Research Article
Volume 1 Issue 1 - 2019
Comparison of Open Reduction External Fixator and Open Reduction K Wire Temporary Arthrodesis in Treatment of Chronic Elbow Dislocation
Van Yuzuncu Y?l University Dursun Odaba? Medical Center Orthopedics and Traumatology Department, Turkey
*Corresponding Author: Sezai Özkan, Van Yuzuncu Y?l University Dursun Odaba? Medical Center Orthopedics and Traumatology Department, Turkey.
Received: September 16, 2019; Published: September 23, 2019
Introduction
Dislocation of the elbow is the second most common type of dislocation in adults (1). The treatment of early diagnosed dislocations is closed reduction and joint motion range exercises under control performed after. If the dislocation remains untreated up to 3 weeks, it is called ignored or chronic elbow dislocation (2-3). Since it is very difficult to achieve and maintain the reduction by non-surgical methods, surgical treatment is suggested in these cases. Chronic elbow dislocation (CED) is rare in developed countries. Due to rare appearance of the ignored elbow dislocation, there are limited number of studies including small patient series. The aim of the present study was to compare the outcomes of the patients who had surgery due to chronic elbow dislocation through open reduction- k wire temporary arthodesis (KWTA) and open reduction-external fixation (EF) methods.
Material and Method
Study Group
Surgical procedures were performed on 11 patients with CED by same surgeon in orthopedics and Traumatology Clinic between 2011 and 2017. Three patients who did not come to the follow-up visits were excluded. Remaining patients included 5 males and 3 females with age average of 30.5 (range; 22-60). Complete dislocation was detected in elbow X-rays of the patients; 3 patients developed fracture mal-union concomitant to the fracture. All injuries were closed. None of the patients had neurovascular deficit. Seven patients referred to a bonesetter whereas dislocation of 1 patient was missed in the emergency service. The average period of referral to our clinic after dislocation was 10.1 (range 2-60) months. Concomitant conditions included medial condyl fracture in 1 patient, lateral condyl fracture in 1 patient and fracture of the radius head in 1 patient. Written consent was obtained from the patients for the study.
Surgical procedures were performed on 11 patients with CED by same surgeon in orthopedics and Traumatology Clinic between 2011 and 2017. Three patients who did not come to the follow-up visits were excluded. Remaining patients included 5 males and 3 females with age average of 30.5 (range; 22-60). Complete dislocation was detected in elbow X-rays of the patients; 3 patients developed fracture mal-union concomitant to the fracture. All injuries were closed. None of the patients had neurovascular deficit. Seven patients referred to a bonesetter whereas dislocation of 1 patient was missed in the emergency service. The average period of referral to our clinic after dislocation was 10.1 (range 2-60) months. Concomitant conditions included medial condyl fracture in 1 patient, lateral condyl fracture in 1 patient and fracture of the radius head in 1 patient. Written consent was obtained from the patients for the study.
| Patient No. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Age | 60 | 27 | 27 | 25 | 38 | 22 | 22 | 23 |
| Gender | M | M | M | F | F | M | F | M |
| Side | R | L | R | R | L | R | R | R |
| Duration between the injury and operation (mo) | 3 | 60 | 2 | 3 | 4 | 3 | 3 | 6 |
| Concomitant injury | - | RH | - | - | HLC | - | - | HMC |
| Surgery | EF | EF | EF | EF | KWTA | KWTA | KWTA | KWTA |
| RH:Radius Head fx | HMC:Humerus Medial Condil fx | HML:Humerus Lateral Condil fx | ||||||
Table 1: Demgraphic and clinical characteristics of patients.
Surgical technique
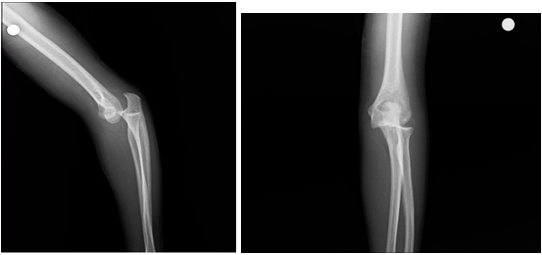
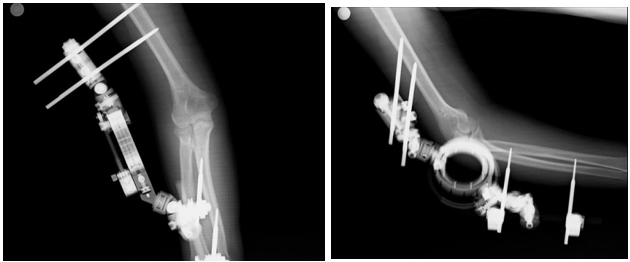
Anteroposterior, lateral, oblique X-rays of the elbows of the patients were taken. The patients were operated at supine position by implementing a tourniquette on proximal side of the arm. The elbow joint was accessed through a posterior incision of 25 cm. Medial and lateral skin flaps were removed. The ulnar nerve was detected, marked and transposed to anterior side subfacially after reduction of the dislocated joint. Then, triceps muscle were dissected sharply from medial and lateral sides up to olecranon; and the joint was revealed. The fibrotic and granulation tissues detected in the olecranon fossa, medial and lateral sides of the joint, between distal side of humerus and radius head, between proximal side of the radius and ulna were cleared carefully. Heterotopic ossifications were removed by osteotome and mini ronger. The collateral ligaments which were contracted were released to allow the reduction. Then, collateral ligament reconstruction was not performed. After reduction of ulnatrochlear joint, instability was observed on varus and valgus on the elbow joint of all patients. A fixator system with elbow movement unit (Orthofix Galaxy External Fixation System, Verona, Italy) was implemented to some of the patients. EF was performed as follows; pins of 5.6 mm were placed on lateral side of the humerus and pins of 3.5 mm were placed on medial side of the distal ulna. Humerus pinning was performed with an open technique to preserve the radial nerve. The elbow was fixed at 110 degrees after installation of fixator system. The concomitant fractures unioned; therefore, they were left as they were. (Figure 1,2,3,4)
Anteroposterior, lateral, oblique X-rays of the elbows of the patients were taken. The patients were operated at supine position by implementing a tourniquette on proximal side of the arm. The elbow joint was accessed through a posterior incision of 25 cm. Medial and lateral skin flaps were removed. The ulnar nerve was detected, marked and transposed to anterior side subfacially after reduction of the dislocated joint. Then, triceps muscle were dissected sharply from medial and lateral sides up to olecranon; and the joint was revealed. The fibrotic and granulation tissues detected in the olecranon fossa, medial and lateral sides of the joint, between distal side of humerus and radius head, between proximal side of the radius and ulna were cleared carefully. Heterotopic ossifications were removed by osteotome and mini ronger. The collateral ligaments which were contracted were released to allow the reduction. Then, collateral ligament reconstruction was not performed. After reduction of ulnatrochlear joint, instability was observed on varus and valgus on the elbow joint of all patients. A fixator system with elbow movement unit (Orthofix Galaxy External Fixation System, Verona, Italy) was implemented to some of the patients. EF was performed as follows; pins of 5.6 mm were placed on lateral side of the humerus and pins of 3.5 mm were placed on medial side of the distal ulna. Humerus pinning was performed with an open technique to preserve the radial nerve. The elbow was fixed at 110 degrees after installation of fixator system. The concomitant fractures unioned; therefore, they were left as they were. (Figure 1,2,3,4)
Elbow flexion-extension exercises were started at pain limit. The exercises were implemented as 20 repetitions once a day. The fixator system was removed in the polyclinic without anesthesia at postoperative week 3. The patients were instructed to keep their elbows in a sling after joint gap exercises. Progressive resistance exercises were started to strengthen the muscles around the elbow at week 6. KWTA was implemented as follows. A K-wire (size 1.8; T?psan, ?zmir, Turkey) was inserted as perpendicular to the ulnar axis on 1 cm below the olecranon tip. The K-wire was forwarded into the humerus transarticularly when the elbow is at flexion of 90 degrees. Reduction control was performed by a scope. The K-wire was removed in the polyclinic without anesthesia at postoperative week 3. Passive exercises of the elbow started at pain limits as twice a day. The patients were told to apply a sling to keep the elbow at 90 degrees after the exercise. Progressive resistance exercises were started to strengthen the muscles around the elbow at week 6.
Main Outcome Measures
The patients were evaluated at postoperative months 3 and 6 and then semi-anually. Flexion-extension gaps of the patients at referral and final control were measured by a hand-held goniometer. Quick Disabilities of the Arm, Shoulder and Hand (Q Dash), Mayo Elbow Performance Indexes (MEPI) and Short Form-36 (SF-36) painsub parameter were recorded.
The patients were evaluated at postoperative months 3 and 6 and then semi-anually. Flexion-extension gaps of the patients at referral and final control were measured by a hand-held goniometer. Quick Disabilities of the Arm, Shoulder and Hand (Q Dash), Mayo Elbow Performance Indexes (MEPI) and Short Form-36 (SF-36) painsub parameter were recorded.
The Quick DASH is a questionnaire consisting of 11 items that measure severity of symptoms as well as individual’s ability to complete tasks, absorb forces. Higher scores in Quick DASH indicate a greater level of disability and severity whereas lower scores indicate a lower level of disability.
The Mayo Elbow Performance Index (MEPI) is an instrument used to test the limitations while using the elbow during activity of daily life (ADL). This specific test utilizes 4 subscales including pain, arc of motion of the humeroulnar articulate, stability and disorders in ADL. The scoring is done as follows; below 60 is poor, 60-74 is fair, 75-89 is good and 90-100 is excellent.
SF-36 is a set of generic, coherent, and self-reporting quality-of-life measure. These measures are used for monitoring and assessment of care outcomes in adult patients. SF-36 pain subparameter consist of two questions; How much bodily pain have you had during the past 4 weeks? During the past 4 weeks, how much did pain interfere with your normal work? (including both work outside the home and housework) The sum of these two item is divided to two in order to detect mean of pain parameter.
An independent observer who has minimum 5 years of experience assessed Broberg-Morrey radiology score of the patients in their final control visit. Grades are demonstrated as follows; grade 0, normal joint; grade 1, slight joint-space narrowing with minimum osteophyte formation; grade 2, moderate joint-space narrowing with moderate osteophyte formation; and grade 3, severe degenerative change with gross destruction of the joint.
Statistical analysis
The independent two sample t-test was used to determine the association of preoperative and postoperative q dash, mepi, flexion/extension (f/e) and postoperative SF-36 values.
The independent two sample t-test was used to determine the association of preoperative and postoperative q dash, mepi, flexion/extension (f/e) and postoperative SF-36 values.
The independent two sample t-test was also used to determine whether preoperative and postoperative q dash, mepi, f/e and postoperative sf-36 values change. Pearson's correlation analysis was implemented to determine whether delay duration and preoperative and postoperative q dash, mepi, f/e and postoperative sf-36 values change.
Fisher's exact test was used to detect if there is any association between fixation method and Broberg radiological stage. Since two procedures were performed according to availability of EF, the patients are naturally randomized. Statistical significance were noted at a minimum of P < 0.05 threshold. All data were analyzed at IBM SSPS version 23.0(IBM Corp., Armonk, NY, USA)
Results
Delay duration of the patients for the surgery was 10.5 (range 2-60 months) in average. Three of 8 patients had concomitant fractures. Eight patients were followed for 4.6 (range 3-6 years) years. None of the patients developed pin path infection and pin loosening. Postoperative MEPI, Q DASH, final ROM and postoperative SF-36 pain values of the patients were presented in Table 2. There was not any statistically significant association between fixation method and Broberg stage (p>0.05). Statistical data of the patients clinical evaluations was shown in Table 3.
| Patient No. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| MEPI score Pre/post peration | 40/90 | 25/85 | 20/75 | 35/80 | 10/65 | 20/80 | 20/65 | 25/70 |
| Q DASH-score Pre/post operation | 66/11 | 73/25 | 77/25 | 86/38 | 66/52 | 55/39 | 84/52 | 80/25 |
| Range of Motion Pre operation-Final |
10/110 | 10/120 | 20/120 | 10/120 | 10/120 | 15/115 | 20/105 | 20/90 |
| Final SF-36 pain score | 77.5 | 90 | 77.5 | 90 | 55 | 45 | 67,5 | 77,5 |
| Broberg-Morrey Rating scale | grade 1 | grade 1 | grade 0 | grade 1 | grade 2 | grade 0 | grade 2 | grade 1 |
MEPI: Mayo elbow performance index, Q DASH: Quick Disabilities of the Arm, Shoulder and Hand, SF-36: Short Form 36
Table 2: Clinical and radiographic outcomes of the patients.
Table 2: Clinical and radiographic outcomes of the patients.
| Clinical parameters | EF Group | KWTA Group | p value |
| Pre op. MEPI | 30 | 18.75 | p>0.05 |
| Post op. MEPI | 81.25 | 70 | p<0.05 |
| Pre op. Q DASH | 75.56 | 71.08 | p>0.05 |
| Post op. Q DASH | 25.56 | 42.04 | p<0.05 |
| Range of Motion | |||
| Pre operation | 12.5 | 16.25 | p>0.05 |
| Final | 117.5 | 107.5 | p>0.05 |
| Final SF-36 pain score | 83.75 | 61, 25 | p<0.05 |
Table 3: Clinical evaluation.
Discussion
Number of the cases with chronic dislocation of the elbow decreased dramatically due to easy access to medical centers and development in imaging techniques. The patients with ignored fractures after interventions done by local bonesetters in the study region are still detected even they are rare. Majority of the studies about this subject was reported by the surgeons from less developed countries (4-5-6). Seven patients in the present study were exposed to traditional bonesetter intervention. Diagnosis of elbow dislocation may be missed in the multiple trauma patients and in the patients with ipsilateral pathology (7-8). There is not any multiple trauma or ipsilateral pathology in the patient whose diagnosis was missed in the emergency service. It was detected from the file of the aforesaid patient, he was taken to ER in an unconscious state and he had high level of alcohol in the blood. We believe that a careful orthopedic examination would be useful for unconscious patient.
There is not any consensus on surgical treatment method for chronic elbow dislocation. Many surgical methods were described. Posterior approach to the elbow facilitates to access the medial and lateral joint through a single incision. The joint was accessed from medial and lateral edges of the triceps through posterior approach in 8 patients of our series; reduction was achieved by loosening the medial and lateral collateral ligaments; therefore triceps extension was not necessary. It was reported that triceps extension is useful for joint stability, early start to movements and prevention of postoperative flexion contracture (9-10). Mahaisavariya et al (11) reported that triceps extension was necessary after 4 to 8 weeks. Kapukaya et al (12) reported successful outcomes in their patients series whom they implemented triceps extension. We had a patient whom we achieved reduction without triceps extension at month 60. Papandrea et al (13) reported that concentric reduction is the key point of the surgery. We achieved concentric reduction by releasing the collateral ligaments. A disadvantage of collateral ligament release is development of varus valgus instability on the elbow after reduction in all patients. Repair of collateral ligament in case of instability was first suggested by Arifiles (14). There are articles suggesting that repair of collateral ligament is not necessary to provide elbow stability (9,15). We resolved the instability problem by fixing the elbow by K wire or external fixator. We did not detect any finding for instability in the control visits.
A common consensus of many authors is to release the ulnar nerve regardless from the surgical method (16-17). We performed ulnar nerve release and subfacial transfer to anterior for all patients. We did not detect any problem on the ulnar nerve in any of the patients. Prolongation of delay period for surgery leads to worse outcomes (18-19). We observed that SF-36 pain score was lower by delay of the surgery.
Ring et al (20) reports that negative functional outcomes are observed in case of concomitant fractures. We detected that the concomitant fracture did not affect the functional outcomes. Boretto et al (21) compared simple and complex elbow dislocations and reported that there is not any difference between two groups in terms of functional and joint movement unless the fracture causes any neurovascular complication. Furthermore, this outcome may be related to the fact that concomitant fractures in our series were less or never associated with the joint.
Open reduction-external fixation was performed on 4 patients in the present study. There was not any difference in MEPI, Q DASH scores and flexion-extension gap averages before the surgery; however, MEPI, Q DASH, SF-36 scores of the patients who had external fixation were better than those who had fixation with K-wire. There are many studies suggesting that external fixator in treatment of chronic elbow dislocation would provide better outcomes (16,22). EF increase the joint stability after the surgery and enables early movement. It is known that early movement and distraction have a preserving and healing effect on the cartilage of which the load falls on (23-24). We believe that higher scores may depend on this effect. The K-wire which was placed with a transarticular approach might have caused a damage in the patients who had temporary arthodesis. However, Islam et al (25) demonstrated similar outcomes for flexion-extension gaps of the elbows of the patients after their surgical procedures with KWTF; however, they measured MEPI scores higher than our scores. They also forwarded K-wires from ulna to humerus with a transarticular approach without triceps muscle extension and collateral repair. However, their patient groups included younger patients.
We considered that the external fixator group would have more joint motion range. There are studies addressing that prolonged joint immobilization would cause joint stiffness (26-27). However, postoperative motion ranges were similar in both groups. Ring et al. (28) compared hinged external fixator and cross pinning for treatment of elbow instability; and they did not detect any difference between these two methods in terms of joint motion ranges and Broberg-Morrey scores. Although our patients had higher pain scores, we believe that they improved their motion ranges to fulfill their daily activities. Regular and long-term controls may contribute promotion of joint motion range exercises of the patients. This may explain similar motion range outcomes in EF and KWTA groups.
There was not any association between fixation method and Broberg-Morrey stage. The arthosis and osteophytes appear to be related to the cartilage injury appeared after the trauma. Lindenhovius et al (29) reported that Broberg and Morrey classification system is affected by specialization and experience of the assessor with a moderate interobserver safety. This may be related to similar outcomes of Broberg-Morrey stages.
Conclusion
Compared with implent of K- wire, implement of external fixator resulted in improved surgical outcomes of chronic elbow dislocations
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was designed as a retrospective data assessment; therefore, ethics committee approval was not required.
References
- Safran MR, Baillargeon D. (2005). Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg. 14(1 Suppl S): 179-85. Review.
- Freeman III BL. (1998). Old unreduced dislocations. In: Crenshaw AH, editor. Campbell’s operative orthopaedics. 9th edition. St. Louis: Mosby. pp. 2673–4.
- Rockwood AC, editor. Rockwood CA. 4th ed. Philadelphia, PA: Lippicott-Raven; 1996. Treatment of old unreduces posterior dislocation of elbow; pp. 975-6.
- Azmi I, Razak M, Hyzan Y. (1998). The results of treatment of dislocation andfracture--dislocation of the elbow--a review of 41 patients. Med J Malaysia.
- Pundkar GN, Sonar SB, Kulkarni OP. (2017). A Case of 3-month-old Neglected Elbow Dislocation Managed by Open Reduction and Cruciate Ligament Reconstruction Using Tendon Graft. J Orthop Case Rep. Jul-Aug;7 (4): 58-60.
- Lahrach K, Ammoumri O, Mezzani A, Benabid M, Marzouki A, Boutayeb F. (2015). A caseof neglected fracture dislocation of the elbow with preservation of elbowfunction. Pan Afr Med J. Mar 3;20:199.
- Ali FM, Krishnan S, Farhan MJ. (1998). A case of ipsilateral shoulder and elbow dislocation: an easily missed injury. J Accid Emerg Med. May; 15 (3): 198.
- Khan MR, Mirdad TM. (2001). Ipsilateral dislocation of the shoulder and elbow. Saudi Med J. Nov;22 (11): 1019-21.
- Mahaisavariya B, Laupattarakasem W. (2005). Neglected dislocation of the elbow.Clin Orthop Relat Res. (431): 21-5.
- Karakoyun Ö, Erol MF, Küçükkaya M. (2014). Treatment of neglected elbow dislocations with the help of hinged external fixator:Report of two cases. Journal of Clinical and Experimental Investigations. 5 (2): 307-12.
- Mahaisavariya B, Laupattarakasem W, Supachutikul A, Taesiri H,Sujaritbudhungkoon S. (1993). Late reduction of dislocated elbow. Need triceps belengthened? J Bone Joint Surg Br. May;75 (3): 426-8.
- Kapukaya A, Ucar BY, Gem M. (2013). Open reduction and Kirschner wire fixation with triceps lengthening for neglected elbow dislocations. J Orthop Surg (Hong Kong). Aug; 21 (2):178-81.
- Papandrea RF, Morrey BF, O’Driscoll SW. (2007). Reconstruction for persistent instability of the elbow aftercoronoid fracture-dislocation. J Shoulder ElbowSurg;16(1):68-77.
- Arafiles RP. (1987). Neglected posterior dislocation of the elbow: a reconstruction operation. J Bone Joint Surg Br; 69:199-202.
- Mehta S, Sud A, Tiwari A, Kapoor SK. (2007). Open reduction for late-presenting posterior dislocation of the elbow. J Orthop Surg (Hong Kong); 15(1):15-21.
- Ivo R, Mader K, Dargel J, Penning D. (2009). Treatment of chronically unreduced complex dislocations of the elbow. Strat Traum Limb Recon 4:49-55.
- Anderson DR, Haller JM, Anderson LA, Hailu S, Chala A, O?Driscoll SW. (2018). Surgical Treatment of Chronic Elbow Dislocation Allowing for Early Range of Motion: Operative Technique and Clinical Results. J Orthop Trauma. Apr; 32 (4): 196-203.
- Morrey BF, Askew LJ, Chao EY. (1981). A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 63: 872-7.
- Naidoo KS. (1982). Unreduced posterior dislocations of the elbow. J Bone Joint Surg Br 64: 603-6.
- Ring D, Jupiter JB, Zilberfarb J. (2002). Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 84: 547-51.
- Boretto JG, Rodriguez Sammartino M, Gallucci G, De Carli P, Ring D. (2014). Comparative study of simple and complex open elbow dislocations. Clin OrthopRelat Res. Jul; 472 (7): 2037-43.
- Jupiter JB, Ring D. (2002). Treatment of unreduced elbow dislocations with hinged external fixation. J Bone Joint Surg Am; 84:1630-5.
- Behrens F, Kraft EL, Oegema TR Jr. (1989). Biochemical changes in articular cartilage after joint immobilization by casting or external fixation. J Orthop Res.;7(3): 335-43.
- Nishino T, Chang F, Ishii T, Yanai T, Mishima H, Ochiai N. (2010). Joint distractionand movement for repair of articular cartilage in a rabbit model with subsequent weight-bearing. J Bone Joint Surg Br. Jul; 92 (7):1033-40.
- Islam S, Jahangir J, Manzur RM, Chowdury AA, Tripura N, das A. (2012). Management of neglected elbow dislocations in a setting with low clinical resources. Orthop Surg. Aug;4(3):177-81. 26. Stehle
- J, Gohlke F. (2011). Classification of elbow stiffness and indications for surgical treatment. Orthopade. Apr; 40(4):282-290.
- Lee S, Sakurai T, Ohsako M, Saura R, Hatta H, Atomi Y. Tissue stiffness induced by prolonged immobilization of the rat knee joint and relevance of AGEs(pentosidine). Connect Tissue Res. 2010 Dec;51(6):467-77. doi:10.3109/03008201003686941. Epub 2010 Jul 6. PubMed PMID: 20604714.
- Ring D, Bruinsma WE, Jupiter JB. (2014). Complications of hinged external fixationcompared with cross-pinning of the elbow for acute and subacute instability. ClinOrthop Relat Res. 472(7): 2044-8.
- Lindenhovius A, Karanicolas PJ, Bhandari M, Ring D. (2012). COAST Collaborative.Radiographic arthrosis after elbow trauma: interobserver reliability. J Hand SurgAm. 37(4): 755-9.
Citation: Cihan Adanas, Sezai Özkan and Hasan Onur Arik. (2019). Comparison of Open Reduction External Fixator and Open Reduction K Wire Temporary Arthrodesis in Treatment of Chronic Elbow Dislocation. Journal of Orthopaedic and Trauma Care 1(1).
Copyright: © 2019 Sezai Özkan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.