Research Article
Volume 1 Issue 1 - 2019
Conservative & Physical therapy vs Corticosteroid therapy vs Percutaneous Needling with Autologous Platelet Rich Plasma therapy for de Quervain’s Stenosing Tenosynovitis in a Tertiary Care Hospital
1Professor, Department of Orthopaedics, JJM Medical College, Davangere
2Junior Resident, Department of Orthopaedics, JJM Medical College, Davangere
3Assistant Professor, Department of Community Medicine, SSSMCRI, Kancheepuram
2Junior Resident, Department of Orthopaedics, JJM Medical College, Davangere
3Assistant Professor, Department of Community Medicine, SSSMCRI, Kancheepuram
*Corresponding Author: Madhan Jeyaraman, Junior Resident, Department of Orthopedics JJM Medical College, Davangere, Karnataka, India.
Received: January 22, 2019; Published: January 30, 2019
Abstract
Background: de Quervain’s stenosing tenosynovitis (dQSTS) is a tenosynovial disorder which is characterized by impaired gliding of the tendons of the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) muscles over the tendon sheath covering these tendons. The most sensitive clinical test to diagnose dQSTS is Finkelstein's manoeuvre. The management of the disease differs based on the severity of the condition.
Objectives: To prospectively review and compare the efficacy, feasibility and durability of conservative & physical therapy, corticosteroid therapy and platelet rich plasma therapy in the view of (1) symptomatic pain relief, (2) improved the visual analogue scale (VAS) score and functional Mayo’s wrist scores, (3) durability of treatment given and (4) alleviation of need of surgery in patients with de Quervain’s tenosynovitis.
Materials and Methods: After screening of cases, 217 cases entered into the study and the cases were randomized into three groups according to our study protocol. Group a cases were treated with conservative & physical therapy, Group B cases were treated with corticosteroid therapy and Group C cases were treated with autologous platelet rich plasma injection with due pre and post procedural care. The cases were followed up on day 0, at the end of 1st week, 1st and 6th month for pain and range of movements. The patients were followed up for complications and the data were analysed statistically.
Results: A total of 25 (30.06%) cases in group A, 48 (69.56%) cases in group B and 64 (95.52%) cases in group C had recovered from disease at the end of 2nd dose of treatment. At the end of 6th month follow up, a total of 39 (60.93%) cases in group A, 21 (30.43%) cases in group B and 3 (4.47%) cases in group C had recurrence. All these patients were followed up for 1 year which showed a statistical difference with P value of <0.001 in VAS score and 0.001 in Mayo’s wrist scores among all three groups. No adverse reactions and serious complications are noted in the study participants.
Conclusion: Percutaneous needling with autologous PRP injection is the superior modality for de Quervain’s tenosynovitis which minimise the pain and improve the functional quality of life.
Keywords: Platelet rich plasma; de Quervain's stenosing tenosynovitis; Corticosteroid; Percutaneous needling
Introduction
de Quervain’s stenosing tenosynovitis (dQSTS) is a tenosynovial disorder which is characterized by wrist pain and tenderness at the radial styloid [1]. Tensoynovitis is due to impaired gliding of the tendons of the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) muscles over the tendon sheath covering these tendons. The resultant impaired gliding is due the thickening of the extensor retinaculum at the first extensor compartment of the wrist, with subsequent narrowing at the fibro-osseous canal [2].
The tern “tenosynovitis” is a misnomer in this clinical condition. The pathophysiology implies the degenerative process of extensor retinaculum [3]. Histological features suggest fibrocartilaginous metaplasia, deposition of mucopolysaccharide, neovascularization and neoinnervation which transmits pain and nociception [4].
The highest prevalence of dQSTS has been reported among subjects 30–55 years of age without any sex predilection. The most sensitive clinical test to diagnose dQSTS is Finkelstein manoeuvre [5]. The management of the disease differs based on the severity of the condition. The available modalities of include PRICE regimen, anti-inflammatory medication, corticosteroid injections, injections, occupational therapy (OT), physical therapy in the form of ultrasound therapy and interferential therapy, biological therapy and surgical release of first extensor compartment.
Objectives
The purpose of this study was to prospectively review and compare the efficacy, feasibility and durability of conservative & physical therapy, corticosteroid therapy and percutaneous needling with autologous platelet rich plasma therapy in patients with de Quervain's tenosynovitis in the view of
The purpose of this study was to prospectively review and compare the efficacy, feasibility and durability of conservative & physical therapy, corticosteroid therapy and percutaneous needling with autologous platelet rich plasma therapy in patients with de Quervain's tenosynovitis in the view of
- Symptomatic pain relief,
- Improved the visual analogue scale (VAS) score and functional Mayo’s wrist scores,
- Durability of treatment given and
- Alleviation of need of surgery.
Materials and Methods
- Health care setup – Tertiary care hospital
- Setting – JJM Medical College, Davangere, Karnataka.
- Duration of the study – September 2016 to August 2018
- Type of the study – Prospective cohort study
- Level of evidence – Level IV
- Sample size – 267
- Sampling technique – Convenient sampling
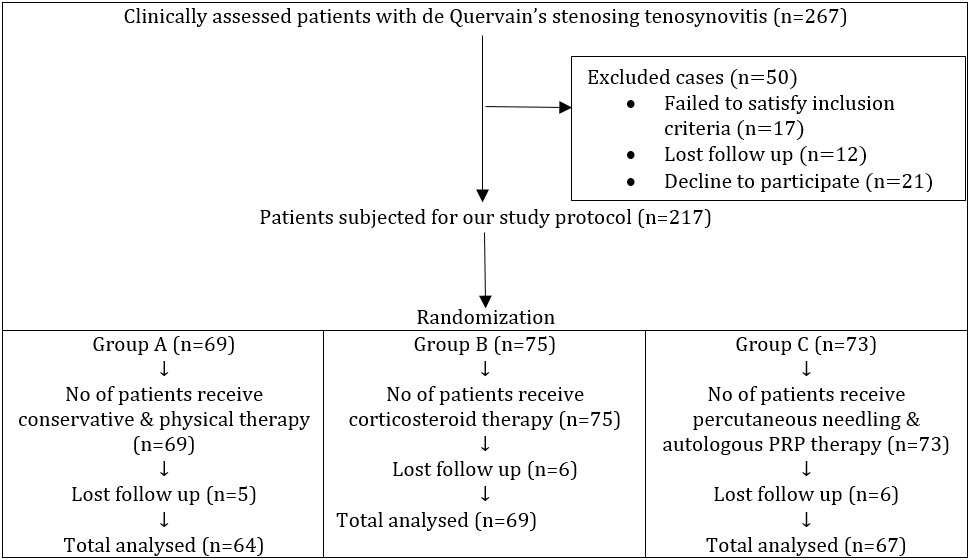
- Selection of cases – Among 267 de Quervain’s tenosynovitis cases, 17 cases failed to satisfy the inclusion criteria, 12 cases lost follow up and 21 cases declined to participate the study. The remaining 217 cases were taken up for this study who were randomized into three groups namely a) Group A (n=69) who receive physical therapy and conservative management, b) Group B (n=75) who receive corticosteroid injection and c) Group C (n=73) who receive percutaneous needling with autologous platelet rich plasma injection as per our study protocol. A total of 17 cases lost follow up post procedure. So, 200 cases were taken into consideration for statistical analysis.
Inclusion criteria
- Patients with de Quervain’s tenosynovitis who have taken conservative treatment but have shown no improvement from past 6 months
- Patients with recalcitrant de Quervain’s tenosynovitis with no improvement from past 6 months
- Patients with physical therapy and orthotic splintting with no improvement from past 6 months
- Patients with swelling over first extensor compartment of the hand from past 3 months
- Patients with positive Finkelstein’s test
- Patients who gave consent for treatment with autologous PRP injection as per our protocol
- Regular visits in the out-patient department
Exclusion criteria
- Patients with haemoglobin < 10 gm/dL and platelet count < 105 / μL
- Patients with usage of analgesics prior to 72 hours of PRP therapy
- Patients with corticosteroid injection at treatment site within 1 month
- Patients who underwent surgical treatment for de Quervain’s tenosynovitis
- Patients with rheumatoid arthritis, gouty arthritis, seronegative arthropathies and reactive arthritis
- Patients with local infection at the site of the procedure, HIV, Hepatitis B or C, coagulation and bleeding disorders, septicaemia and other systemic disorders
- Patients refusal for PRP treatment as per our protocol
After getting IEC clearance and informed written consent from the patients enrolled in our study, the cases were subjected for thorough clinical examination and to investigate the duration of the disease and the nature of management taken prior to the study. The baseline investigations and radiographic analysis such as plain x ray and ultrasound examination of the affected wrists were analysed. All the cases are investigated for the usage of NSAIDs 72 hour’s prior and local steroid infiltration 4 weeks prior to autologous PRP injection.
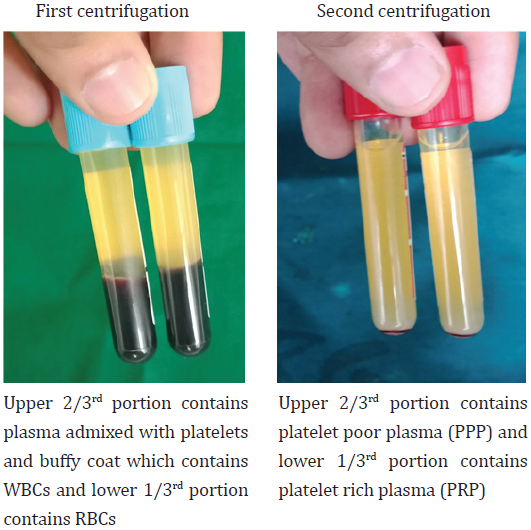
Preparation of platelet rich plasma 20 cc of venous blood were withdrawn into vacutainers containing sodium citrate and were subjected first centrifugation at a rate of 3000 rpm for 15 minutes. Then the resultant plasma admixed with platelets were transferred into plain vacutainer which were subjected for second centrifugation at a rate of 5000 rpm for 15 minutes. The resultant solution in the vacutainer contain upper 2/3rd portion of platelet poor plasma and lower 1/3rd portion of platelet rich plasma. 20 ml of autologous venous blood yield 3 – 4 ml of autologous platelet rich plasma solution. Before injecting autologous PRP injection, 10% of calcium chloride solution was added to autologous PRP in the ratio of 1:10.
Modalities of treatment instituted
Group A cases (n=69) were given conservative therapy in the form of rest, ice pack application, analgesics and anti edema measures for 2 weeks and physical therapy in the form of ultrasonic therapy and soft tissue massage.
Group A cases (n=69) were given conservative therapy in the form of rest, ice pack application, analgesics and anti edema measures for 2 weeks and physical therapy in the form of ultrasonic therapy and soft tissue massage.
Group B cases (n=75) were given single dose of 40 mg of triamcinolone infiltration around the inflamed tendon sheath of APL and EPB tendons. The patients, who reported no pain relief, were offered 2nd dose of steroid infiltration with an interval of 4 weeks.
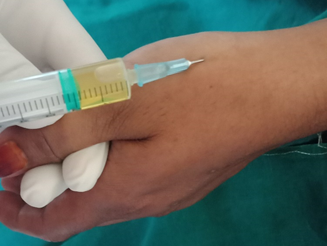
Group C cases (n=73) were treated with percutaneous needling with 3 – 4 ml of autologous platelet rich plasma injection along the inflamed tendon sheath of APL and EPB tendons. The sterile dressing and crepe bandage were applied at the injection site. The patients, who reported no pain relief, were offered 2nd dose of PRP injection with an interval of 4 weeks as it provide time for collagen production.
All patients were advised for resting the affected wrist with thumb spica splint for 24 to 48 hours post injection. The patients were trained for home based wrist exercises. All the patients were reviewed according to the study protocol.
All the patients were advised not to perform repetitive movements over affected wrist for minimum of 2 weeks and the pain was combated with paracetamol and ice pack application. The functional status and severity of pain around the wrist joint were charted according to VAS and Mayo’s wrist score both pre-procedurally on day 0 and post-procedurally at the end of 1st week, 1st and 6th month. All the cases were followed up for 1 year post injection to know the efficacy and durability of the treatment instituted. The data obtained from the participants of the study were subjected for statistical analysis and the following results were obtained.
Results
A total of 217 cases entered the study who were randomized into three groups and treatment instituted as per our study protocol. A total of 17 cases lost follow up post procedure. So, 200 cases were taken into consideration for statistical analysis.
| Variables | Group A (n=64) | Group B (n=69) | Group C (n=67) | P value | |
| Sex | Male | 43 | 33 | 38 | 0.41 |
| Female | 21 | 36 | 29 | ||
| Age | Mean ± SD | 51.85 ± 10.14 | 57.49 ± 10.00 | 53.96 ± 09.47 | 0.01 |
| Range (in years) | (36 – 72) | (39 – 77) | (33 – 75) | ||
Table 1: Patient’s demography.
| Follow up | Group A | Group B | Group C | P value |
| VAS score | ||||
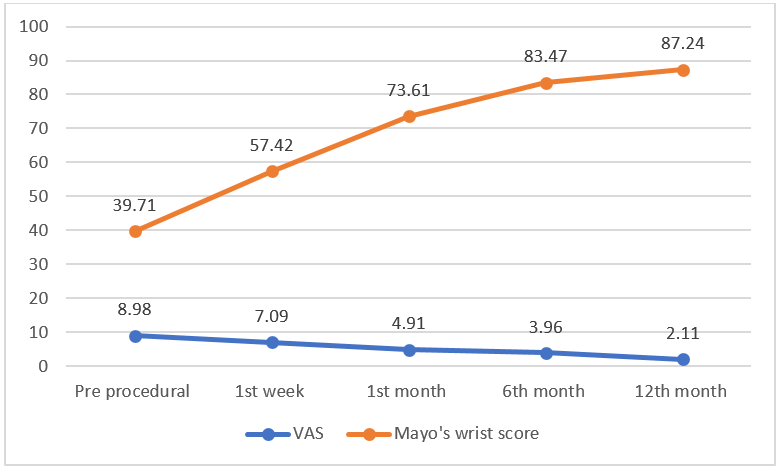
| Pre procedural | 8.63 ± 0.17 | 9.18 ± 0.38 | 8.98 ± 0.57 | 0.06 |
| 1st week | 7.09 ± 1.09 | 4.42 ± 1.30 | 7.09 ± .090 | 0.046 |
| 1st month | 6.37 ± 2.45 | 5.13 ± 2.07 | 4.91 ± 1.01 | <0.001 |
| 6th month | 5.01 ± 0.26 | 6.09 ± 1.41 | 3.96 ± 1.94 | <0.001 |
| 12th month | 7.61 ± 0.72 | 4.93 ± 1.95 | 2.11 ± 0.28 | <0.001 |
| Mayo’s Wrist score | ||||
| Pre procedural | 30.12 ± 6.47 | 36.43 ± 7.19 | 39.71±9.67 | 0.92 |
| 1st week | 36.19 ± 5.23 | 59.78 ± 4.14 | 57.42±6.91 | 0.27 |
| 1st month | 39.71 ± 4.47 | 63.45 ± 5.17 | 73.61±7.01 | 0.045 |
| 6th month | 51.43 ± 6.64 | 70.94 ± 6.29 | 83.47±6.83 | 0.003 |
| 12th month | 64.78 ± 7.12 | 72.01 ± 5.42 | 87.24±6.94 | 0.001 |
Table 2: VAS and Mayo’s Wrist scoring (Repeated ANOVA test).
| Group | Total | No of patients cured with 1st dose (at end of 1st month follow up) | No of patients cured with 2nd dose (after 4 weeks of initial dose) | No of patients with recalcitrant disease (at the end of 6th month follow up) |
| A (Conservative and physical therapy) | n=64 | 13 (20.31%) | 12 (18.75%) | 39 (60.93%) |
| B (Corticosteroid injection) | n=69 | 37 (53.62%) | 11 (15.94%) | 21 (30.43%) |
| C (Percutaneous needling & autologous PRP injection) | n=67 | 51 (76.11%) | 13 (19.40%) | 3 (4.47%) |
Table 3: Number of injections.
| Group | Pain | Swelling | Recurrence (at the end of 6th month) |
| A (n=64) | 51 (79.68%) | 34 (53.12%) | 39 (60.93%) |
| B (n=69) | 23 (33.33%) | 12 (17.39%) | 21 (30.43%) |
| C (n=67) | 45 (67.16%) | 17 (25.37%) | 3 (4.47%) |
Table 4: Complications.
Group A (n=64): The preprocedural and 12th month follow up mean VAS score and Mayo’s wrist scores were 8.63±0.17 and 30.12±6.47 improved to 7.61±0.72 and 64.78±7.12 respectively. A total of 25 (30.06%) cases had recovered from disease at the end of 2nd dose of treatment. At the end of 6th month follow up, 39 (60.93%) cases resulted in recurrence of symptoms.
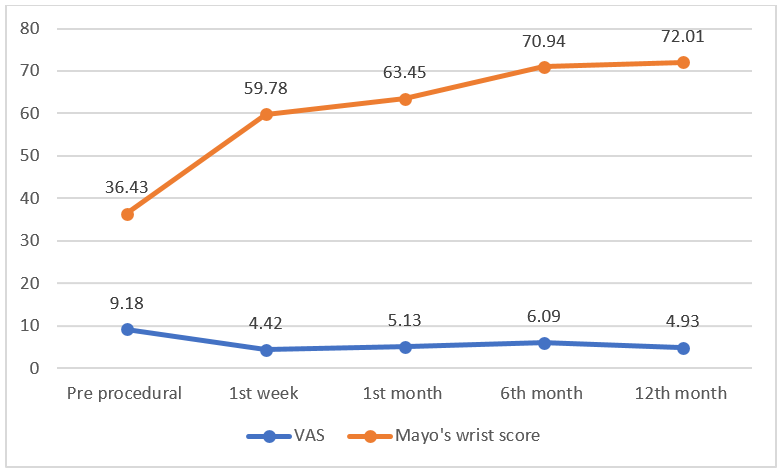
Group B (n=69): The preprocedural and 12th month follow up mean VAS score and Mayo’s wrist scores were 9.18±0.38 and 36.43±7.19 improved to 4.93±1.95 and 72.01±5.42 respectively. A total of 48 (69.56%) cases had recovered from disease at the end of 2nd dose of treatment. At the end of 6th month follow up, 21 (30.43%) cases resulted in recurrence of symptoms.
Group C (n=67): The preprocedural and 12th month follow up mean VAS score and Mayo’s wrist scores were 8.98±0.57 and 39.71±9.67 improved to 2.11±0.28 and 87.24±6.94 respectively. A total of 64 (95.52%) cases had recovered from disease at the end of 2nd dose of treatment. At the end of 6th month follow up, 3 (4.47%) cases resulted in recurrence of symptoms.
All three groups of patients were followed up for 1 year which showed a significant statistical difference with P value of <0.001 in VAS score and 0.001 in Mayo’s wrist scores among all three groups.
Discussion
de Quervain’s tenosynovitis is also called de Quervain’s stenosing tenosynovitis, washerwoman’s sprain or stenosing peritendinitis [1.] The pathophysiology of de Quervain’s tenosynovitis is due to repeated passage of tendon through narrow canal which leads to swelling and fibrotic nodule formation over abductor pollicis longus and extensor pollicis brevis tendons [2,3]. When the disease progresses, retinaculum thickens along with fibrocartilaginous metaplasia and synovial hypertrophy occurs [4]. The platelet rich plasma knocks down the retinacular thickening and synovial hypertrophy which leads to rejuvenation of tendon sheath. Rejuvenation occurs due to proper balance among pro-angiogenic, anti-angiogenic and chemotactic factors.
de Quervain’s tenosynovitis is also called de Quervain’s stenosing tenosynovitis, washerwoman’s sprain or stenosing peritendinitis [1.] The pathophysiology of de Quervain’s tenosynovitis is due to repeated passage of tendon through narrow canal which leads to swelling and fibrotic nodule formation over abductor pollicis longus and extensor pollicis brevis tendons [2,3]. When the disease progresses, retinaculum thickens along with fibrocartilaginous metaplasia and synovial hypertrophy occurs [4]. The platelet rich plasma knocks down the retinacular thickening and synovial hypertrophy which leads to rejuvenation of tendon sheath. Rejuvenation occurs due to proper balance among pro-angiogenic, anti-angiogenic and chemotactic factors.
Patients with dQSTS report a gradual onset of pain or tenderness at the radial styloid that may be accompanied by swelling. On clinical examination, patients will have decreased abduction and extension ranges of motion at the first carpometacarpal joint, pain with isometric activation of the APB and EPB tendons, and crepitus of tendons moving through the thickened extensor sheath. Finkelstein’s test is typically positive in such patients but should rule out the other causes of pain along the radial aspect of the wrist and forearm to clinch the accurate diagnosis [5].
Management options for de Quervain’s tenosynovitis are as follows [6-11]
A) Pharmacological management [6,7]
A) Pharmacological management [6,7]
- Analgesics and muscle relaxants,
- Local steroid infiltration in the form of 40 mg of triamcinolone into the affected tendon sheath which reduces inflammation,
- Local sodium hyaluronate injection, which act as a viscosupplement by increasing the viscosity of the synovial fluid, which helps to lubricate, cushion and reduce the pain
- Active range of wrist movements, ultrasonic therapy and soft tissue massage of the wrist joint,
- Home based exercise programme in the form of hot fomentation and active range of wrist movement exercises,
- Orthotics like braces and splints which reduce the micromotion at the injured area
- Open or arthroscopic release of fibrosis of tendon sheath covering APL and EPB tendons
- Ultrasound guided percutaneous needle tenotomy of the affected tendon sheath
- Loco-regional cryotherapy with -11°C to -140°C provides anti-inflammatory and analgesic effect to the degenerated tendon sheath
- Autologous platelet rich plasma (PRP) injection, homologous platelet lysate (HPL) injection
- Tissue bioengineering with mesenchymal stem cell and silk scaffolds, autologous tenocyte injection and injection of microRNA.
Jirarattanaphochai., et al. randomly assigned 160 patients to study the effect of an oral non-steroidal anti-inflammatory on the efficacy of steroid injection shows no benefit of oral NSAID administration. [12] Mardani-Kivi., et al. studied the efficacy of corticosteroid injection alone when compared to corticosteroid injection with thumb spica casting and concluded that a combination of both were better than injection alone as regards treatment success and functional outcomes, citing success rates of 69% and 93% respectively [13].
Hajder., et al. studied the efficacy of ultrasound guided injection of triamcinolone citing a success rate of 91% after up to two injections, highlighting the potential role of ultrasound in increasing injection accuracy [14]. Goldfarb., et al. studied the effect of steroid and local anaesthetic injection with and without bicarbonate finding an acidic injection preparation had no effect on the incidence of flare reaction compared to the neutral formula with bicarbonate [15].
Evan., et al. performed US guided percutaneous needle tenotomy with PRP injection for dQSTS case showed improved pain free results at the end of 3rd month. At 6th month follow up, VAS score improved to 10 out of 100 and patients had no recurrence of symptoms [16].
Bouras., et al. performed surgical exploration of first dorsal compartment and Le Viet plasty in 20 cases for dQSTS. At three years follow-up, the functional results were good in all the patients. Non-aesthetic scars were noticed in three patients. We did not notice neither a case of radial nerve injury nor a tendinous luxation in our series [17].
Alexander., et al. observed the long-term results of surgical release of de Quervain’s stenosing tenosynovitis in 94 cases. They concluded six perioperative complications, including one superficial wound infection, one delayed wound healing, and four transient lesions of the radial nerve. Simple decompression of both tendons and partial resection of the extensor ligament with a maximum of 3 mm can be recommended in operative treatment of dQSTS with excellent long-term results. [18]
Here our patients were treated according to their corresponding group protocol. At the end of 6th month follow up, a total of 39 (60.93%) cases in group A, 21 (30.43%) cases in group B and 3 (4.47%) cases in group C had recurrence. All these patients were followed up for 1 year which showed a statistical difference with P value of <0.001 in VAS score and 0.001 in Mayo’s wrist scores among all three groups. The recurrence cases were counselled for surgical release of dorsal compartment which is out of scope of this article.
Conclusion
Though the availability of various modalities of management for dQSTS, percutaneous needling with autologous platelet rich plasma injection is the most superior modality for de Quervain’s stenosing tenosynovitis which minimise the pain and improve the functional quality of life. Autologous PRP injection act as an osteointegrative and histopromotive agent which minimise the need for surgical management and decrease the morbidity of the patient.
Funding sources: Nil
Conflicts of interest: Nil
Acknowledgements: Nil
References
- Moore JS. (1997). De Quervain’s tenosynovitis. Stenosing tenosynovitis of the first dorsal compartment. J Occup Environ Med. 39(10):990–1002.
- Muckart RD. (1964). Stenosing tendovaginitis of abductor pollicis longus and extensor pollicis brevis at the radial styloid (de Quervain’s disease). Clin Orthop Relat Res. 33:201–8.
- Kay NR. (2000). De Quervain’s disease. Changing pathology or changing perception? J Hand Surg Br. 25(1):65–9.
- Clarke MT, Lyall HA, Grant JW, Matthewson MH. (1998). The histopathology of de Quervain’s disease. J Hand Surg Br. 23(6):732–4.
- Finkelstein H. (1930). Stenosing tendovaginitis at the radial styloid process. J Bone Joint Surg [Am]. 12:509–540.
- Rees JD, Maffulli N, Cook J. (2009). Management of tendinopathy. Am J Sports Med. 37(9):1855–67.
- Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. (2009). Corticosteroid injection for de Quervain’s tenosynovitis. Cochrane Database Syst Rev. 8; (3):CD005616.
- Backstrom KM. (2002). Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain’s tenosynovitis: a case report. J Orthop Sports Phys Ther. 32(3):86–97.
- Lamphier TA, Crooker C, Crooker JL. (1965). De Quervain’s disease. Ind Med Surg. 34:847–856.
- Capasso G, Vittorino T, Maffulli N, Turco G, Piluso G. (2002). Surgical release of de Quervain’s stenosing tenosynovitis postpartum: can it wait? Int Orthop. 26:23–25.
- Fu SC, Rolf C, Cheuk YC, Lui PP, Chan KM. (2010). Deciphering the pathogenesis of tendinopathy: a three-stages process. Sports Med Arthrosc Rehabil Ther Technol. 2:30.
- Jirarattanaphochai K, Saengnipanthkul S, Vipulakorn K, Jianmongkol S, Chatuparisute P, Jung S. (2004). Treatment of de Quervain disease with triamcinolone injection with or without nimesulide. A randomized, double-blind, placebo-controlled trial. J Bone Joint Surg Am 86-a (12): 2700-6.
- Mardani-Kivi M, Karimi MM, Bahrami F, Hashemi-Motlagh K, Saheb-Ekhtiari K, Akhoondzadeh N. (2014). Corticosteroid injection with or without thumb spica cast for de Quervain tenosynovitis. J Bone Joint Surg Am 39 (1): 37-41.
- Hajder E, de Jonge M, van der Horst CMA, Obdeijn M. (2013). The role of ultrasound-guided triamcinolone injection in the treatment of De Quervain's disease: Treatment and a diagnostic tool? Chir Main 32 (6): 403-7.
- Goldfarb CA, Gelberman RH, McKeon K, Chia B, Boyer MI. (2007). Extra-articular steroid injection: early patient response and the ncidence of flare reaction. J Hand Surg 32 (10): 1513-20.
- Peck Evan and Ely Erin. (2013). Successful treatment of de Quervain tenosynovitis with Ultrasound guided Percutaneous Needle Tenotomy and Platelet Rich Plasma Injection. The American Academy of Physical Medicine and Rehabilitation. 5: 438-441.
- Bouras Y, El Andaloussi Y, Zaouari T, Touil N, Fnini S, Chikhaoui N, Largab A. (2010). Surgical treatment in De Quervain's tenosynovitis. About 20 cases. Ann Chir Plast Esthet. 55 (1):42-5.
- Alexander Scheller, Ralph Schuh, Wolfgang Hönle and Alexander Schuh. (2009). Long-term results of surgical release of de Quervain’s stenosing tenosynovitis. Int Orthop. 33(5): 1301–1303.
Citation: Ramesh.R, Madhan Jeyaraman., et al. (2019). Conservative & Physical therapy vs Corticosteroid therapy vs Percutaneous Needling with Autologous Platelet Rich Plasma therapy for de Quervain’s Stenosing Tenosynovitis in a Tertiary Care Hospital. Journal of Orthopaedic and Trauma Care 1(1).
Copyright: © 2019 Madhan Jeyaraman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.