Case Report
Volume 4 Issue 1 - 2022
Bilateral Sinonasal Inverted Papilloma
Department of Otorhinolaryngology – Head and Neck Surgery Rizal Medical Center, Pasig City
*Corresponding Author: Peter John F. Carabeo MD, Department of Otorhinolaryngology – Head and Neck Surgery Rizal Medical Center Barangay Bagong-Ilog, Pasig City.
Received: March 09, 2022; Published: March 21, 2022
Abstract
A case of Inverted Papilloma in a 30-year old male initially presenting with a unilateral nasal obstruction. Endoscopic examination revealed bilateral exophytic fleshy mass with attachments to the turbinates. Surgical resection of the intranasal mass from its attachments was done and was submitted for histopathologic analysis. Final biopsy result from bilateral intranasal masses revealed slides showing squamous metaplastic changes to transitional epithelium pushed deep within their underlying connective tissue stroma, classic for inverted papilloma. This report highlights the case of bilateral inverted papilloma. This also shows the importance of meticulous pre-operative and intraoperative examination, possibly saving this patient from an aggressive recurrence of the disease.
Keywords: Inverted papilloma; Inverting papilloma; Schneiderian papilloma; Bilateral intranasal mass
Introduction
Sinonasal inverted papilloma, also known as Schneiderian papilloma is a rare, benign tumor that is locally aggressive and has the propensity for malignant transformation in up to 15% of the cases. Typically, it would present as a unilateral nasal obstruction associated with sinusitis and epistaxis, localized mainly on the lateral nasal wall. [2] However, atypical presentations such as frontal or sphenoid location and bilateral involvement have been reported. [3] Although it is recognized as a benign lesion, the goal of treatment is complete surgical resection primarily due to its tendency for malignant transformation and recurrence. [4] This study aims to describe an atypical presentation of inverted papilloma.
Objectives
- To report a case of an atypical presentation of inverted papilloma
- To discuss the importance of recognition and adequate management for a case of bilateral inverted papilloma
vMethodology
Study Design: Case Report
Setting: Tertiary government hospital Patient: One (1)
Study Design: Case Report
Setting: Tertiary government hospital Patient: One (1)
Ethical Considerations
An informed consent from the patient was obtained. IRB exemption has been approved.
An informed consent from the patient was obtained. IRB exemption has been approved.
Case Presentation
A 30-year old male, sought consult at the ENT out-patient department of a tertiary government hospital due to left nasal obstruction. A year prior to initial consult, the patient noted a firm left intranasal mass that occasionally bleeds upon finger manipulation. This was associated with left intranasal obstruction and occasional thick, mucoid, non-foul smelling nasal discharge. There was no consultation done and no medication was taken at this time. However, due to progression of symptoms, the patient decided to seek ENT consultation. The Filipino Sino-nasal Outcome Test (SNOT) score on initial consult was noted to be 23.
On physical examination, inspection revealed no gross facial asymmetry or bulges. Nasal endoscopy revealed a fleshy intranasal mass in the left nasal cavity, with thick white discharge predominantly seen on the nasal floor with attachments noted at the inferior turbinate (Figure 1). Upon insinuation of the rigid 30 degree nasal endoscope, a mass of the same characteristic was also noted with attachments to the left middle turbinate which easily bleeds upon minimal contact with the instrument. The nasal endoscopy on the right nasal cavity revealed a smaller fleshy polypoid mass appreciated on both antero-inferior and postero-inferior portions of the right middle turbinate (Figures 2). The rest of the ENT examination was unremarkable.
Contrast-enhanced paranasal CT scan done revealed soft tissue densities on the left nasal cavity with attachments noted on both the inferior and middle turbinates. Minimal soft tissue densities of the same quality were also noted on the right middle turbinate but cannot be totally differentiated from possible mucosal inflammation. Unfortunately, the common finding of hyperostosis on the attachment of the intranasal inverting papilloma was not appreciated in the scan due to the low quality of CT scan done in another facility. Punch biopsy of the left intranasal mass was done which revealed histologic findings consistent with Inverted Papilloma. Hence, surgical intervention was then advised.
Intraoperatively, endoscopic partial medial maxillectomy on the left was done, with the fleshy, exophytic mass resected from its attachments to the inferior and middle turbinates. On the right nasal cavity, resection of the fleshy, exophytic mass with attachments to the right middle turbinate was also done. Final histopathological examination of tissue fragments from both nasal cavities revealed a lining by pseudostratified, ciliated epithelium with a focus exhibiting squamous metaplastic changes and a few foci of well-circumscribed nests of benign squamous epithelium to transitional epithelium pushed deep within the stroma (Figure 3), all of which are consistent with histopathologic findings for Inverted Papilloma.
Discussion
Sinonasal Inverted Papilloma is a benign but locally aggressive tumor first reported by Ward in 1854. It was later in 1938 that Ringertz et al. identified its endophytic growth pattern with a characteristic tendency to invert into its underlying connective tissue stroma hence the name inverted papilloma (IP). It is rare and only accounts for about 0.5 to 4% of all primary nasal tumors. The most common presenting symptom of IP is a unilateral intranasal obstruction associated with persistent nasal discharge and epistaxis, in which malignancy should also be of consideration especially in the elderly. [5] Along with malignancy, differential diagnoses include sinonasal polyps, and inverted papilloma, among a number of other possible considerations. Excision of the intranasal mass which will also serve as histopathologic analysis is a common occurrence in a tertiary hospital especially if malignancy is unlikely and if a pre-operative biopsy becomes difficult especially for indigent patients. Although the patient in the case presented is in the younger age group, the managing team decided to do a punch biopsy of the left intranasal mass due to possible malignant clinical features exhibited. Biopsy results then revealed microscopic findings consistent with Inverted Papilloma. Histologically, IP will show an endophytic growth pattern consisting of hyperplastic epithelial proliferation growing downward to the underlying connective tissue stroma. Epithelium may be composed of squamous, transitional and columnar cells or a mixture of all three. [6] Consideration of IP instead of a more benign inflammatory polyp despite its bilateral presentation may have saved this patient from morbid complications and recurrence.
In a study by Tomazic et al., recurrence of inverted papilloma was diagnosed in 29.2% of the cases that underwent surgical management. Recurrence rate was also noted to be significantly higher after a revision surgery which highlights the importance of removing the tumor completely during the first surgery. [7] Complete surgical removal of the intranasal mass and meticulous identification of its attachments under direct visual control is the goal of treatment for IP. [4] In this case, the final histopathologic diagnosis showed bilateral inverted papilloma.
This report highlights the atypical presentation of inverted papilloma and shows the importance of meticulous preoperative and intraoperative examination, possibly saving this patient from the dreaded malignant transformation and an aggressive recurrence of the disease.
Appendix
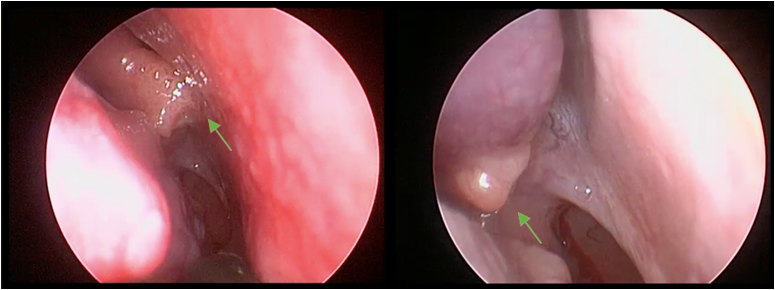
Figure 2: Endoscopic picture of the exophytic fleshy mass on the right intranasal cavity with attachments to the middle turbinate (green arrow).
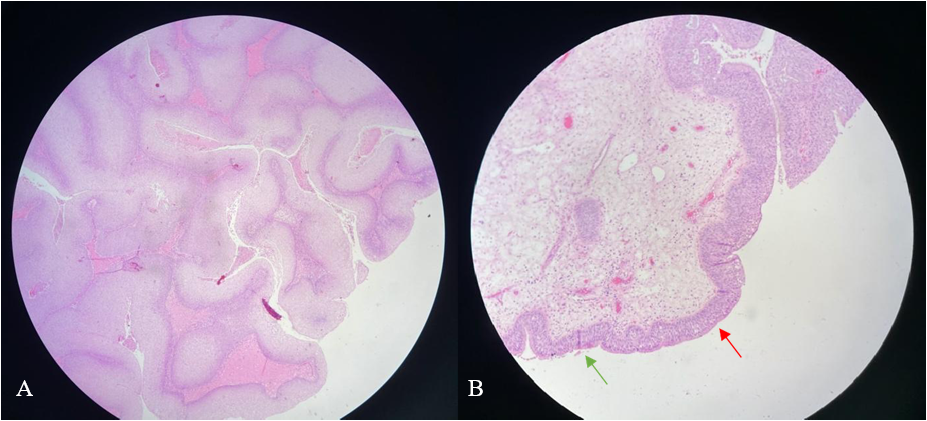
Figure 3: A) Scanner view of tissue fragment from the left intranasal mass, showing nests of hyperplastic epithelial cells extending into the stroma which is a classic histopathologic finding in inverted papilloma. B) Low power objective view of tissue fragment from the right intranasal mass, showing ciliated epithelium (green arrow) transitioning to more polygonal cells without cilia (red arrow).
References
- Govindaraj, S., & Wang, H. (2014). Does human papilloma virus play a role in sinonasal inverted papilloma? Current Opinion in Otolaryngology & Head and Neck Surgery, 22(1), 47-51.
- Upadhyaya, N., Khandekar, S., Dive, A., & Mishra, R. (2015). Sinonasal inverted papilloma: A case report and mini review of histopathological features. Journal of Oral and Maxillofacial Pathology, 19(3), 405.
- Akkari, M., Lassave, J., Mura, T., Gascou, G., Pierre, G., Cartier, C., … Crampette, L. (2016). Atypical presentations of Sinonasal inverted papilloma: Surgical management and influence on the recurrence rate. American Journal of Rhinology & Allergy, 30(2), 149- 154.
- Mackle, T., Chambon, G., Garrel, R., Meieff, M., & Crampette, L. (2008). Endoscopic treatment of sinonasal papilloma: A 12 year review. Acta Oto-Laryngologica, 128(6), 670- 674.
- Wassef, S. N., Batra, P. S., & Barnett, S. (2012). Skull base inverted papilloma: A comprehensive review. ISRN Surgery, 2012, 1-34.
- Upadhyaya, N., Khandekar, S., Dive, A., & Mishra, R. (2015). Sinonasal inverted papilloma: A case report and mini review of histopathological features. Journal of Oral and Maxillofacial Pathology, 19(3), 405.
- Tomazic PV, Hubmann F, and Stammberger H. (2015). The problem of high recurrence rate in endoscopic revision surgery for inverted papilloma [in German with English abstract]. Laryngorhinootologie 94:447–450.
Citation: Peter John F. Carabeo, Rodante A. Roldan, Giancarla Marie C. Ambrocio. (2022). Bilateral Sinonasal Inverted Papilloma. Journal of Otolaryngology - Head and Neck Diseases 4(1). DOI: 10.5281/zenodo.6379121
Copyright: © 2022 Peter John F. Carabeo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

