Review Article
Volume 6 Issue 1 - 2024
Causes of Dry Eye Syndrome
1Student Pharmaceutics Department Sri Ramakrishna College of Pharmacy, Coimbatore, Tamil Nadu
2Professor Pharmaceutics Department Sri Ramakrishna College of Pharmacy, Coimbatore, Tamil Nadu
2Professor Pharmaceutics Department Sri Ramakrishna College of Pharmacy, Coimbatore, Tamil Nadu
*Corresponding Author: K. Priya, Student Pharmaceutics Department Sri Ramakrishna College of Pharmacy, Coimbatore, Tamil Nadu.
Received: April 10, 2024; Published: April 22, 2024
Abstract
Dry Eye Syndrome (DES) is a very common, multifactorial disease of the lacrimal functional unit that results in hyperosmolarity, tear film instability, chronic irritation, and inflammation of the ocular surface. (J. Shimazaki, 2018)
According to estimates, between 5 and 50 per cent of adults worldwide suffer from dry eye. This indicates how common the condition is. A comprehensive understanding of complications associated with DES is made possible by the remarkable diversity in medical backgrounds and sensitivity to symptoms among patients with DES. Over the past few years, it has become clear that DES is a tear film disorder brought on by either excessive or insufficient tear evaporation. The annual treatment costs associated with dry eye disease may exceed fifty-five billion dollars in the United States. Therefore, new treatments for dry eye must be developed for the benefit of both Dry Eye patients and the ophthalmic industry. (Farhat et al. 2015)
Introduction
Common Causes of Dry Eye
Dry eyes are caused by a variety of reasons that disrupt the healthy tear film. Your tear film has three layers: fatty oils, aqueous fluid and mucus. This combination usually keeps the surface of your eyes lubricated, smooth and clear. Problems with any of these layers can cause dry eyes.
Dry eyes are caused by a variety of reasons that disrupt the healthy tear film. Your tear film has three layers: fatty oils, aqueous fluid and mucus. This combination usually keeps the surface of your eyes lubricated, smooth and clear. Problems with any of these layers can cause dry eyes.
Reasons for tear film dysfunction are many, including hormone changes, autoimmune disease, inflamed eyelid glands or allergic eye disease. For some people, the cause of dry eyes is decreased tear production or increased tear evaporation.
Reasons for tear film dysfunction are many, including hormone changes, autoimmune disease, inflamed eyelid glands or allergic eye disease. For some people, the cause of dry eyes is decreased tear production or increased tear evaporation.
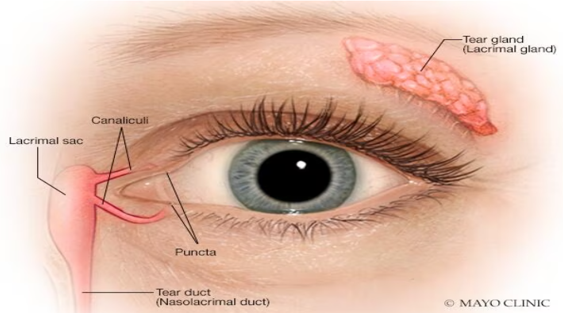
Tear Glands and Tear Ducts
The tear glands located above each eyeball called the lacrimal glands, continuously supply tear fluid that's wiped across the surface of your eye each time you blink your eyelids. Excess fluid drains through the tear ducts into the nose.(Golden MI et al. 2023)
The tear glands located above each eyeball called the lacrimal glands, continuously supply tear fluid that's wiped across the surface of your eye each time you blink your eyelids. Excess fluid drains through the tear ducts into the nose.(Golden MI et al. 2023)
Decreased Tear Production
Dry eyes can occur when you're unable to produce enough liquid tears, also called aqueous fluid. The medical term for this condition is keratoconjunctivitis sicca (ker-uh-toe-kun-junk-tih-VY-tis SIK-uh). Common causes of decreased tear production include
Dry eyes can occur when you're unable to produce enough liquid tears, also called aqueous fluid. The medical term for this condition is keratoconjunctivitis sicca (ker-uh-toe-kun-junk-tih-VY-tis SIK-uh). Common causes of decreased tear production include
- Aging
- Certain medical conditions including Sjogren's syndrome, allergic eye disease, rheumatoid arthritis, lupus, scleroderma, graft vs. host disease, sarcoidosis, thyroid disorders or vitamin A deficiency
- Certain medicines, including antihistamines, decongestants, hormone replacement therapy, antidepressants, and medicines for high blood pressure, acne, birth control and Parkinson's disease.
- Corneal nerve desensitivity caused by contact lens use, nerve damage or laser eye surgery, though symptoms of dry eyes related to this procedure are usually temporary.(Golden MI et al.2023)
Increased Tear Evaporation
The oil film produced by small glands on the edge of your eyelids (meibomian glands) might become clogged. Blocked meibomian glands are more common in people with rosacea or other skin disorders. (Golden MI et al. 2023)
The oil film produced by small glands on the edge of your eyelids (meibomian glands) might become clogged. Blocked meibomian glands are more common in people with rosacea or other skin disorders. (Golden MI et al. 2023)
Common Causes of Increased Tear Evaporation Include
- Posterior blepharitis (meibomian gland dysfunction)
- Blinking less often, which tends to occur with certain conditions, such as Parkinson's disease; or when you're concentrating during certain activities, such as while reading, driving or working at a computer
- Eyelid problems, such as the lids turning outward (ectropion) and the lids turning inward (entropion)
- Eye allergies
- Preservatives in topical eye drops
- Wind, smoke or dry air
- Vitamin A deficiency (Salmon JF, 2020)
Dry Eye Due to Diabetes
Diabetes mellitus (DM) has been identified as one of the leading systemic risk factors for DES. The reported prevalence of DES in diabetics is 15–33% in those over 65 years of age and increases with age and is 50% more common in women than in men.
Diabetes mellitus (DM) has been identified as one of the leading systemic risk factors for DES. The reported prevalence of DES in diabetics is 15–33% in those over 65 years of age and increases with age and is 50% more common in women than in men.
The incidence of dry eye is correlated with the level of glycated haemoglobin: the higher the level of glycated haemoglobin, the higher the incidence of dry eye.
Approximately 20% of dry eyes occurred in individuals with Type 2 diabetes aged between 43 and 86 years. 53% of patients with either diabetes or borderline diabetes had self-reported clinically relevant dry eyes. (Lin Zhao et al 2016)
Significant associations have been identified between diabetic retinopathy (DR) and DES. 17.1% of DES in patients with DM was found to have mild non-proliferative diabetic retinopathy (NPDR), 17.1% had moderate NPDR, 11.1% had severe non-proliferative diabetic retinopathy (NPDR), and 25.1% had proliferative diabetic retinopathy (PDR).
DR is also associated with a decrease in tear film function. Tear break-up time (BUT) and Schirmer's test values were significantly decreased in the PDR group compared to the non-DR group while corneal fluorescein staining scores, positive rate of rose Bengal staining, the surface regularity index, and the surface asymmetry index were increased. The concentrations of lactoferrin and tear-specific prealbumin were decreased in the DR group. The odds of DR in DES were 2.29 (CI = 1.16–4.52, P = 0.016) and both DES and retinopathy were associated with HbA1c. (Lin Zhao et al 2016)
LFU plays a regulatory role in tear secretion and tear film formation and maintains the normal physiology of the ocular surface; damage to any component of LFU leads to tear-deficient or evaporative DES. Tear hyperosmolarity and tear film instability caused by LFU and ocular surface dysfunction are the key factors in DES. Effects of hyper glycemia on any component of the LFU may be transferred to the entire system via neural connections, leading to insufficient tear production or excess tear loss, abnormalities in blinking, and changes in tear film composition. (Lin Zhao et al 2016)
The lacrimal function unit (LFU) is composed of the “cornea, conjunctiva, lacrimal gland, meibomian gland, lids, and the sensory and motor nerves that connect them,” which protect and maintain the tear film and normal function of the ocular surface. LFU plays a regulatory role in tear secretion and tear film formation to maintain the normal physiology of the ocular surface; damage to any component of LFU leads to tear-deficient or evaporative diabetes mellitus-associated dry eye syndrome. (Lin Zhao et al 2016)
Breast Cancer Causing Symptomatic Dry Eye (Sde)
- Breast cancer patients undergoing systemic treatment have a fairly high prevalence of symptomatic dry eye.
- Around 40% of them experienced moderate to severe degrees of dry eye.
- The severity of symptomatic dry eye in the exposure group showed cycle-dependency.
- SDE was significantly predominant in women with breast cancer undergoing systemic adjuvant treatment.
- Dry eye assessments among patients receiving more than four cycles of chemotherapy or targeted therapy, thus early revealing possible dry eye conditions to both patients and clinicians for further specialized examination and treatment. (Feng Jin et al., 2020)
Dry Eye Due to Anti-Hypertensive Drug
Antihypertensive (anti HT) therapy causes Dry Eye Syndrome, which has been claimed for years however most of the publications are epidemiological studies. Prospective, non-randomized clinical study. A total of 71 patients who would be initiated anti HT medication due to elevated systemic blood pressure were included in the study. Thirty of these patients were given anti HT drugs containing diuretic (diuretic +), and 41 of them were given diuretic-free drugs (diuretic). While the number of patients medicated in the group that received Angiotensin Converting Enzyme inhibitors (ACE inh)/Angiotensin receptor blockers (ARB) (ACE/ARB +) was 29, the number of those medicated in the ACE/ARB-free group (ACE/ARB) was 42. Ocular surface disease index scores, tear osmolarity, Schirmer I test, tear film break-up time (TBUT), fluorescein (FL) and rose bengal corneal staining patterns of the patients were analyzed. The patients were examined through the repetition of all the tests in the 1st and the 3rd month. Results: The participants (n ¼ 71) comprised 38 males and 33 females with a mean age of 51.8 ± 10.4. When the first (0–1st month) and the third month (0–3rd months) control measurements between diuretics (+) and diuretics () groups before and after anti HT therapies were compared, a statistically significant difference was not found in any of the tests applied. When the 0–1st-month measurements of ACE/ARB (+) and ACE/ARB () groups were compared, it was observed that staining with FL in the ACE/ARB (+) group decreased in a statistically significant manner (p ¼ 0.035) and there was a significant increase in TBUT values (p ¼ 0.022). Discussion and conclusion: The use of antiHT drugs containing diuretics had no adverse effect on the tear function tests, but using drugs that contain ACE/ARB could have a positive impact. (Emine Kalkan Akcay 2014)
Antihypertensive (anti HT) therapy causes Dry Eye Syndrome, which has been claimed for years however most of the publications are epidemiological studies. Prospective, non-randomized clinical study. A total of 71 patients who would be initiated anti HT medication due to elevated systemic blood pressure were included in the study. Thirty of these patients were given anti HT drugs containing diuretic (diuretic +), and 41 of them were given diuretic-free drugs (diuretic). While the number of patients medicated in the group that received Angiotensin Converting Enzyme inhibitors (ACE inh)/Angiotensin receptor blockers (ARB) (ACE/ARB +) was 29, the number of those medicated in the ACE/ARB-free group (ACE/ARB) was 42. Ocular surface disease index scores, tear osmolarity, Schirmer I test, tear film break-up time (TBUT), fluorescein (FL) and rose bengal corneal staining patterns of the patients were analyzed. The patients were examined through the repetition of all the tests in the 1st and the 3rd month. Results: The participants (n ¼ 71) comprised 38 males and 33 females with a mean age of 51.8 ± 10.4. When the first (0–1st month) and the third month (0–3rd months) control measurements between diuretics (+) and diuretics () groups before and after anti HT therapies were compared, a statistically significant difference was not found in any of the tests applied. When the 0–1st-month measurements of ACE/ARB (+) and ACE/ARB () groups were compared, it was observed that staining with FL in the ACE/ARB (+) group decreased in a statistically significant manner (p ¼ 0.035) and there was a significant increase in TBUT values (p ¼ 0.022). Discussion and conclusion: The use of antiHT drugs containing diuretics had no adverse effect on the tear function tests, but using drugs that contain ACE/ARB could have a positive impact. (Emine Kalkan Akcay 2014)
Dry Eye Syndrome Due to Hormonal Changes
The endocrine system influences all tissues and cells in the human body. The ocular surface is constantly exposed to circulating hormones and expresses their specific receptors. (Craig JP, et al., 2017)
The endocrine system influences all tissues and cells in the human body. The ocular surface is constantly exposed to circulating hormones and expresses their specific receptors. (Craig JP, et al., 2017)
Dry eye disease (DED) is a disorder with multifactorial aetiology, and endocrine anomalies are one of the inciting factors. (Gilbard JP, Farris RL. 2009)
The endocrine anomalies that cause DED include physiological conditions such as menopause, menstrual cycle variations, pathologies such as polycystic ovarian syndrome, androgen resistance, and iatrogenic conditions such as contraceptive use, and antiandrogen treatment. (Bonini S et al., 2007)
This review highlights the status of these hormones in DED along with the mechanism of action of different hormones on the ocular surface structures and the clinical implications of these effects. (Gipson IK, 2007)
The influence of androgens, oestrogens, and progesterone on the ocular surface tissues and the implications of androgen-deficient states in DED are also discussed. The physiological and pathological effects of menopause and sex hormone replacement therapy are discussed. (Hashemi H, et al., 2014)
The effects of insulin and insulin resistance on the ocular surface and DED and the growing potential of topical insulin therapeutics for DED are mentioned. Thyroid-associated ophthalmopathy, its impact on the ocular surface, and the tissue effects of thyroid hormone in the context of DED are reviewed. (Gorimanipalli B 2023)
Finally, the potential role of hormonal therapeutics in the management of DED has also been discussed. The compelling evidence suggests that it would be clinically beneficial to consider the possibility of hormonal imbalances and their impact while treating patients with DED. (Emine Kalkan Akcay 2023)
References
- J. Shimazaki, (2018) Santen Pharmaceutical Company (F, C, R), Otsuka Pharmaceutical Company (F, R), Senju Pharmaceutical Company (F) Investigative Ophthalmology & Visual Science November 2018, Vol.59, DES7-DES12.
- Sadiya Farhat J. P et al., (2015) world journal of pharmacy and pharmaceutical sciences, Volume 10, Issue 9, 1448-1462, Department of Pharmaceutics, Karnataka College of Pharmacy, Bangalore 560064, India
- Golden MI, et al., (2023) Dry Eye Syndrome. https://www.ncbi.nlm.nih.gov/books/NBK470411
- Salmon JF, (2020) Dry eye. In: Kanski's Clinical Ophthalmology: A Systematic Approach. 9th ed. Elsevier; https://www.clinicalkey.com. Accessed Aug. 4, 2020.
- Lin Zhao et al., (2016) Journal of Ophthalmology. April 2016 doi: 10.1155/2016/8201053, PMCID: PMC4861815, PMID: 27213053
- Shamsher Singh et al., (2018). Dry Eye in DM & Its Relationship with Diabetic Retinopathy, International Journal of Medical Research Professionals.
- Feng Jin et al., (2020) Prevalence of symptomatic dry eye in breast cancer patients undergoing systemic adjuvant treatment: A cross-sectional study Breast. 53: 164–171.
- Craig JP, et al., (2017). TFOS DEWS II definition and classification report. Ocular Surface. 15: 276–83.
- Gilbard JP, Farris RL. (2009). Ocular surface drying and tear film osmolarity in thyroid eye disease. Acta Ophthalmol (Copenh). 61:108–16.
- Bonini S et al., (2007). A. Itchy-dry eye associated with polycystic ovary syndrome. Am J Ophthalmol. 143: 763–71. e2.
- Gipson IK. (2007). The ocular surface: The challenge to enable and protect vision: The Friedenwald lecture. Investigation Ophthalmology Vis Science 48: 4391.
- Hashemi H, et al., (2014). Prevalence of dry eye syndrome in an adult population. Clinical Experiment Ophthalmology 2014; 42:242–8.
- Gorimanipalli B, Khamar P, Sethu S, Shetty R. (2023). Hormones and dry eye disease. Indian Journal of Ophthalmology. 71(4): 1276-1284.
- Emine Kalkan Akcay, Murat Akcay, Gamze Dereli Can, Nabi Aslan, Betul Seher Uysal, Basak Bostanci Ceran, Pinar Koseahya, and Nurullah Cagil, Department of Ophthalmology, (2023). Yildirim Beyazit University Medical Faculty Ankara Ataturk Training and Research Hospital, Ankara, Turkey.
Citation: K. Priya and Dr. J. Bagyalakshmi. (2024). Causes of Dry Eye Syndrome. Journal of Pharmacy and Drug Development 6(1).
Copyright: © 2024 K. Priya. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.