Case Report
Volume 3 Issue 1 - 2021
Disequilibrium double-whammy: A case of concurrent BPPV and cerebellar stroke
1Neurology Department, Liverpool Hospital, Liverpool 2170, NSW, Australia
2Conjoint Professor, South Western Clinical School, University of NSW, Sydney, NSW, Australia
3Professor, Griffith University, Southport, Qld, Australia
4Professor, Chair, Sechenov Moscow First State University, Moscow, Russia
2Conjoint Professor, South Western Clinical School, University of NSW, Sydney, NSW, Australia
3Professor, Griffith University, Southport, Qld, Australia
4Professor, Chair, Sechenov Moscow First State University, Moscow, Russia
*Corresponding Author: Prof Roy G Beran, PO Box 598, Northbridge, NSW 1560, Australia.
Received: May 13, 2021; Published: May 26, 2021
Abstract
Introduction: Benign paroxysmal positional vertigo (BPPV) and cerebellar stroke can both present with vertigo. They are not commonly described to occur simultaneously, although BPPV remains an independent risk factor for ischaemic strokes. This paper reports a patient presenting with classical BPPV shown to have cerebellar infarction.
Case Report: A 50 year old man, presenting with vertigo was diagnosed with BPPV, following clinical examination, Semont manoeuvre, Dix-Hallpike’s manoeuvre and Brandt Daroff exercise/ procedure. Magnetic Resonance Imaging demonstrated acute cerebellar infarctions, on a background of multiple vascular risk factors, suggesting these presented as BPPV.
Discussion: BPPV, non-sustained vertigo triggered by changes in head position, is produced by irritation of the cupula of semicircular canals by calcium carbonate deposits. Both BPPV and posterior circulation infarctions cause vertigo, with BPPV being an independent risk for ischaemic strokes. BPPV led to the presentation but investigation confirmed concurrent diagnosis of acute cerebellar infarctions. He responded to Brandt Daroff exercises and was asymptomatic at discharge. Assuming the BPPV was the presentation of the stroke, suggesting a central cause thereof, the underlying pathophysiology of the BPPV remains obscure. The alternative explanation is that the case represents a propicious, coincidental occurrence of both diagnoses. He subsequently suffered further ischaemic stroke, due to an underlying clopidogrel resistance, and suffered significant morbidity as a result. Patients presenting with clinical diagnosis of BPPV rarely undergo screening for stroke, especially affecting the posterior circulation, potentially explaining the paucity of data regarding concurrent BPPV and cerebellar strokes.
Conclusions: Posterior-circulation stroke should be considered in patients presenting with BPPV symptoms.
Keywords: Positional Vertigo; Cerebellar Stroke; Unexpected Presentation
Introduction
Benign paroxysmal positional vertigo (BPPV) and cerebellar stroke can both present with vertiginous attacks [1]. These two conditions are rarely described to occur simultaneously, although BPPV remains an independent risk factor for ischaemic strokes [1-5]. This paper presents the fourth report of a case of a patient who presented with the classical features of BPPV in whom Computer Tomography (CT) and subsequent Magnetic Resonance Imaging (MRI) demonstrated acute cerebellar infarction in whom BPPV was the presenting feature of the stroke.
Case
A 50 year old man, Mr A, presented to Liverpool Hospital with a one day history of ataxia preceded by one week history of intermittent positional vertigo, especially in bed when turning to the left. His past medical history included type 2 diabetes mellitus (Hba1C 7.7%), hypertension (normotensive at admission) and dyslipidaemia (normal lipid studies at admission with the patient on statins). His National Institute of Health Stroke Scale (NIHSS) score, at presentation, was 0, making expectation of stroke unlikely. On examination, the patient had a positive Semont’s manoeuvre and Dix-Hallpike’s manoeuvre, with nystagmus towards left, which was successfully corrected with three repetitions of Brandt Daroff exercises [6-8]. A CT perfusion series showed a probable right hemisphere perfusion mismatch, possibly secondary to occlusion of the right Posterior Inferior Cerebellar Artery (PICA). MRI of the brain, performed subsequently, showed several small focal areas of restricted diffusion bilaterally in the posterior inferior cerebellum consistent with acute infarcts (Figure 1). The patient’s vertigo resolved following the Brandt Daroff exercises and he was commmenced on dual anti-platelet therapy of clopidogrel (75mg daily) and Aspirin (100mg daily) following intial loading dose of 300mg each respectively, based on the MRI findings. Trans-thoracic echocardiogram performed, to investigate cardio-embolic source of emboli, was unremarkable. The patient was discharged home following return to baseline fuctional status.
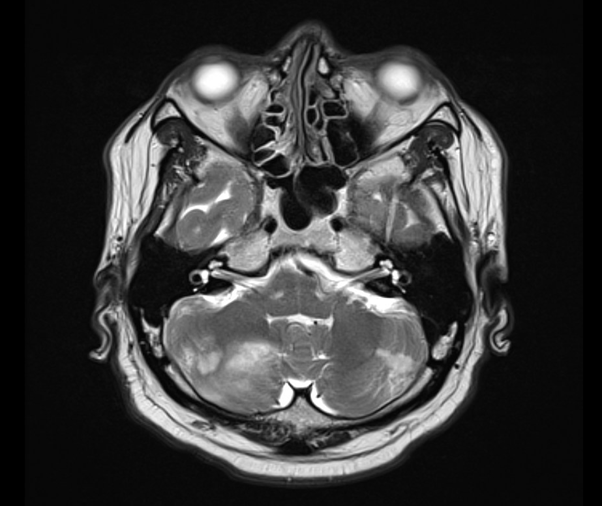
Image 1: T2 weighted image of cerebellar hemispheres from patient’s first presentation showing bilateral acute and subacute infarcts.
Mr A represented to Liverpool Hospital, three days following previous admission, with ataxia and disequilibirum and a NIHSS score of 4 (secondary to dysarthia, upper limb ataxia and partial gaze palsy). He presented outside the window for either thrmobolysis or endo-vascular clot retrieval and was conservatively managed. He did not have any symptoms of BPPV during the second presentation. A CT perfusion study of the brain identified a new left cerebellar hemisphere infact, in addition to mismatches from his previous admission. This was confirmed with a subsequent MRI of the brain(Figure 2). Multiple electrode aggregometry (Multiplate Analyser®, Roche diagnostics) test for platelet function revealed resistance to clopidogrel, and Mr A’s clopidogral therapy was replaced with ticagrelor 90mg BD following a loading dose of 180mg. Mr A was subsequently discharged to a rehabiliation facility.
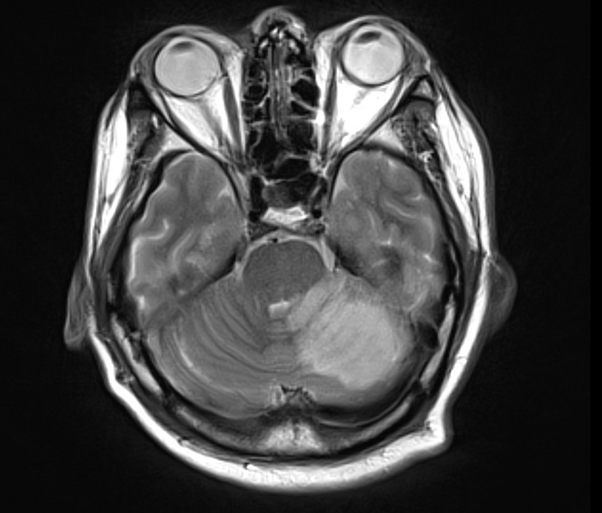
Image 2: T2 weighted MRI of cerebellar hemispheres from patient’s second presentation showing an acute left cerebellar hemisphere infarction.
Discussion
BPPV is defined as intermittent episodes of non-sustained vertigo triggered by changes in head position relative to gravity [2]. Vertiginous symptoms in this condition are produced by irritation of the cupula of semicircular canals by calcium carbonate otoliths. Both BPPV and posterior circulation infarctions are known causes of vertigo, with BPPV being significantly more prevalent [9]. BPPV has also been identified as an independent risk factor for ischaemic strokes [1]. Positional nystagmus, caused by a central lesion, is described in the literature with the majority of these being due to cerebellar involvement [9]. Central positional nystagmus is unlikely to respond to interventions, such as Brandt Daroff exercises. It was Mr A’s vertigo, with classical features of BPPV, which led to his presentation to hospital, but, upon investigation, he was confirmed to have a concurrent diagnosis of acute cerebellar infarctions. His vertigo symptoms responded favourably to Brandt Daroff exercises and he was symptom free two days following first admission. Assuming that the BPPV, as clinically confirmed, was the presenting feature of his cerebellar strokes, the underlying pathophysiology of the BPPV remains unclear as it would suggest a central cause thereof. With a potential central cause for the BPPV, it is difficult to explain how it fully resolved, once he underwent the Brandt Daroff maneouvre, acknowledging the accepted pathophysiology for BPPV. The alternative explanation is that of an unexpected propicious, coincidental occurrence of both diagnoses in a patient for whom the symptoms of BPPV domiated the clinical picture but led to further investigation to reveal the strokes. He subsequently suffered a further ischaemic stroke, due to an underlying clopidogrel resistance, and suffered significant morbidity as a result.
A review of literature shows that these two conditions are rarely reported to occur simultaneously [2-4, 10]. Patients presenting with BPPV rarely undergo screening for cerebro-vascular accidents (CVA), especially affecting the posterior circulation, potentially explaining the paucity of data regarding concurrent BPPV and cerebellar strokes. This case, to the best of our knowledge, represents the fourth such presentation to be reported in the literature and, raises concern regarding the need for further investigation of those who present with BPPV, to look for subclinical stroke. In their review, Nelson et al suggested that four signs, viz. focal neurological deficits, total ipsilateral hearing loss, inability to walk unaided and positional nystagmus should be considered as red flags for cerebellar stroke, in patients presenting with vertigo [11]. Patients presenting with any of these signs should undergo further imaging, to rule out posterior circulation strokes, acknowledging that the only such feature, seen in the current case, was that of positional nystagmus which was diagnosed as BPPV, on the basis of clinical examination and response to standard, conservative intervention, applying the Brandt Daroff maneouvre.
Conclusion
This paper reports a further case of BPPV shown to have concurrent cerebellar hemisphere infarction. The presence of vascular risk factors, prompted parallel investigations for a CVA while managing the BPPV. The resultant diagnosis of two different pathologies highlights the need for a broader approach to vertiginous patients. It is imperative that appropriate history taking and examination, for other causes of disequilibrium, be extended to patients presenting with BPPV, to look for posterior circulation strokes.
References
- Kao CL, Cheng YY, Leu HB, et al. (2014). Increased risk of ischemic stroke in patients with benign paroxysmal positional vertigo: a 9-year follow-up nationwide population study in taiwan. Front Aging Neurosci. 6:108.
- Chen J, Zhao W, Yue X, et al. (2020). Risk Factors for the Occurrence of Benign Paroxysmal Positional Vertigo: A Systematic Review and Meta-Analysis. Front Neurol. 11:506.
- Volgger, V., Gürkov, R. (2017). Acute vestibular syndrome in cerebellar stroke. HNO 65:149–52.
- Hesselbrock RR. (2017). Cerebellar Infarction Presenting with Acute Vestibular Syndrome in Two U.S. Air Force Pilots. Aerosp Med Hum Perform. 88(9):880-883.
- Sakata E, Ohtsu K, Shimura H, et al. (1987). Positional nystagmus of benign paroxysmal type (BPPN) due to cerebellar vermis lesions. Pseudo-BPPN. Auris Nasus Larynx. 14(1):17-21.
- Teo SP. (2015). Semont manoeuvre for vertigo assessment. Aust Fam Physician. 44(7):471-3.
- Talmud JD, Coffey R, Edemekong PF. Dix Hallpike Maneuver. [Updated 2020 Sep 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
- Gupta, A.K., Sharma, K.G. & Sharma, P. (2019). Effect of Epley, Semont Maneuvers and Brandt–Daroff Exercise on Quality of Life in Patients with Posterior Semicircular Canal Benign Paroxysmal Positional Vertigo (PSCBPPV). Indian J Otolaryngol Head Neck Surg 71: 99–103.
- Saber Tehrani AS, Coughlan D, et al. (2013). Rising annual costs of dizziness presentations to U.S. emergency departments. Acad Emerg Med. 7:689-96.
- Macdonald NK, Kaski D, Saman Y, et al. (2017). Central Positional Nystagmus: A Systematic Literature Review. Front Neurol. 8:141.
- Nelson JA, Viirre E. (2009). The clinical differentiation of cerebellar infarction from common vertigo syndromes. West J Emerg Med. 10(4):273-77.
Citation: Namraj Goire and Roy G Beran. (2021). Disequilibrium double-whammy: A case of concurrent BPPV and cerebellar stroke. Journal of Brain and Neurological Disorders 3(1). DOI: 10.5281/zenodo.4895715
Copyright: © 2021 Roy G Beran. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
