Case Report
Volume 5 Issue 1 - 2023
Extramedullary Plasmacytoma in the Sinonasal Cavity: A Case Report
1Medical Officer III, ORL-HNS, Philippines
2M.D., FPSO-HNS, Medical Specialist IV, ORL-HNS, Philippines
2M.D., FPSO-HNS, Medical Specialist IV, ORL-HNS, Philippines
*Corresponding Author: Arianna Danielle Nano, Rizal Medical Center Pasig Boulevard Barangay Bagong Ilog Pasig City, Philippines 1600.
Received: February 20, 2023; Published: March 03, 2023
Abstract
A 48-year-old male was diagnosed with a rare head and neck tumor of solitary extramedullary plasmacytoma. Limited literature exists on the management of extramedullary plasmacytoma. Radiation therapy remain to be the mainstay treatment but surgery can be utilized for symptomatic relief, increasing radiation effectiveness, and in cases of neurologic instability. Due to lack of consensus guidelines for its management, a multidisciplinary team conference was held to discuss the management for the patient. The patient underwent endoscopic tumor debulking with medial maxillectomy, followed by postoperative radiation. Post-treatment, the patient had post-radiation symptoms such as decreased vision and hearing but with gross disease improvement and improved obstructive symptoms. Magnetic resonance imaging done one month after treatment showed no residual disease.
Keywords: Plasmacytoma; Extramedullary plasmacytoma; Solitary plasmacytoma; Sinonasal tumor
Introduction
Plasma cells arise from the bone marrow with the main function of antibody production to help ward against systemic infection. However, there are instances that these cells proliferate in number and become malignant. This disease spectrum shows either a localized malignant plasmacytic proliferation, called solitary plasmacytoma, or a disseminated, systemic form, known as multiple myeloma. Plasmacytoma occurs only in 3% of the plasmacytic malignancies, hence, considered a rare tumor [3]. Solitary plasmacytoma can be further classified into a non-osseous extramedullary plasmacytoma (EMP) for those that arise from the soft-tissue, and a solitary bone plasmacytoma for those that arise from the bone [6,8]. For extramedullary plasmacytoma in the head and neck region, literature points to an incidence of only 1%. Commonly, patients diagnosed with EMP are males who are between 50-80 years of age. The most frequent location of EMP involves the nasopharynx and paranasal sinuses 75% of the time [9].
The plasmacytic diseases have to be distinguished from each other because of the differences in the management and respective prognosis. A disseminated bone or marrow involvement will be diagnosed as multiple myeloma, whereas, limitation to one location will entail a diagnosis of a solitary plasmacytoma. Due to the rarity of the disease, currently, no consensus guidelines exist for its management. Existing literature mostly comes from case reports, while some practiced a multidisciplinary team conference to arrive at a treatment approach [5]. In the Philippines, there is currently only one published case of extramedullary plasmacytoma which tackled the surveillance of plasmacytoma over a 7-year period post-radiotherapy [3].
Ethical considerations
An informed consent from the patient was obtained. IRB exemption will be applied for.
An informed consent from the patient was obtained. IRB exemption will be applied for.
Case Presentation
A 48-year-old male, known diabetic, sought consult at a tertiary government hospital’s Otorhinolaryngology-Head and Neck Surgery (ORL-HNS) out-patient department for a three-month history of left nasal obstruction with occasional bouts of left-sided epistaxis, and frontoparietal headache with 6/10 in severity. He denies symptoms of hyposmia, facial pain, pallor, weakness, and loss of consciousness.
He was previously managed at an emergency room of a private hospital wherein physical examination of the nose revealed a left intranasal mass, hence, computed tomography (CT) of the paranasal sinuses was requested.
Imaging results (see Figure 1) revealed an enhancing 5.8x 3.0x5.0 cm soft tissue mass in the left nasal cavity with bone erosion of the following: left lamina papyracea, left lacrimal bone, left fovea ethmoidalis, left cribriform plate, left sphenoid sinus, anterior wall, and medial wall of left maxillary sinus. Extraconal extension of the mass towards the left orbit with compression of the left medial rectus was also noted. Biopsy of the left intranasal mass revealed round cell neoplasm. Immunohistochemical stains were facilitated which showed positive for CD138 and Kappa, pointing to a diagnosis of plasmacytoma. Due to financial limitations, the patient decided to transfer to a tertiary government hospital.
On physical examination, the patient appears to have a left infraorbital bulge, described as non-hyperemic, non-tender, causing lateral deviation of the left eye. Similarly, the worm’s and eagle’s view of the patient showed superolateral left eye displacement. Gross nasal examination was unremarkable. On nasal endoscopy, the right nasal cavity is narrowed due to deviation of the septum. The left nasal cavity is completely filled with fleshy mass with some necrotic tissue and mucoid discharge. The inferior and middle turbinate in the left nasal cavity cannot be visualized. No oropharyngeal extension of the mass and no palpable neck masses were noted.
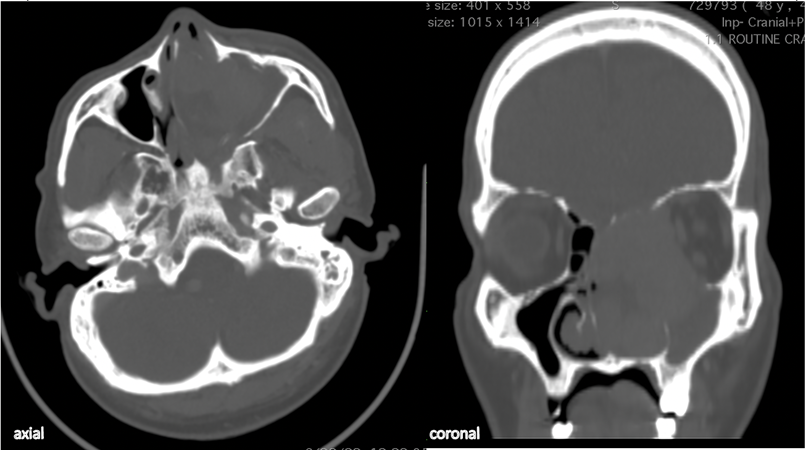
Figure 1: Axial and coronal cuts of the CT scan in bone window showing a 5.8x 3.0x5.0 cm mass occupying the entire left intranasal cavity with extensions to the left pyriform aperture, medial aspect of the left extraconal orbit; bony erosions can be visualized at the left lamina papyracea, left fovea ethmoidalis, left lacrimal bone, left cribriform plate, and left maxillary sinus.

Figure 2: Facial profile of the patient showing the left infra-orbital extension of the mass causing superolateral deviation of the left eye.
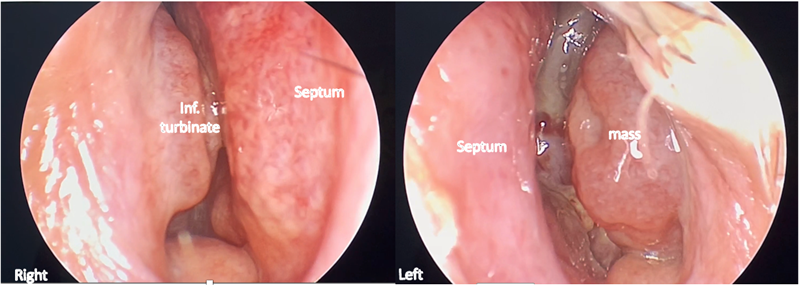
Figure 3: Nasal endoscopy showed a narrowed anterior portion of the bilateral nasal cavities. Right nasal septum showed bulging of septum due to mass effect; left nasal cavity showed presence of fleshy left intranasal mass.
Pre-operative management
Multidisciplinary team discussion
Upon transfer at our institution, a multi-disciplinary approach [5] was employed to provide holistic management for the patient. The following subspecialties were involved: 1) Internal Medicine - Hematology section, 2) Internal Medicine - Oncology section, 3) Radiation Oncology, 4) Ophthalmology, and lastly, 4) Otorhinolaryngology-Head & Neck surgery.
Multidisciplinary team discussion
Upon transfer at our institution, a multi-disciplinary approach [5] was employed to provide holistic management for the patient. The following subspecialties were involved: 1) Internal Medicine - Hematology section, 2) Internal Medicine - Oncology section, 3) Radiation Oncology, 4) Ophthalmology, and lastly, 4) Otorhinolaryngology-Head & Neck surgery.
The Internal Medicine- Oncology service’s inputs focused on establishing the diagnosis by differentiating between the localized and disseminated form of plasmacytic proliferation. Work-ups done included bone marrow aspiration biopsy (BMA) to quantify plasma cells, and whole body scan to determine areas of osteolysis and disease dissemination. Serum electrophoresis was also requested to check elevation of heavy chain monoclonal protein made by myeloma cells, but unfortunately was not done due to financial constraints. The results were as follows: BMA showed normocellular bone marrow with normal hemoglobin and plasma cell count while the whole-body scan revealed limited osteoblastic activity in the left maxillary area, leading to a diagnosis of solitary plasmacytoma in the left maxilla and offering our patient a better prognosis compared to a diagnosis of multiple myeloma.
Due to the fact that plasmacytoma is very responsive to radiation therapy, the involved services have agreed that the patient’s management would definitely include radiation therapy.
Radiation oncology underlined the importance of and the side effects that accompany radiation therapy. Because of the extraconal extension to the left orbit, one of the most pressing adverse effects is retinopathy. The patient expressed a desire to maintain vision if possible. The Ophthalmology service hence requested baseline ophthalmologic tests and repeat of such tests post-treatment. However, they deemed that radiotherapy is sufficient for the orbital extent and no ophthalmologic surgical management was necessary.
The Otorhinolaryngology, Head and Neck service on the other hand, considered the patient’s desire for relief of obstructive symptoms, hence offered the patient endoscopic tumor debulking of intranasal mass under general anesthesia with possible conversion to lateral rhinotomy if with uncontrollable bleeding. The patient underwent left inferior turbinectomy and partial medial maxillectomy. Debulking laterally extended up to the medial aspect of the left maxillary sinus, and posteriorly up to the area of the nasopharynx Approximately 5x3cm total mass area was removed.
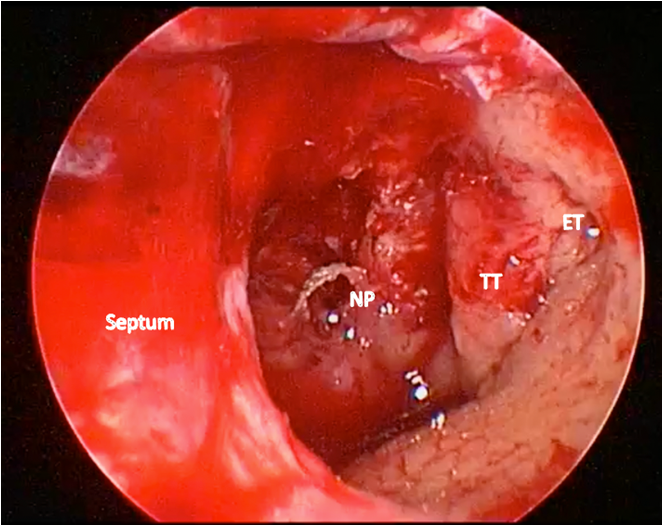
Figure 4: Left nasal cavity after debulking; NP - nasopharynx, TT - Torus Tubarius, ET - Eustachian Tube
Post-operative management
Post-operatively, J.B. underwent 25 days of Intensity-Modulated Radiation Therapy (IMRT) with a dose of 50 Gy radiation therapy. For residual disease monitoring, the patient underwent contrast-enhanced MRI of the cranium with paranasal sinuses after 6-8 weeks of radiation which showed findings of post-operative granulation tissue around the surgical bed, and inflammatory changes in the left paranasal maxillary sinus (See Figure 6). Additional monitoring include Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), and C-reactive protein (CRP). All of the tests were unremarkable except for the elevated ESR.
Post-operatively, J.B. underwent 25 days of Intensity-Modulated Radiation Therapy (IMRT) with a dose of 50 Gy radiation therapy. For residual disease monitoring, the patient underwent contrast-enhanced MRI of the cranium with paranasal sinuses after 6-8 weeks of radiation which showed findings of post-operative granulation tissue around the surgical bed, and inflammatory changes in the left paranasal maxillary sinus (See Figure 6). Additional monitoring include Complete Blood Count (CBC), Erythrocyte Sedimentation Rate (ESR), and C-reactive protein (CRP). All of the tests were unremarkable except for the elevated ESR.

Figure 5: Profile of patient J.B. 25 days post-radiation therapy showing decreased left lower lid bulge.
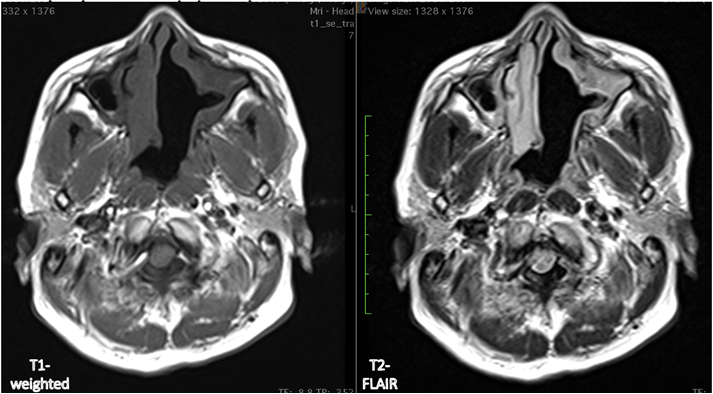
Figure 6: Post-radiation imaging in T1 weighted imaging and T2-FLAIR after surgery and radiation therapy showing absence of the previously noted intranasal mass but with inflammatory changes.
Discussion
The existing literature fits the epidemiology and disease presentation [3,5] of patient J.B. The suggested work-up for differentiating disseminated from localized disease were utilised but due to financial limitations of the patient, some were not done. Nonetheless, the patient was diagnosed with a localised extramedullary plasmacytoma. Existing literature states that radiation therapy is the only treatment for those that cannot be completely resected. Some studies support surgical intervention for structural instability and symptomatic relief, which was done in this case, because of the patient’s desire for immediate relief from the obstructive symptoms.
Common symptoms that patients experience after undergoing RT to the head and neck are taste dysfunction, mucositis, and ototoxicity [1]. In his case, he experienced altered taste sensation, decreased hearing in both ears, and thickened nasal discharge, which were individually addressed. Nasal douching with saline solution to alleviate the thick nasal discharge. Dietary referral for creating more palatable food choices to address the altered taste was done. Ototoxicity, on the other hand, was measured post-radiation to assess the severity of decrease in hearing, which in our patient showed bilateral moderate mixed hearing loss. Important to note, however, is that no baseline hearing tests were done. Similar to baseline ophthalmologic examination, we suggest that a baseline hearing test be routine for head and neck malignancies with expected radiation therapy as part of the treatment regimen [10]. Upon follow-up, six months post-surgery and four months post-radiation therapy, the patient has overall improved nasal obstruction, but has persistent nasal discharge. In addition, due to the irradiation to the region of the eyes and ears, he noted worsening of both vision and hearing, more prominent in the left, which was the side of the mass.
Conclusion
A patient with extramedullary plasmacytoma has been managed with surgical debulking and radiation. As part of the management of the disease, treatment goals were discussed to match with the patient’s expectations. Post-treatment, he is currently deemed disease-free, but has experienced adverse effects of radiation therapy, which were addressed symptomatically.
Few studies currently support the surgical management of extramedullary plasmacytoma, but most studies advocate radiation therapy. Additional studies may be necessary to support surgical management of extramedullary plasmacytoma. As one of the few studies that exist in the Philippines, we recommend pre-operative ophthalmologic and hearing evaluation prior to initiation of radiation. In the long run, regular monitoring must be done for surveillance of recurrence or possible conversion to disseminated disease.
References
- Abraham, Z., Ngunyale, B., Massawa, E., Ntzunagi, D., & Mpondo, B. (2018). Oral and otolaryngological complications of radiotherapy for head and neck cancers among patients attending Ocean Road Cancer Institute Tanzania. Medical Journal of Zambia, Vol. 45 (1): 32–43.
- Andrews RE, Brown JE, Lawson MA, Chantry, AD. (2021). Myeloma Bone Disease: The Osteoblast in the Spotlight; Journal of Clinical Medicine; 10(17):3973.
- Azman, M., Gendeh, B., & Ali, S.A. (2011). Extramedullary plasmacytoma of the nasopharynx: A rare tumor with 7-year follow-up. Philippine Journal of otolaryngology-Head and neck Surgery.
- Balakrishnan, P.H., Singh, R., Pujary, K., & Aziz, B. (2011). Solitary Extramedullary Plasmacytoma of the Sinonasal Region.
- Grammatico, S., Scalzulli, E., & Petrucci, M.T. Solitary plasmacytoma; 2017.
- Luh, SP., Lai, YS., Tsai, CH. (2007). Extramedullary plasmacytoma (EMP): Report of a case manifested as a mediastinal mass and multiple pulmonary nodules and review of literature. World J Surg Onc 5, 123.
- Nyunt, W., Draman, R., Mustapha, W., Karim, N., Idris, M., Abdullah, N., Loong, T., Jamaludin, W., Masir, N., Wahid, F. (2008). Multi-Disciplinary Approach for Managing Plasmacytoma: A Case Report.
- O’ Connell, T., Horita, T., Kasravi, B. (2005). Understanding and interpreting serum protein electrophoresis. Am Fam Physician. 2005;71(1):105-112.
- Jeyaraj, P., Venkatesan, M., & Nijhawan, V.S. (2016). Solitary extramedullary plasmacytoma of the maxillary sinus, progressing to smoldering multiple myeloma with multifocal skeletal involvement, which Resolved Completely Following Chemotherapy Alone.
- NCCN Continuing Education. NCCN Guidelines® Insights - Multiple Myeloma, Version 3.2022 | NCCN Continuing Education. [cited 2023 Jan 08]. Retrieved November 20, 2022, from https://education.nccn.org/node/91062
- Sarin V. (2019). Adverse Cochlear Effects After Head and Neck Cancer Therapy. Indian J Otolaryngol Head Neck Surg. Oct;71(Suppl 1): 740-747.
- Stifter S, Babarovi? E, Valkovi? T, Seili-Bekafigo I, Stemberger C, Nacinovi? A, Lucin K, Jonji? N. (2010). Combined evaluation of bone marrow aspirate and biopsy is superior in the prognosis of multiple myeloma. Diagn Pathol. 2010 May 18; 5:30.
Citation: Arianna Danielle M. Nano and Giancarla Marie C. Ambrocio. (2023). Extramedullary Plasmacytoma in the Sinonasal Cavity: A Case Report. Journal of Otolaryngology - Head and Neck Diseases 5(1). DOI: 10.5281/zenodo.7707486
Copyright: © 2023 Arianna Danielle Nano. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
