 0.05. STATA version 14.0 statistical package was used for data cleaning and analysis. To test the difference in mean of AP angulation and lateral angulation across the 3 groups of intervention (above elbow, below elbow and k-wire), ANOVA test was employed.
Results
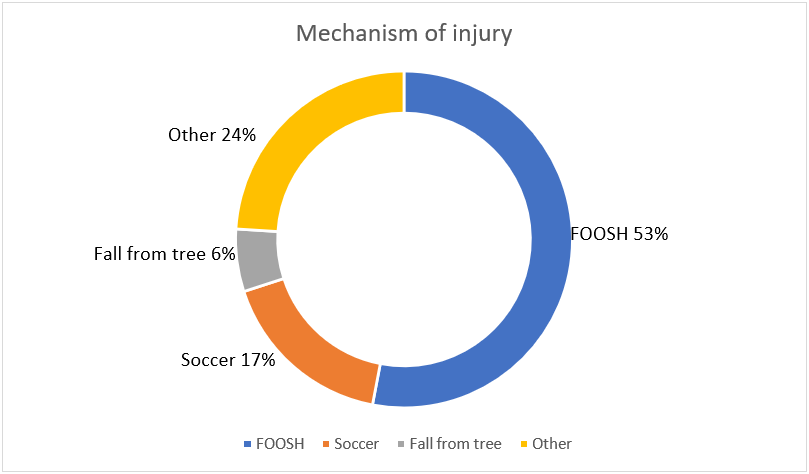
A total of 96 patients were included in the study. There were 76 boys & 20 girls (see Table I). The mean age was 9 years (2 - 14). Majority of patients were black Africans (92%, 88/96). Fifty eight percent (56/96) of patients injured the right side and 42% (40/96) injured the left side. Eighty six percent (83/96) of patients were right hand dominant while 3% (3/96) were ambidextrous. The dominant hand was injured in 96% (92/96) of patients. The commonest mechanism of injury was FOOSH at 53% (51/96) and followed by soccer injuries (17%,17/96) (see Figure 1).
| Gender | Male: 79% (76/96) |
| Female: 21% (20/96) | |
| Age (years) | 9.1 (2 – 14) |
| Injured side | Right: 58% (56/96) |
| Left: 42% (40/96) | |
| Dominant hand | Right: 86% (83/96) |
| Left: 11% (10/96) | |
| Ambidextrous: 3% (3/96) |
Table I: Demographics, injured side and dominant hand.
The most chosen treatment intervention was a below-elbow POP at 40% (38/96) (see Table II). Thirty nine percent (37/96) were treated in an above-elbow cast while 21% (21/96) had k-wire insertion. There was a 100% (96/96) union rate recorded. The mean time to union was 25 days (14 - 46). Three percent (3/96) of patients required re-operation for loss of reduction (LOR). In 3% (3/96) of patients the cast required bivalving because it was too tight. Pin-tract sepsis was seen in 3 of the 21 patients treated with k-wire insertion (14%, 3/21) (see Table III). The mean AP view (radial-ulna) angulation before treatment was 13.08 degrees (0 - 35), 0.08 degrees (0 - 4) after immediate treatment and 0.57 degrees (0 - 5) at the time of union (4 - 6 weeks). The mean lateral view (volar-dorsal) angulation was 7.94 degrees (0 - 25) before treatment, 0.57 degrees (0 - 7) after initial treatment and 0.92 degrees (0 - 7) at union (see Table II). Mean fracture shortening was 1.16cm before treatment with bayoneting in 47% (45/96) of patients.
In the above-elbow POP group, the average age was 8.27 years (2 - 13). The average pre-treatment fracture displacement on AP and lateral view was 8.38 degrees (0 – 25) for both (see Table II). Immediately after fracture reduction, the average fracture displacement on AP and lateral view was 0.22 degrees (0 - 4) and 0.95 (0 - 4) respectively. At the time of fracture union, the average fracture displacement on AP and lateral view was 0.54 degrees (0 - 5) and 1.24 degrees (0 - 5) respectively in this group.
| Below-elbow | Above-elbow | K-wires | Overall | |
| Total | 40% (38/96) | 39% (37/96) | 21% (21/96) | 96 |
| Pre-treatment AP view angulation | 13.63 (0 – 36) | 8.38 (0 – 25) | 14.71 (5 – 30) | 13.08 (0 – 35) |
| Pre-treatment lateral view angulation | 7.16 (0 – 25) | 8.38 (0 – 25) | 8.57 (0 – 20) | 7.94 (0 – 25) |
| Immediate post-treatment AP view angulation | 0 | 0.22 (0 – 4) | 0 | 0.08 (0 – 4) |
| Immediate post-treatment lateral view angulation | 0.53 (0 – 7) | 0.95 (0 – 4) | 0 | 0.57 (0 – 5) |
| AP view angulation at union | 0.47 (0 – 5) | 0.54 (0 – 5) | 0.81 (0 – 6) | 0.57 (0 – 5) |
| Lateral view angulation at union | 0.89 (0 – 7) | 1.24 (0 – 5) | 0.38 (0 – 5) | 0.92 (0 – 7) |
Table II: Degree of angulation between the 3 treatment groups, the mean and range is given in degrees.
| Below-elbow | Above-elbow | K-wires | Overall | |
| LOR | 3% (3/96) | 0 | 0 | 3% (3/96) |
| Tight cast | 1% (1/96) | 2% (2/96) | 0 | 3% (3/96) |
| Pin-tract sepsis | 0 | 0 | 14% (3/21) | 3% (3/96) |
| Open reduction | 0 | 0 | 2% (2/96) | 2% (2/96) |
| Total | 4% (4/96) | 2% (2/96) | 14% | 9% (9/96) |
Table III: Complications encountered: “Open reduction” is not considered a complication in this study.
In the below-elbow POP group, the average age was 9.74 years (2 - 14). The average pre-treatment fracture displacement on AP and lateral view was 13.63 degrees (0 - 36) and 7.16 degrees (0 – 25) respectively (see Table II). Immediately after fracture reduction, the average fracture displacement on AP and lateral view was 0 degrees and 0.53 degrees (0 – 7) respectively. At the time of fracture union, the average fracture displacement on AP and lateral view was 0.47 degrees (0 – 5) and 0.89 degrees (0 – 7) respectively.
In the k-wire group, the average age was 9.60 years (6 – 13). The average pre-treatment fracture displacement on AP and lateral view was 14.71 degrees (5 – 30) and 8.57 degrees (0 – 20) respectively (see Table II). Immediately after fracture reduction, the average fracture displacement on AP and lateral view was 0 for both. At the time of fracture union, the average fracture displacement on AP and lateral view was 0.81 degrees (0 – 6) and 0.38 degrees (0 – 5) respectively.
The pre-treatment mean AP angulation showed statistically significant difference between the 3 groups (p = 0.0112) while the mean lateral angulation showed no statistically significant difference (p = 0.6975) (see Table IV).
There was no statistically significant difference in mean AP angulation at the immediate post-treatment stage across all the groups (p = 0.2009) as well as for the mean lateral angulation at this stage (p = 0.0712) (see Table V).
| Group (AP) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 8.4 | 6.7 | 37 | 0.0112 |
| Below elbow | 13.6 | 10.4 | 38 | 0.6975 |
| K-wire | 14.7 | 9.2 | 21 | |
| Group (Lateral) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 8.4 | 6.7 | 37 | 0.6975 |
| Below elbow | 7.2 | 7.7 | 38 | |
| K-wire | 8.6 | 7.6 | 21 |
Table IV: Pre-treatment angulation.
There was no statistically significant difference in mean AP angulation at the 6 weeks post-treatment stage across all the groups (p = 0.7066) as well as the mean lateral angulation (p = 0.2259) (see Table VI).
The difference in mean AP angulation at the pre-treatment stage between the below-elbow and above-elbow group was statistically significant (p = 0.031). Similarly, the difference in mean AP angulation at the pre-treatment stage between K-wire and above-elbow group was statistically significant (p = 0.027). No significant difference in mean AP angulation at the pre-treatment stage was observed between K-wire and below-elbow group (see Table V).
| Group (AP) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 0.22 | 0.92 | 37 | 0.2009 |
| Below elbow | 0 | 0 | 38 | 0.0712 |
| K-wire | 0 | 0 | 21 | |
| Group (Lateral) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 0.95 | 1.7 | 37 | 0.0712 |
| Below elbow | 0.53 | 1.6 | 38 | |
| K-wire | 0 | 0 | 21 |
Table V: Immediate post-treatment angulation.
| Group (AP) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 0.54 | 1.4 | 37 | 0.7066 |
| Below elbow | 0.47 | 1.4 | 38 | 0.2259 |
| K-wire | 0.81 | 1.8 | 21 | |
| Group (Lateral) | Mean | Standard deviation | Frequency | p value |
| Above elbow | 1.2 | 1.9 | 37 | 0.2259 |
| Below elbow | 0.9 | 2.0 | 38 | |
| K-wire | 0.38 | 1.2 | 21 |
Table VI: 6 weeks post-treatment angulation.
Discussion
Metaphyseal distal radius fractures are commonly seen in pubertal growth ages, 11-14 years in males and 8-11 year in females [5]. These occur more in boys than in girls [9]. Findings in this study are similar to these facts. The mean age of our group was 9 years (2-14) and 79% (76/96) of these were boys.
Our study showed a 3% (3/96) rate of significant LOR. It occurred in patients that were treated with a below-elbow cast. This is a low rate when compared to the available literature. In his report, Wim Van Leemput stated that 45.8% of patients showed a marked displacement after reduction and cast immobilisation [6]. Mazzini found a 35% re-displacement rate [1]. We defined significant LOR as that requiring a secondary procedure. This remarkably reduced the rate of significant LOR in this study as not every loss of position was acted on. Important risk factors for re-displacement vary. Complete initial displacement, non-anatomical reduction and poor plaster application technique are among the listed [4]. Forty seven percent of our patients had fracture bayoneting at the time of injury. However, as depicted in table II, pre-treatment AP and lateral angulation was not very severe. Also worth noting is that patients older than 14 years are 4.8 times more likely to lose reduction and patients with residual translation of 10% in the sagittal plane are 4 times more likely to lose reduction [1]. In another study, 13% of patients underwent a closed reduction and k-wire insertion because of re-displacement [6]. Only 3% of our patients required k-wire insertion after LOR a week after the initial casting. Constantino et al. concluded that the quality of reduction was the only risk factor found to be predictive of re-displacement [13]. This study however had a small sample size (26).
A 17% complication rate related to the use of k-wires is reported, with a deep infection rate of 2% [4]. Fernandez reported a pin-tract infection rate of 5.19% in his patients [9]. Pin-tract infection developed in 10% of patients in a study by Ehab I [3]. No deep infection was recorded in our study and the pin-tract sepsis rate was 14% (3/21). Our definition of pin-tract sepsis was not stipulated and was left to the discretion of the treating surgeon. A higher recording might have been documented otherwise.
An open reduction was done in 2% (2/96) of the patients. These patients were pinned in the same sitting. Open reduction may be required in 8% of cases [8]. Some authors found no “superiority of reduction and pin fixation over cast immobilization in the bayonet position of closed overriding distal metaphyseal radius fractures in children under ten years” [14]. Sinikumpu and Nietosvaara also advice that both options (pinning vs cast-only) are viable for bayoneting fractures in pre-pubertal patients [15]. Such a finding is important. It implies reduced treatment costs for patients and avoiding unnecessary sedation with its associated risks. Orland and his colleagues found that 27% of the manipulations done in the emergency department were potentially unnecessary [16]. They concluded that improving awareness of acceptable deformities in young children may substantially reduce health-care costs [16]. A recent retrospective study has reported overweight children to have 2 times the risk of normal-weight children for re-displacement and that they are at an increased risk for reduction failure [17]. Cast related complications happened in 3 of our patients. All 3 required that the cast be bivalved because of severe swelling and tightness as a result. Two of these were in an above-elbow cast and 1 in a below-elbow cast. Worth noting however is that none of these patients lost the pre-achieved position and no compartment syndrome ensued.
The current study had a 9% (9/96) complication rate (3 tight casts, 3 secondary operations and 3 pin-tract sepsis).
The retrospective design of this study is a limitation. Another limitation present is that of not applying a standard definition for pin-tract sepsis. This might have grossly underestimated this complication. The definition of significant loss of reduction was essentially left to the discretion of the treating surgeon because it relies on the patient requiring a secondary procedure. This decision was individualised and not based on any consensus. A randomised control trial would be able to give better answers.
Conclusion
The overall complication rate associated with distal radius metaphyseal fractures in children is relatively low. The use of K-wires is not a benign undertaking and should be reserved for specific cases that demand it. Good outcomes can be expected in the management of this injury but potential complications must be discussed with the parents and patient.
References
- Mazzini JP, Beck N, Brewer J, Baldwin K, Sankar W, Flynn
J. (2012). Distal metaphyseal radius fractures in children following closed reduction and casting: can loss of reduction be predicted. International orthopaedics (SICOT) 36: 1435-1440. - Hellebrekers P, de Vries LS, Timmers TK. Displaced Distal Forearm Fractures in Children. J Trauma Treat 2016, 5:4.
- Ehab I, El-Desokey, Kandil AE. (2013). Closed reduction with pinning of metaphyseal fractures of the distal radius in children. Egyptian orthopaedic journal, 48: 194-199.
- Firth GB, Robertson AJF. (2017). Treatment of distal radius metaphyseal fractures in children: a case report and literature review. SA Orthop J 16(4).
- Akar D, Korogul C, Erkus S. Conservative follow-up of severely displaced distal radial metaphyseal fractures in children. Cureus 10 (9): e3259.
- Van Leemput W, De Ridder K. (2009). Distal metaphyseal radius fractures in children: reduction with or without pinning. Acta Orthop. Belg. 75, 306-309.
- Mazzini JP, MartinJR. (2010). Paediatric forearm and distal radius fractures: risk factors and re-displacement-role of casting indices. International Orthopaedics (SICOT) 34: 407-412.
- McLauchlan GJ, Cowan B, Annan HI, Robb JE. (2002). Management of completely displaced metaphyseal fractures of the distal radius in children. A Prospective Randomized Controlled Trial. J Bone Surg [Br] 84-B: 413-7.
- Fernandez FF, Zander M, Peterlein CD, Daniel H, Schofer MD (2017). A retrospective study comparing conservative cast treatment and surgical k-wire pinning in severely and completely displaced distal metaphyseal radius fractures in children. J Trauma Care 3(1): 1014.
- Zeng ZK, Liang W, Sun Y et al. ((2018). Is percutaneous pinning needed for the treatment of displaced distal radius metaphyseal fractures in children? A systematic review. Medicine 97:36.
- Chivers DA, Hilton TL, Dix-Peek. (20130. An assessment of three-point index in predicting the redisplacement of distal radial fractures in children. SA Orthopaedic Journal Winter. Vol 12 – No 2.
- Randsborg P (2013). Fractures in children. Acta Orthopaedica, 84:sup350, 1-24.
- Constantino DMC, Machado L, Carvalho M, Cabral J, Sa? Cardoso P, Balaco? I, Ling TP, Alves C. (2021). Redisplacement of paediatric distal radius fractures: what is the problem? J Child Orthop. Dec 1;15(6): 532-539.
- Laaksonen T, Puhakka J, Stenroos A, Kosola J, Ahonen M, Nietosvaara Y. (2021). Cast immobilization in bayonet position versus reduction and pin fixation of overriding distal metaphyseal radius fractures in children under ten years of age: a case control study. J Child Orthop. Feb 1;15(1): 63-69.
- Sinikumpu JJ, Nietosvaara Y. (2021). Treatment of Distal Forearm Fractures in Children. Scand J Surg. Jun;110(2): 276-280.
- Orland KJ, Boissonneault A, Schwartz AM, Goel R, Bruce RW Jr, Fletcher ND. Resource Utilization for Patients with Distal Radius Fractures in a Pediatric Emergency Department. JAMA Netw Open. 2020 Feb 5;3(2): e1921202.
- Liu Y, Liu C, Guo D, Wang N, Zhao Y, Li D. (2021). Effect of childhood overweight on distal metaphyseal radius fractures treated by closed reduction. J Orthop Surg Res. Mar 10;16(1): 182.
Citation: Philani Ntombela, Winifred Mukiibi, Loyiso Gqamana and Mmampapatla Ramokgopa. (2022). Immediate Short-term Outcomes of Distal Radius Metaphyseal Fractures in Children. Journal of Orthopaedic and Trauma Care 3(1). DOI: 10.5281/zenodo.6601116
Copyright: © 2022 Philani Ntombela. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.