Research Article
Volume 1 Issue 1 - 2019
Distribution of Stillbirth Causes in Chile between Years 2002-2015
Department of Obstetrics and Neonatal Nursing, Faculty of Health Sciences, University of Atacama, Chile
*Corresponding Author: David San Martín Roldán, Department of Obstetrics and Neonatal Nursing, Faculty of Health Sciences, University of Atacama, Chile.
Received: July 17, 2019; Published: July 23, 2019
Abstract
Introduction: A stillbirth is a pregnancy event that is a negative result for parents, families and health personnel involved. The lack of resources could be the main obstacle to access to prenatal care, a symptom of health inequities. The weak knowledge of causes of stillbirth is associated with the belief that they are inevitable; however, many binding factors are potentially modifiable.
Objective: Describe of stillbirths causes in Chile.
Material and Methods: Cross-sectional and analytical study. The analysis was determined from the 22 gestational weeks, according to standard criteria of the World Health Organization. The most frequent causes were used to determine association by means of test x2 with statistical significance level p <0.05.
Results: The highest percentage of fetal deaths was recorded at 35 or more weeks (35.63%). Main macro-causes of stillbirth were fetal (47.0%), placental (31.4%) and unknown (10.89%). Main specific causes were intrauterine hypoxia (24.4%), unspecified cause (10.87%), and placental morphological-functional abnormalities (10.83%). Specific cause intrauterine hypoxia is associated with gestational age, maternal age and maternal educational level (p <0.05).
Conclusion: Prenatal health reflects obstetric care, quality and progress in health care. There are gaps in the detection of causes and quality of records, so that unknown causes tend to rise over time. It is advisable to add maternal temporal, biological and social components to the registry of fetal deaths.
Keywords: Stillbirth; Fetal Death; Pregnancy Outcome; Health Inequities; Cause of Death; Risk Factors
Introduction
The medicalization and institutionalization of childbirth have expanded in order to improve indicators of obstetric care, reducing maternal and neonatal morbidity and mortality rates. However, a stillbirth -death or stillbirth from the 22 gestational weeks- is an event of pregnancy, which is a negative result for parents, families and health personnel involved. [1-6]
The fetal death is related to the level of development of the countries and their levels of economic income. The lack of resources could be the main obstacle to access to prenatal care, a symptom of health inequities. [7,8] 2.6 million third-trimester fetuses die annually worldwide, 98% occurred in developing countries, a stable figure since 2011. Worldwide, one in three stillbirths was alive before the labor began and died for a cause of preventable death. [7,9,10,11]
The growing concern about the risk of stillbirth explains the intensive intrapartum fetal monitoring and the increase in the frequency of caesarean sections in middle and high income countries; being that prevention should be the appropriate strategy, and to prevent it is necessary to know the current state of the situation in stillbirths. [7,9,12,13]
The World Health Organization (WHO) defines stillbirth as the product of conception born dead before or during labor. This standard definition considers fetuses ≥ 22 gestational weeks, or weight ≥ 500 grams, or body length ≥ 25 centimeters. [12]
Because stillbirths are often not heavy, the gestational age criterion is the most commonly used in Chile, in high income countries and is thus specified in the International Classification of Diseases - Tenth Revision (ICD-10). [9,12,14]
The figure made by Healthy People 2010 recommends a rate of 4.1 fetal deaths per 1000 births. In Chile to the year 2010, the figure was 8.6 per 1000 live births according to the Perinatal Guide (2015 edition), however, the data are out of date, since 2005 death certificate has been issued to any product of the conception. Therefore, we do not know the real rate of Chilean stillbirths. [15,16]
The registries of stillbirths worldwide are untidy and only indicators of fetal mortality are known in 36% of the total of countries (and many less reports causes). This leads to underestimation of stillbirths in different countries, which indicates the need to strengthen registration systems. [15]
The studies carried out on the risk factors of stillbirths that use vital statistics are limited, based on the quality of the records.
The weak knowledge of causes of stillbirth is associated with the belief that they are unavoidable, however, many factors linked to stillbirth are potentially modifiable, such as: infections, chronic non-communicable diseases, nutritional factors, drugs, smoking, inadequate prenatal care, professional absence of childbirth, low socioeconomic level, and low or no maternal education, rurality and home birth. [(17]
The aim of this work is described go the stillbirth causes in Chile between the years 2002-2015 and the possibly associated multidimensional factors.
Material and Methods
Transversal and analytical study. The public database DEIS-MINSAL (Department of Health Statistics and Information - Ministry of Health of Chile) has the stillbirth records in Chile. The data can be found on the official DEIS-MINSAL website along with the description of the variables in the stillbirth record. All available years were collected. [18]
The population corresponded to stillbirth’s ≥ 22 gestational weeks, without criteria of inclusion and exclusion. The data that did not indicate the week of gestation were eliminated, as well as those that were unlikely to be within true limits for the typing of the gestational week.
The causes of stillbirth corresponded to 236 specific causes of death in fetuses ≥22 weeks for ICD-10, these causes were reclassified in macro-causes of death, according to the death mechanism , which corresponded to the clinical condition attributed to precise, possible etiology or probable. [19,20]
Those data in which the record of the cause of the fetal death has not been found, were recognized as "unknown". Fetal death was analyzed from the 22 gestational weeks, according to the WHO standard criteria. [19, 21]
The classification in macro-causes corresponds to type deaths: fetal, maternal, placental, infection, labor and delivery, and unknown, this according to criteria based on international studies, and validated by Chilean medical experts’ members of the National Obstetric Commission and Neonatal. [22]
One of the independent variables is gestational age that was divided into: 22-27, 28-34 and ≥35 weeks, by the relationship between gestational age and average fetal weight according to the Intrauterine Growth Curves Recommendation. [22, 23]
Other independent variables linked to perinatal health such as maternal and sociodemographic age such as: educational level, place of delivery and area of residence, can be identified as factors related to health inequities. [24]
Regarding the variable place of birth, it is defined as place of occurrence of death, such as the health center, the categories of house or room, and other places.
The frequency distribution and the proportion of the total fetal deaths according to macro-cause and specific cause of stillbirth were obtained, for a specific cause the first five of higher frequency were reported.
To determine the association between variables, the chi-squared (x2) test with statistical significance level p < 0.05 was used.
The highest percentage of stillbirth was recorded at 35 or more weeks (35.63%), followed by 28-34 weeks (32.91%) and finally at 22-27 weeks (31.44%).
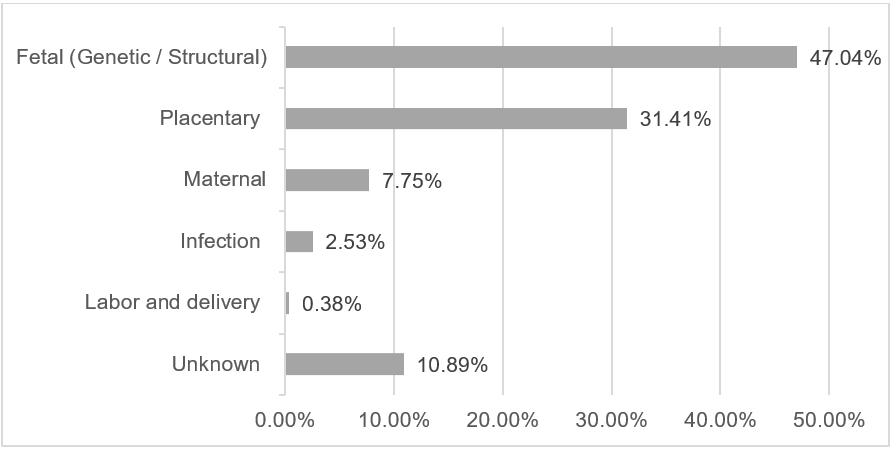
The fetal-type macro-cause is responsible for almost half of the total deaths (47%) and almost 1 in 3 stillbirths is involved in the placental-type macro-cause (31.4%) (Graphic 2).
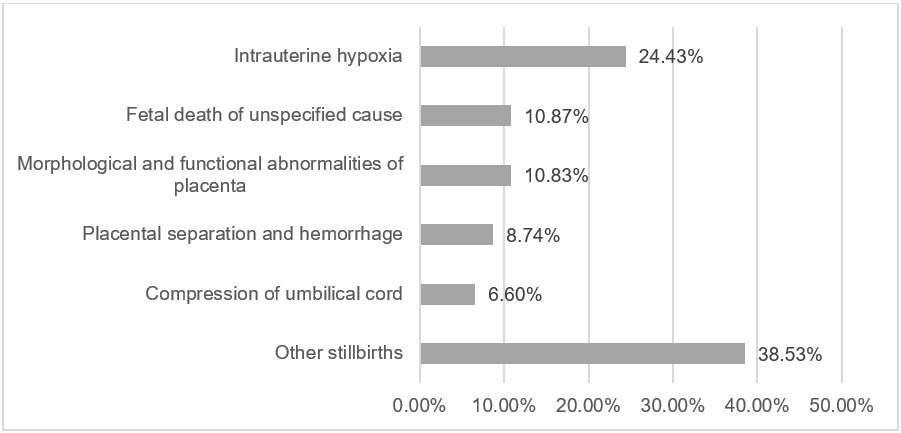
In specific causes, stillbirth due to intrauterine hypoxia is present in 24.4% of cases. More than 10% of total deaths are described as "unspecified" (Graphic 3).
In smaller percentages are the causes: maternal hypertensive disorders 5.06% (n=909); multiple congenital malformations 3.73% (n=669); premature rupture of membranes 2.31% (n=415) and chorioamnionitis 2.03% (n=364). Edwards syndrome is the most lethal of all the syndromes 1.61% (n=289) (Table 1).
| Ranking | Specific cause of stillbirth | N = 17.952 | % |
| 1 | Intrauterine hypoxia | 4,386 | 24.43 |
| 2 | Fetal death of unspecified cause | 1,951 | 10.87 |
| 3 | Morphological and functional abnormalities of placenta | 1.944 | 10.83 |
| 4 | Placental separation and hemorrhage | 1.570 | 8.74 |
| 5 | Compression of umbilical cord | 1,184 | 6.60 |
| 6 | Hypertensive disorders of the mother | 909 | 5.06 |
| 7 | Multiple congenital malformations | 669 | 3.73 |
| 8 | Premature rupture of the membranes | 415 | 2.31 |
| 9 | Chorioamnionitis | 364 | 2.03 |
| 10 | Hydrops fetalis not due to hemolytic disease | 323 | 1.80 |
| 11 | Other deaths | 4.237 | 23.59 |
Table 1: Distribution of the 10 most frequent causes of stillbirths.
The macro-causes of fetal type occur with greater frequency ending the pregnancy, in women of 40 or more years, delivery in hospitals and rurality. The maternal macro-cause occurs more frequently in gestational time 22 and 27 weeks, maternal age 30-39 years and delivery at home. The placental macro-cause is more frequent in the final weeks of pregnancy, maternal age 30 to 39 years and delivery at home. (Table 2).
| Variables | Macro cause of stillbirth* | ||||||
| Fetal | Placenta | Maternal | p value | ||||
| N | % | N | % | N | % | ||
| Gestational age | |||||||
| 22-27 weeks | 2.527 | 44,77 | 1,497 | 26.52 | 565 | 10.01 | <0.001 |
| 28-34 weeks | 2,818 | 47.69 | 1,894 | 32.05 | 506 | 8.56 | |
| ≥ 35 weeks | 3.100 | 48.45 | 2,247 | 35.12 | 320 | 5 , 00 | |
| Maternal age | |||||||
| ≤ 19 years | 1,196 | 48.07 | 735 | 29.54 | 154 | 6.19 | <0.001 |
| 20-29 years | 3,378 | 46,4 | 2.332 | 32.03 | 519 | 7.13 | |
| 30-39 years | 2,99 | 45.63 | 2.137 | 32.61 | 591 | 9.02 | |
| ≥ 40 years | 809 | 55.26 | 389 | 26.57 | 112 | 7.65 | |
| Unknown | 72 | 43.11 | 45 | 26.95 | 15 | 8.98 | |
| Maternal educational level | |||||||
| Basic or primary | 1,718 | 47.45 | 1,152 | 31.81 | 261 | 7.21 | 0.058 |
| Medium | 4.860 | 46.9 | 3.208 | 30.96 | 810 | 7.82 | |
| Higher | 1,755 | 47.54 | 1.192 | 32.29 | 297 | 8.04 | |
| None | 50 | 49.5 | 35 | 34.65 | 5 | 4.95 | |
| Unknown | 62 | 35,43 | 51 | 29,14 | 18 | 10.29 | |
| Place of birth | |||||||
| Hospital/Clinic | 8.199 | 47.57 | 5.427 | 31.49 | 1.325 | 7.69 | <0.001 |
| House/Room | 127 | 34.7 0 | 130 | 35.52 | 43 | 11.75 | |
| Other | 119 | 33.9 0 | 81 | 23.08 | 2. 3 | 6.55 | |
| Residence area | |||||||
| Urban | 6,953 | 47.17 | 4.595 | 31.18 | 1.105 | 7.5 0 | 0.003 |
| Rural | 791 | 49.41 | 496 | 30.98 | 140 | 8.74 | |
| Unknown | 701 | 43,49 | 547 | 33.93 | 146 | 9.06 | |
Table 2: Distribution of 3 most frequent macro-causes according to study variables.
*The 3 most frequent macro-causes are reported; the remaining percentage is equivalent to the rest of the stillbirths.
Statistical significance: p < 0.05.
*The 3 most frequent macro-causes are reported; the remaining percentage is equivalent to the rest of the stillbirths.
Statistical significance: p < 0.05.
The specific cause intrauterine hypoxia occurs more proportionally in pregnancies between 22 and 27 gestational weeks, maternal age less than 20 years, maternal educational level basic hospital delivery and rurality. The unspecified cause occurs more frequently between 22 and 27 gestational weeks and urbanity. The specific cause morphological-functional placental abnormalities are more frequent between 28 and 34 gestational weeks, maternal age greater than or equal to 40 years, home birth and rurality (Table 3).
| Variables | Specific cause of stillbirth* | ||||||
| Intrauterine hypoxia | Unspecified cause |
Morphological abnormalities placental |
p value | ||||
| N | % | N | % | N | % | ||
| Gestational age | |||||||
| 22-27 weeks | 1,254 | 42.02 | 747 | 25.03 | 472 | 15.82 | <0.001 |
| 28-34 weeks | 1,308 | 36.59 | 579 | 16,2 | 676 | 18.91 | |
| ≥ 35 weeks | 1,824 | 40.75 | 625 | 13.96 | 796 | 17.78 | |
| Maternal age | |||||||
| ≤ 19 years | 701 | 42.56 | 325 | 19.73 | 255 | 15.48 | <0.001 |
| 20-29 years | 1.873 | 40.20 | 836 | 17.94 | 814 | 17,47 | |
| 30-39 years | 1.470 | 37.95 | 640 | 16.52 | 717 | 18.51 | |
| ≥ 40 years | 308 | 40.53 | 124 | 16.32 | 141 | 18.55 | |
| Unknown | 3. 4 | 35.79 | 26 | 27.37 | 17 | 17.89 | |
| Maternal educational level | |||||||
| Basic or primary | 956 | 41.26 | 380 | 16.40 | 438 | 18.9 | <0.001 |
| Medium | 2,656 | 40.59 | 1,198 | 18.31 | 1.122 | 17,15 | |
| Higher | 718 | 35.85 | 329 | 16.43 | 356 | 17.77 | |
| None | 27 | 39.71 | 9 | 13.24 | 13 | 19.12 | |
| Unknown | 29 | 28.16 | 35 | 33.98 | 15 | 14.56 | |
| Place of birth | |||||||
| Hospital/Clinic | 4.237 | 40.25 | 1,775 | 16.86 | 1,857 | 17.64 | 0.059 |
| House/Room | 79 | 30.98 | 58 | 22.75 | 55 | 21.57 | |
| Other | 70 | 27.67 | 118 | 46.64 | 32 | 12.65 | |
| Residence area | |||||||
| Urban | 3.599 | 39.67 | 1,641 | 18.09 | 1.569 | 17,29 | 0.620 |
| Rural | 404 | 42,71 | 129 | 13.64 | 181 | 19,13 | |
| Unknown | 383 | 37.70 | 181 | 17.81 | 194 | 19,09 | |
Table 3: Distribution of 5 most frequent specific uses according to variables.
*The first 3 most frequent specific causes are reported; the remaining percentage equals the rest of stillbirths.
Statistical significance: p < 0.05.
*The first 3 most frequent specific causes are reported; the remaining percentage equals the rest of stillbirths.
Statistical significance: p < 0.05.
The association between macro-cause fetal type was significant with gestational age, maternal age, place of delivery and area of residence (p < 0.05). For specific cause intrauterine hypoxia there is a significant association with gestational age, maternal age and maternal educational level (p < 0.05).
Discussion
Prenatal health and the analysis of stillbirth is relevant in member countries of the Organization for Economic Cooperation and Development (OECD), as well as in developing countries because it reflects obstetric care, quality and health progress. [25]
The worldwide trend of stillbirth rates is decreasing and more noticeably in developed countries. The effect of mortality on the economy and future society indicates the need for actions in the prevention of stillbirths. Stillbirth is one of the epidemiological problems that having low rates could contribute significantly to the creation and formation of healthy nations. [26]
The results of this study are a diagnostic approach that could help the prevention of a new lethal fetal event through reproductive counselling, prenatal care and adequate approach in the new pregnancy. In addition to preventing the psychosocial morbidity of those involved and who are also victims of this event, precisely emotional support interventions are extremely important, and health systems must respond to this need. [27]
While Chile advances in clinical records and databases, there are still problems in the quality of these. Potentially there is low rigor in the assignment of the cause of stillbirth, because the death options are 236, with wide classification segments, low detection tools and weak research. [9]
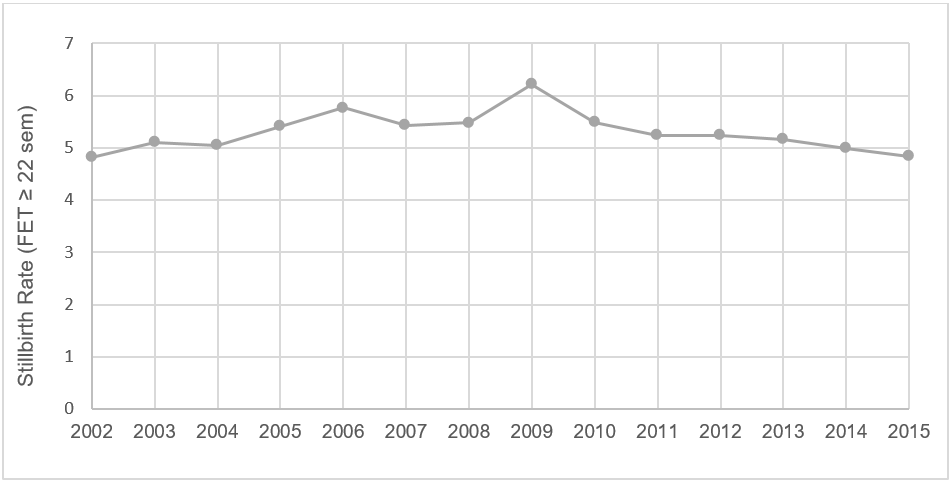
The annual rate of stillbirth in the world is reduced, in Chile it increased slightly in the 2002-2015 perspective. But in the micro analysis, there were years in which the maximum recommended rate was far exceeded and stayed away from indicators of high-income countries and the OECD average. [19]
In the proper analysis of the causes, the results of this research coincide with the international literature. The mechanisms of fetal and placental death are more dangerous as pregnancy progresses, while maternal and infectious macro-causes are not as relevant in peri-term fetuses. There is direct proportionality in the triad: placental anomalies, gestational advancement and stillbirth in the second-third trimester. [28]
The greater the maternal age, the maternal and fetal macro-causes increase. The group of pregnant women that includes women under or equal to 19 to 29 years old is characterized by an increase in the number of stillbirths and of all macro-causes of death. At higher maternal educational level, more stillbirths occur due to macro-cause such as fetal, maternal, placental and infection. At higher maternal age, stillbirths increase due to macro-fetal type, maternal and unknown, decreasing for placental, infection, labor and delivery.
Stillbirths in labor and delivery are due to problems of coverage, quality and equity in delivery care. This constituent can be reduced initially with quality health care in most pregnancies.
As the pregnancy progresses, the number of stillbirths increases due to intrauterine hypoxia, morphological and functional placental anomaly, detachment and placental hemorrhage, and compression of the umbilical cord.
There is potentially low stringency in the assignment of cause of stillbirth, ICD-10 offers 236 stillbirth options, with broad classification segments and does not capture significant fetal and placental categories. About 11% of stillbirths are attributed a stale cause and it is surprising that 1 in 4 stillbirths die from intrauterine hypoxia without more definite detail. The inscription of unspecified cause could be a consequence of lack of experience of the evaluator or insufficient elements to establish causality and hypoxia to low quality of information, as a result unproductive death certificates are obtained. [28]
There may be an over diagnosis of the unspecified cause and intrauterine hypoxia. To decrease the disproportionate labeling of unspecified causes to determine the cause, it is necessary to intervene with: fetal karyotype tests, total body radiography, placental histopathology, maternal tests of hereditary thrombophilia’s, TORCH profile and Parvovirus infection, thyroid hormones, Coombs indirect and genital culture. [28]
The unspecified cause has fewer meanings as the term approaches, the hypothesis is that at this stage of pregnancy the biological certainty of death increases, or the evaluator is more engaged in investigating cause of death in older fetuses.
Different obstetric societies advise delivery assistance in health centers. In Chile, public policies recommend institutionalized birth. The Netherlands, a pro-freedom country, choice of delivery, with 28% of home births, has the highest rate of stillbirths (10 stillbirths per 1,000 live births) compared to developed countries, considering that in other countries similar economically the rate is 30% less. It can be a problem of financial protection, since in most OECD countries, delivery to a public hospital is free, but not in the Netherlands. [29]
It is necessary to add variables to the registry of stillbirths that incorporate temporal, biological and social components of the mother, for example: intrapartum/antepartum death , since most of the intrapartum stillbirths are preventable, in addition to prenatal control number, null parity, intergenic period, attention in public/private sector, chronic no communicable maternal diseases, consumption of substances in pregnancy, body mass index, ethnicity, socioeconomic level and maternal nationality. [25, 28, 30]
High income countries seek to eliminate avoidable stillbirths by monitoring their indicators of coverage, prenatal care and health promotion, closing gaps of inequity and preventing risk factors in prenatal care. The possibility of reducing the stillbirth rate with quality health care is demonstrable. [25, 31,32,33,34]
The limitations of this study are the weakness of the electronic registry in Chile and the amount of data recognized as unknown. In addition, the weak knowledge of the cases prevents addressing the stillbirth from the purely biological variables in the approach to risk assessment.
Conclusions
The stillbirth rate remained less stable at the time of study, only fetal and unknown macro-causes were the only ones that increased. Stillbirths in the third trimester reflected the highest incidences and the fetal type macro-cause is the strongest responsible for the stillbirth in Chile.
Specifically, stillbirths due to intrauterine hypoxia are present in almost 1 in 4 stillbirths. There is a significant gap of stillbirths in which cause of death is not specified, being more frequent between 22-27 gestational weeks.
The association between macro-cause fetal types was significant with gestational age, maternal age, and place of delivery and area ofresidence. For intrauterine hypoxia there is association with gestational age, maternal age and maternal educational level.
Recommendations
It is necessary to improve the data collection system with a standardized classification system, since the estimates of causality in stillbirth are hampered for this reason, since the reality of death is unknown and makes the design of strategies difficult.
It is necessary to improve the data collection system with a standardized classification system, since the estimates of causality in stillbirth are hampered for this reason, since the reality of death is unknown and makes the design of strategies difficult.
From the promotional point of view, it is effective to maintain normal nutritional status and prevent diabetes, hypertension and smoking, in addition to implementing updated guidelines reinforcing clinical practices and perinatal audits, the latter is very useful in identifying underlying causes of stillbirth.
The knowledge of the current situation favors the preventive aspects in term gestational weeks and the need to improve the biopsychosocial registry of each stillborn. Future research in the field of stillbirth should assess the risk of home birth in circumstances of complete normality of the maternal-fetal axis, versus the hospital center.
Finally, the decrease in the stillbirth rate will be possible when the research is improved, with standardization of specialists, cross-section of clinical audits and a convenient classification of causes.
References
- Reinebrant H., et al. (2017). Making stillbirths visible: a systematic review of globally reported causes of stillbirth. BJOG: An International Journal of Obstetrics & Gynaecology 125 (2):212–224.
- Gopichandran V., et al. (2018). Psycho-social impact of stillbirths on women and their families in Tamil Nadu, India – a qualitative study. BMC Pregnancy and Childbirth 18(1).
- de Bernis L, Kinney MV, Stones W, ten Hoope-Bender P, Vivio D, Leisher SH, et al. (2016). Stillbirths: ending preventable deaths by 2030. The Lancet 387(10019): 703–16.
- Pásztor N, Keresztúri A, Kozinszky Z, Pál A. (2013). Identification of Causes of Stillbirth through Autopsy and Placental Examination Reports. Fetal and Pediatric Pathology 33(1): 49–54.
- Pons A, Sepúlveda E, Leiva JL, Rencoret G, Germain A. (2014). Muerte fetal. REV MED CLIN CONDES 25(6): 908–16.
- Chen K, Seow K, Chen L. (2015).The role of preterm placental calcification on assessing risks of stillbirth. Elsevier 36(9): 1039–44.
- WHO: World Health Organization [Internet]. Geneve: WHO; c2016 [cited: 29/08/2018] True magnitude of stillbirths and maternal and neonatal deaths underreported.
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. (2016). Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 387 (10018): 587–603.
- Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. (2011). Stillbirths: Where? When? Why? How to make the data count? Lancet 377(9775):1448–63.
- Tilahun D, Assefa T. (2017). Incidence and determinants of stillbirth among women who gave birth in Jimma University specialized hospital, Ethiopia. PanAfrican Medican J 8688: 1–11.
- WHO: World Health Organization. [Internet]. Geneve: WHO; c2016 [cited: 29/08/2018] Making every baby count: audit and review of stillbirths and neonatal deaths.
- Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. (2011). Major risk factors for stillbirth in high-income countries: A systematic review and meta-analysis. Lancet 377(9774): 1331–40.
- Akseer N, Lawn JE, Keenan W, Konstantopoulos A, Cooper P, Ismail Z, et al. (2015). Ending preventable newborn deaths in a generation. International Journal of Gynecology & Obstetrics 131: S43–8.
- de Bernis L, Kinney M V, Stones W, ten Hoope-Bender P, Vivio D, Leisher SH, et al. (2016). Stillbirths: ending preventable deaths by 2030. Lancet 387(10019): 703–16.
- Frøen JF, Friberg IK, Lawn JE, Bhutta ZA, Pattinson RC, Allanson ER, et al. (2016). Stillbirths: progress and unfinished business. The Lancet 387(10018): 574–86.
- The Stillbirth Collaborative Research Network Writing Group. Causes of Death among Stillbirths. Jama (2011). 306(22): 2459–68.
- Ramonien? G, Maleckien? L, Nadišauskien? RJ, Bartusevi?ien? E, Railait? DR, Ma?iulevi?ien? R, et al. (2017). Maternal obesity and obstetric outcomes in a tertiary referral center. Medicina 53(2):109–13.
- MINSAL: Ministerio de Salud de Chile. Bases de datos defunciones fetales [Internet]. DEIS: Departamento de estadísticas e información de salud. 2018.
- Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, van den Broek N. (2014). Causes of and factors associated with stillbirth in low- and middle-income countries: a systematic literature review. BJOG: An International Journal of Obstetrics & Gynaecology 121: 141–53.
- Goldenberg RL, McClure EM, Bhutta ZA, Belizán JM, Reddy UM, Rubens CE, et al. (2011). Stillbirths: the vision for 2020. The Lancet 377 (9779):1798–805.
- Frøen JF, Cacciatore J, McClure EM, Kuti O, Jokhio AH, Islam M, et al. (2011). Stillbirths: why they matter. The Lancet 377 (9774):1353–66.
- MINSAL: Ministerio de Salud de Chile [Internet]. Santiago MINSAL; c2015 [citado: 26/10/2017] Guía Perinatal 1-466.
- Milad A M, Novoa P JM, Fabre B J, Samané M MM, Aspillaga M C. (2010). Recomendación sobre Curvas de Crecimiento Intrauterino. Revista Chilena de Pediatría 81(3).
- Ministerio de Sanidad Servicios Sociales e Igualdad. Avanzando hacia la equidad. Propuesta de políticas e intervenciones para reducir las desigualdades sociales en salud en España. Inf Estud e Investig (2015).
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. (2016). Stillbirths: rates, risk factors, and acceleration towards 2030. The Lancet 387 (10018): 587–603.
- Social Trends Institute. The Sustainable Demographic Dividend. (2010).
- McNamara K, Meaney S, O’Donoghue K. (2018). Intrapartum fetal death and doctors: a qualitative exploration. Acta Obstetricia et Gynecologica Scandinavica 97(7): 890–8.
- ANZSA (Coordinating Centre). Investigating the causes of stillbirth?; a prospective cohort study examining use and effectiveness of a comprehensive investigation protocol [Internet]. South Brisbane: ANZSA Coordinating Centre Mater Medical Research Institute Raymond; (2013).
- Darmstadt GL, Shiffman J, Lawn JE. (2015). Advancing the newborn and stillbirth global agenda: priorities for the next decade. Archives of Disease in Childhood 100 (Suppl 1): S13–8.
- Lakew D, Tesfaye D, Mekonnen H. (2017). Determinants of stillbirth among women deliveries at Amhara region, Ethiopia. BMC Pregnancy and Childbirth 17(1).
- Leisher SH, Teoh Z, Reinebrant H, Allanson E, Blencowe H, Erwich JJ, et al. (2016 ). Seeking order amidst chaos: a systematic review of classification systems for causes of stillbirth and neonatal death, 2009–2014. BMC Pregnancy and Childbirth 16(1).
- Pásztor N, Keresztúri A, Kozinszky Z, Pál A. (2014). Identification of Causes of Stillbirth through Autopsy and Placental Examination Reports. Fetal Pediatr Pathol 33(1): 49–54.
- Thorsten V, Dudley D, Parker C, Koch M, Hogue C, Stoll B, et al. (2018). Stillbirth, Inflammatory Markers, and Obesity: Results from the Stillbirth Collaborative Research Network. American Journal of Perinatology 35(11): 1071–8.
- Lehner C, Harry A, Pelecanos A, Wilson L, Pink K, Sekar R. (2018). The feasibility of a clinical audit tool to investigate stillbirth in Australia - a single centre experience. Australian and New Zealand Journal of Obstetrics and Gynaecology 59 (1): 59–65.
Citation: David San Martín Roldán. (2019). Distribution of Stillbirth Causes in Chile between Years 2002-2015. Journal of Medical Research and Case Reports 1(1).
Copyright: © 2019 David San Martín Roldán. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.