Case Report
Volume 2 Issue 2 - 2020
Burkholderia Pseudomallei: A Complicated, Potentially fatal, Case of Melioidosis with a Proposed Management Regimen
1MD, FACS, FASCRS, Attending Surgeon, Houston Methodist Specialty Group, Methodist Sugar Land Colon & Rectal Surgery, USA
2Baylor University, USA
3MD, Houston Methodist Hospital, USA
4Attending Surgeon, Department of Vascular Surgery, Department of Cardiovascular Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 500, Sugar Land, TX 77479, USA
5Attending Surgeon, Division of Infectious Disease, Department of Internal Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 430, Sugar Land, TX 77479, USA
6Attending Surgeon, Division of Infectious Disease, Department of Internal Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 430, Sugar Land, TX 77479, USA
2Baylor University, USA
3MD, Houston Methodist Hospital, USA
4Attending Surgeon, Department of Vascular Surgery, Department of Cardiovascular Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 500, Sugar Land, TX 77479, USA
5Attending Surgeon, Division of Infectious Disease, Department of Internal Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 430, Sugar Land, TX 77479, USA
6Attending Surgeon, Division of Infectious Disease, Department of Internal Medicine, Houston Methodist Hospitals System, 16605 Southwest Freeway, Suite 430, Sugar Land, TX 77479, USA
*Corresponding Author: Ali Mahmood, MD, FACS, FASCRS, Attending Surgeon, Houston Methodist Specialty Group, Methodist Sugar Land Colon & Rectal Surgery, USA.
Received: May 27, 2020; Published: June 10, 2020
Abstract
We present an unusual case and management plan for a complicated case of Burkholderia Pseudomallei. A 75 year old male travelled to the United States from Southeast Asia, and presented acutely to the emergency room with fevers and difficulty breathing. He was diagnosed with a pulmonary embolus, following radiological imaging. Concurrently, with his acute presentation, he was found to have an underlying infection, diagnosed to be from Burkholderia Pseudomallei. He was treated initially with intravenous antibiotics and sent home with a prolonged regimen of oral antibiotics. Despite being on antibiotics, and being completely asymptomatic, he seeded the infection to his vascular graft. This was placed via endovascular technique to treat a ruptured right ileac artery aneurysm. The graft was placed well after the infection was diagnosed and treated. This bacteria is endemic to Southeast Asia, however, with global travel, the prevalence is increasing in multiple different countries and continents. A brief detailed review of Burkholderia Pseudomallei was undertaken and presented, along with a management plan for addressing the abdominal vascular infection. It is important for the clinician to maintain an index of suspicion in the setting of patient presentation, occupation, recent travel and both radiological and pathological findings.
Keywords: Burkholderia Pseudomallei; Melioidosis; Graft Infection; Liver Abscess; Spleen Abscess; Southeast Asia
Case Presentation
We present a complicated case of Burkholderia pseudomallei. The patient is a 75 year old male of Vietnamese origin who presented to the hospital emergency room with complaints of fever and shortness of breath, following a flight from Vietnam. He was found to have an embolus in the distal main pulmonary arteries, affecting the right upper lobe. (Figure 1)
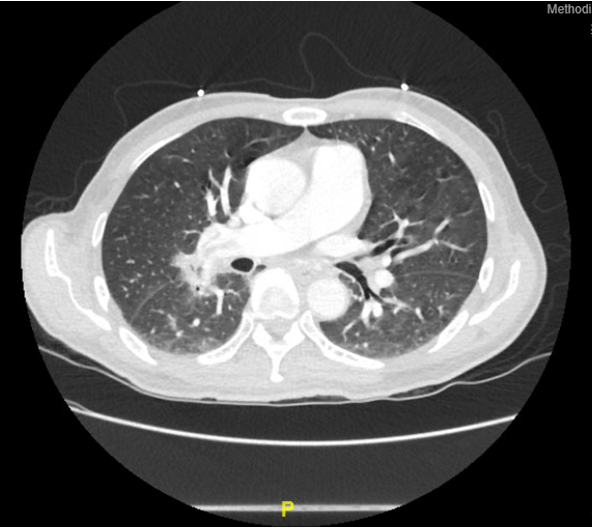
Figure 1: CT scan of the chest showing the significant filling defect, along with multiple lymphadenopathy.
Upon presentation he was hypoxic, with an oxygen saturation of 89% on room air, and an arterial oxygen concentration of 68 on his arterial blood gas. His comorbidities included diabetes and hypertension. The patient was admitted to the intensive care unit. Subsequent imaging was performed, which revealed hilar lymphadenopathy with hilar infiltrates and a small mass. Biopsy of the multiple pleural lesions revealed a diagnosis of Burkholderia Pseudomallei. The patient was placed on flurouquinolones and sulfamethoxazole/trimethoprim. The sulfamethoxazole/trimethoprim (Bactrim ®) duration was for 1 year.
The patient responded well, became asymptomatic, however upon cessation of the antibiotics, he developed fevers again. The workup did not reveal any etiology. He was placed back upon the same antibiotic regimen, and his fever disappeared. There were not any other symptoms.
Approximately 2 months later, he developed pain in the right lower quadrant, along with the right groin. Diagnostic workup revealed a contained rupture of a right iliac artery pseudoaneursym. (Figure 2) This was repaired using a covered stent. (Figure 3)

Figure 2: CT scan of the abdomen and pelvis depicting the large pseudo-aneurysm with contained rupture.
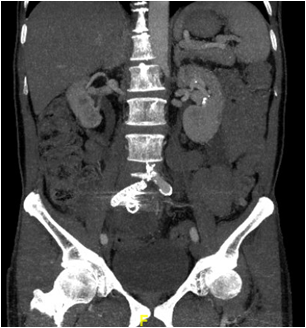
Figure 3: CT scan of the abdomen and pelvis (coronal cross section) showing the repair of the aneurysm.
6 months after the repair of his right iliac vascular pathology, the patient presented to the hospital with high fevers. The patient also had swelling of the right knee, concurrently. MRI revealed fluid around the knee that was subsequently aspirated and sent for cultures. There was not any growth reported. Repeat abdominal imaging showed that the graft site of the right iliac was inflamed with fluid circumferentially surrounding the graft site with the sigmoid colon juxtaposed to the graft site. (Figure 4).
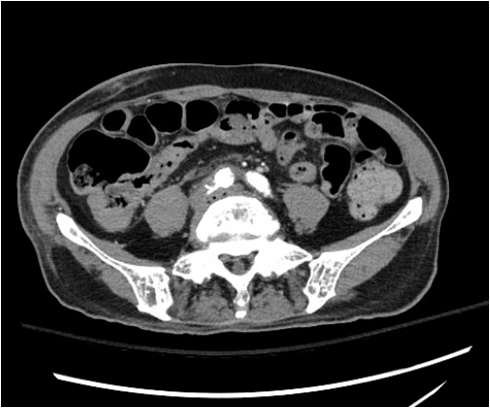
Figure 4: CT scan of the abdomen and pelvis showing the aneurysm, with significant air pockets and fluid around.
We recommended resection of the infected graft. We furthermore recommended resection of the sigmoid colon and creation of a colostomy. We further recommended an extra anatomic bypass to perfuse the right lower limb. A femoral-femoral graft, or an axillary-femoral bypass was proposed to ensure blood supply to the right limb, and concurrently provide flow to the right pelvis as well.
Discussion
Burkholderia is a gram negative bacteria. These are opportunistic pathogens, in particular Burkholderia pseudomallei. The bacteria do possess an outer membranous layer that does impede antibiotics. This lipopolysaccharide capsule is attributed for their polymyxin resistance. Some forms of the bacteria also have altered DNA gyrase, and dihydrofolate reducatase targets that contribute to antibiotic difficulty and resistance. [1]
Burkholderia pseudomallei is a bacteria that is relative rare in the North America. Historically this disease has seen prominence is Southeast Asia. One of the larger studies published looked at data form Thailand, where 7126 cases were identified. [2] The distribution pattern was 5475 cases in Northeast Thailand, 536 cases in Central Thailand, 374 cases is South Thailand, 364 cases in East Thailand, 358 cases in North Thailand and 19 cases appreciated in west Thailand. This was in concordance with the agricultural and farming distribution of the economic landscape. Endemic to soil and surface water, the disease process presents with various manifestations, ranging from abdominal abscesses, subcutaneous abscesses, pneumonia, osteomyelitis, and endocarditis to name a few. [3,4]
The majority of patients presenting in that part of the world are agricultural workers. The mortality was very impressive in some studies, ranging between 39-50%. [3,5] Annual mortality numbers have been reported to be 89,000. A second large study, evaluating 10,175 patients over 25 years correlated the increased severity and mortality of disease in the immunocompromised population. [4] The patient population with the biggest risk factors, to no surprise, was the immunocompromised. [4-6] Diabetes and cystic fibrosis accounted for a significant impact of both mortality and morbidity of the disease process.
The diabetic patients were more prone to pneumonia (35.7%), intra-abdominal abscesses (18.3%) and sepsis (18%). [4-6]. another separate study attributed diabetes to a twelve fold increase in infectious susceptibility to Burkholderia pseudomallei. [7] From a molecular standpoint, high titers of CD8+ and NK cells were determined to be of significant importance in fighting B. pseudomallei. 8 Social habits have also contributed to the increased morbidity and mortality, with an Australian study finding a correlation between excessive alcohol abuse and increased severity of disease. [9] There have been links to animals, with a specific swine Melioidosis uncovered in Southern Thailand. [10] This form of the disease was isolated in a slaughter house, where the animals of origin were thought to be originated from one farm. This finding underscored that contaminated soil and/or water are usually the media for bacterial proliferation, however animals can serve as a vetor. The majority of the bacteria, however, have been found to live in soil, rice rhizosphere and water.11
The proliferation of Melioidosis was further seen to spread globally, especially following natural disasters, including the US Virgin Islands in late 2017. [12] Hurricanes Irma and Maria were followed by several isolated cases, however these were definitively greater than the usual number for that region. In Guadeloupe, French West Indies, there were only 2 cases reported from 1997 to 2017. [13] Following the excessive and extensive hurricane damage in 2017, there were 3 cases confirmed. We do, however, realize that testing for Melioidosis has improved and become more readily available over the last decade. In Brazil, there were 28 reported cases, with geographic spread form the Northwest region to the central part of the country. [14]
The disease does have an affinity towards adults, however it has been described in children as well. Over a 12 year span, a study was undertaken in Southern Thailand to examine the pediatric population. [15] There were 27 confirmed cases of Melioidosis. The incidence of splenic and hepatic abscesses was higher in children than adults, with also a preponderance of subcutaneous skin infections. Authors advocated that the presence of visceral abscesses, in particular the liver and/or spleen coupled with a cutaneous infection, be empirically treated as Melioidosis until proven otherwise.
The clinical presentation of Melioidosis can vary dramatically. Relative to the pathology, the disease entity can present from fevers to vague abdominal pain, to significant cutaneous lesions. One study found that global travel often created a misdiagnosis, as high as 21%, given the unfamiliarity of this disease process outside of Southeast Asia. [2-5] Presentation in the lungs can mimic bronchogenic carcinoma, mediastinal lymphadenopathy, and even patchy infiltrates, as in our patient. [16] Computed Tomography (CT) is the imaging modality of choice to help obtain a diagnosis. The definitive diagnostic test is pathological proven microbiology.
Treatment regimens have varied depending on geographic prevalence. Intravenous Meropenem, followed by oral sulfamethoxazole/trimethoprim and/or doxycycline have been administered with success. There is a certain species of Burkholderia, Burkholderia cepacia that is much more prevalent in the cystic fibrosis population. [17] Addition of low dose colistin to a regimen of moxifloxacin-ceftazidime have been to shown to increase efficacy. There was also a case report reported where gentamicin was used with moderate success in a patient with B. pseudommalei infective endocarditis with septic emboli to the brain. [18] The treatment duration is variable, with long term antibiotic usage, this can range from months to a year.
Interestingly, one epidemiological study found that inoculation and exposure to Burkholderia thailandensis, a less virulent bacteria of the same genus, conferred cellular immunity to Burkholderia pseudomallei, melioidosis. [19] This has led to investigating if a vaccine can be made. Although a human vaccine has yet to be introduced, there does exist evidence that CD8+ cells are involved in the immunological response, in humans. A study did examine the response in the animal model. The multi-component vaccine, a combination of glycoconjugates, live-attenuated, and/or inactive bacteria would need to be introduced to induce an antibody response and confer immunity.
Our patient presented with an acute abdominal infection to the graft, well after the initial infection had been diagnosed and treated. He had been on oral antibiotics for well over a year, without showing any signs of symptoms of a continual infectious process. Nevertheless, he seeded his graft site. Our management regimen involved the resection of the infected aneurysm and graft. This was performed concurrently with the resection of the sigmoid colon. The patient received a colostomy, with the distal rectum marked, with non absorbable suture, for future Hartmann’s reversal. We advocate performing a colostomy over a primary intracorporeal anastomosis because there exists an underlying infection inside the abdominal and pelvic cavity. This would predispose the anastomosis to an infection and potentially increase the chances of an anastomotic leak. The vasculature to the right hemipelvis was ensured with a femoral-femoral crossover bypass graft. The patient did exceedingly well and was discharged home within 5 days.
- Rhodes KA, Schweizer HP. (2016). Antibiotic resistance in Burkholderia species. Drug Resist Updat. 28: 82-90.
- Hantrakun V, Kongyu S, Klaytong P, Rognsumlee S, Day NPJ, Peacock SJ, Hinjoy S, Limmanturotsakul D. (2019). Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the implications for a National Notifiable Diseases Surveillance System. Open Forum Infect Dis. 6(12): 498.
- Tang RY, Lim SH, Lam JE, Nurasykin S, Eileen T, Chan YW. (2019). A 5-year retrospective study of melioidosis cases treated in a district specialist hospital. Med J Malaysia. 74(6): 472-6.
- Birnie E, Virk HS, Savelkoel J, Spijker R, Bertherat E, Dance DAB, Limmathurotsakul D, Devleesschauwer B, Haagsma JA, Wiersinga WJ. (2019). Global burden of melioidosis in 2015: a systemic review and data synthesis. 19(8): 892-902.
- Morici L, Torres AG, Titball RW. Novel multi-component vaccine approaches for Burkholderia pseudomallei. Clin Exp Immunol. 2019; 196(2): 178-88.
- Birnie E, Savelkoel J, Reubsaet F, Roelofs JJTH, Soetekouw R, Kolkman S, Cremers AL, Grobusch MP, Notermans DW, Wiersinga WJ. (2019). Melioidosis in travelers: An analysis of Dutch melioidosis registry data 1985-2018. Travel Med Infect Dis. 101461.
- Le Tohic S, Montana M, Koch L, Curti C, Vanelle P. (2019). A review of melioidosis cases imported into Europe. Eur J Clin Microbiol Infect Dis. 38(8): 1395-1408.
- Kronsteiner B, Chaichana P, Sumonwiriya M, Jenjaroen K, Chowdhury FR, Chumseng S, Teparrukkul P, Limmanthurostsakul D, Day NPJ, Klenerman P, Dunachie SJ. (2019). Diabetes alters immune response patterns to acute melioidosis in humans. Eur J Immunol. 49(7): 1092-1106.
- Chakrovorty A, Heath CH. (2019). Melioidosis: An updated review. Aust J Gen Pract. 48(5): 327-332.
- Kwanhian W, Jiranantasak T, Kessler AT, Tolchinsky BE, Parker S, Songsri J, Wisessobat S, Pukanha K, Testamenti VA, Khrongsee P, Sretrirutchai S, Kaewrakmuk J, Tangpong J, Tuanyok A. (2020). Investigation of Melioidosis Outbreak in Pig Farms in Southern Thailand. Vet Sci. 7(1).
- Seng R, Saiprom N, Phunpang R, Baltazar CJ, Boontawee S, thodthasri T, Silakun W, Chantratita N. (2019). Prevalence and genetic diversity of Burkholderia pseudomallei isolates in the environment near a patient’s residence in Northeast Thailand. PLoS Negl Trop Dis. 13(4).
- Guendel I, Ekpo LL, Hinkle MK, Harrison CJ, Blaney DD, Gee JE, Elrod MG, Boyd S, Gulvik CA, Liu L, Hoffmaster AR, Ellis BR, Hunte-Ceaser T, Ellis EM. (2019). Melioidosis after Hurricanes Irm and maria, St. Thomas/St. John District, US Virgin Islands, October 2017. Emerg Infect Dis. 25(10): 1952-55.
- Melot B, Bastian S, Dournon N, Valade E, Gorge O, Le Fleche A, idier C, Vernier M, Fernandes E, Hoen B, Breurec S, Carles M. (2020). Three New Cases of Melioidosis, Guadeloupe, French West Indies. Emerg Infect Dis. 26(3): 617-619.
- Volpe-Chaves CE, Rodrigues ACS, Lacerda MLGG, Oliveira CTF, Castilho SB, Franciscato C, Santos ICO, Assef APDC, Roever L, Oliveira SMDVL, Paniago AMM. (2019). Melioidosis, an emerging infectious disease in the Midwest Brazil: A case report. Medicine (Baltimore). 98(16).
- Chanvitan S, Geater A, Laoprasopwattana K. (2019). Hepatic/splenic abscess and/or skin and soft tissue infection as predictors of melioidosis in children. J Infect Dev Ctries. 13(2): 149-153.
- Zhao J, Yap A, Wu E, Yap J. (2020). A mimic of bronchogenic carcinoma – pulmonary melioidosis. Respir Med Case Rep. 29.
- El-Halfawy OM, Naguib MM, Valvano MA. (2017). Novel antibiotic combinations proposed for treatment of Burkholderia cepacia complex infections. Antimicrob Resist Infect Control. 6: 120.
- Sia T, Podin Y, Chuah TB, Wong JS. (2018). Melioidosis: an unusual cause of infective endocarditis: a case report. Eur Heart J Case Rep. 2(2).
- Rongkard P, Kronsteiner B, Hantrakun V, Jenjaroen K, Sumonwiriya M, Chaichana P, Chumseng S, Chantratita N, Wuthiekanun V, Fletcher HA, Teparrukkul P, Limmathurostsakul D, Day NPJ, Dunachie SJ. Emerg Infect Dis. 2020; 26(3): 463-471.
Citation: Ali Mahmood., et al. (2020). “Burkholderia Pseudomallei: A Complicated, Potentially fatal, Case of Melioidosis with a Proposed Management Regimen”. Journal of Medicine and Surgical Sciences 2.2.
DOI: 10.5281/zenodo.3903488
DOI: 10.5281/zenodo.3903488
Copyright: © 2020 Ali Mahmood. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
