Case Report
Volume 4 Issue 1 - 2022
Aggressive Periodontitis: Source of Peri-implant Infectious Tissues which Solution We Try to Adapt?
Université Saad Dahlab of Blida, Algeria
*Corresponding Author: Saoudi Fadila, Université Saad Dahlab of Blida, Algeria.
Received: March 12, 2022; Published: March 25, 2022
Abstract
Periodontal and peri-implant pathologies have a recognized infectious origin. The logical therapeutic approach will be etiological and its objective will aim to reduce or eradicate, not the periodontal flora as a whole, but its pathogenic component. Microbiology is nowadays a means of diagnosis, which makes it possible to highlight pathogenic bacteria, in periodontal pockets.
This one seems judicious in order to better prevent peri-implantitis in subjects that already had periodontitis in the past on one hand and on the other, in order to better target the treatment. The bacterial culture technique will be improved to explain some precautions to take in order to avoid the loss of some implants.
We will add to these statistics realized on a sample of 21 patients in a region at west of Algiers i.
Dr SAOUDI. F CHU Beni Messous; Pr BOUZIANE.D(ORAN)
Dr SAOUDI. F CHU Beni Messous; Pr BOUZIANE.D(ORAN)
PLAN
1_Introduction
2_Peri-implant tissues
2-1_ Definition
2-2_Biology reminder
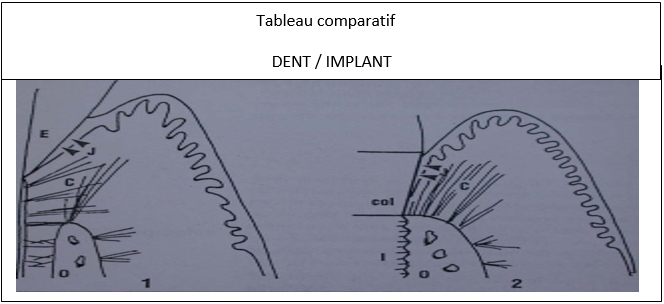
2-3_Comparative table tooth/ implant
3_Peri-implantitis
3-1_Definition
3-2_Clinical aspects related to peri-implantitis
3-3_Radiological interpretation
4_Pathophysiological concepts of peri-implantitis
_Mechanical concepts
_Infectious concepts
_Prevention of peri-implantitis
_Clinical monitoring
_Radiological monitoring
_decrease of factors favoring peri-implantitis
_Treatement of peri-implantitis
_Maintenance
_Conclusion
2_Peri-implant tissues
2-1_ Definition
2-2_Biology reminder
2-3_Comparative table tooth/ implant
3_Peri-implantitis
3-1_Definition
3-2_Clinical aspects related to peri-implantitis
3-3_Radiological interpretation
4_Pathophysiological concepts of peri-implantitis
_Mechanical concepts
_Infectious concepts
_Prevention of peri-implantitis
_Clinical monitoring
_Radiological monitoring
_decrease of factors favoring peri-implantitis
_Treatement of peri-implantitis
_Maintenance
_Conclusion
Introduction
In 20 years, dentistry has changed in a revolutionary way. No more-old dental bridges, no more unsightly unstable dentures, to let spend the night in a glass of water. However, throughout the treatments which consist of the placement of implants, even in subjects not presenting any general pathology, the concern of any practitioner is that it doesn’t occur inflammatory or infectious damage around the Implant (peri-implantitis).
Peri-Implant Tissues
Dental implants first appeared in the 1980s and are often a therapeutic solution of choice. This helps to give patients the feeling of having kept their natural teeth.
Dental implants first appeared in the 1980s and are often a therapeutic solution of choice. This helps to give patients the feeling of having kept their natural teeth.
Definition
The dental implant is an artificial root, anchored in the jaw bone. It is used to replace the root of a damaged or torn tooth and to support a prosthesis. The dental implant is the intermediary between the prosthesis and the jaw bone, it transmits the chewing forces to the bone support and acts as a shock absorber.
*types and shapes of the dentant implat :
We recognize 2types of implants
-those fixed on the jaw
-Those fixed in the jaw
Their diameter varies from 2 to 3mm and their length from 10 to 15mm.
*The resistance of the implant:
The dental implant is an artificial root, anchored in the jaw bone. It is used to replace the root of a damaged or torn tooth and to support a prosthesis. The dental implant is the intermediary between the prosthesis and the jaw bone, it transmits the chewing forces to the bone support and acts as a shock absorber.
*types and shapes of the dentant implat :
We recognize 2types of implants
-those fixed on the jaw
-Those fixed in the jaw
Their diameter varies from 2 to 3mm and their length from 10 to 15mm.
*The resistance of the implant:
An implant must withstand chewing forces of the order of 10 to 15 kg/cm2 which can be exercised in different directions, a dental implant must not deteriorate over time, nor in contact with saliva, gum tissue or other items that may be in the mouth. Metals such as lead, mercury or used for other dental care cancause an electric current (electrogalvanization) in the salivary medium.
Durability of the implant
it must exceed human longevity. Success is obtained on the one hand with very precise radiological investigations (Cone Beam) and on the other hand, thanks to the application of a rigorous method.
it must exceed human longevity. Success is obtained on the one hand with very precise radiological investigations (Cone Beam) and on the other hand, thanks to the application of a rigorous method.
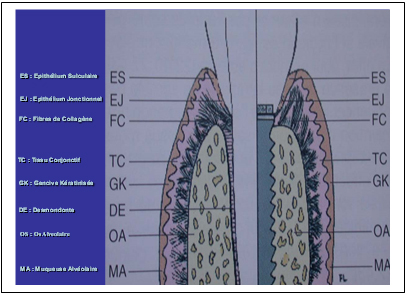
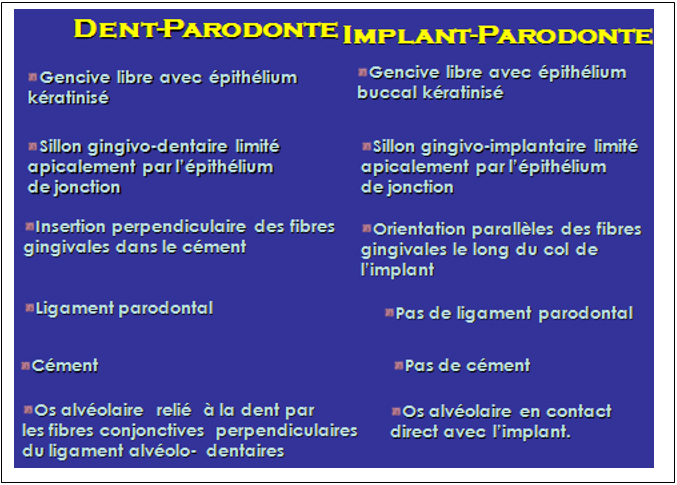
Biology reminder. Fig1-fig2:
Comparative table tooth/ implant: an implant is not a tooth, the differences are precise at the level of: soft tissues; ligament; supra –crestal fibers, vascularization. The soft tissues around the implants resemble the masticatory mucosa, are pink in color and appear to be firmly attached to the surface of the abutments.
Comparative table tooth/ implant: an implant is not a tooth, the differences are precise at the level of: soft tissues; ligament; supra –crestal fibers, vascularization. The soft tissues around the implants resemble the masticatory mucosa, are pink in color and appear to be firmly attached to the surface of the abutments.
The intrasular surface of the peri-implant mucosa presents a very characteristic appearance. Distinct from that of the sulcular gingiva. It is smooth, red, showing the vessels blood from the underlying connective tissue. Despite this fragile appearance, this tissue does not bleed. The peri-implant mucosa contains more collagens and fewer fibroblasts (Berglundh T et Al., Clinic oral ImplRes -1991; 2 :81-90).
The characteristics of the transmucosal junctional epithelium and the connectivetissue attachment of the implant becomes established during the healing of the ridgelining after surgery. Epithelial cells have the ability to stick to the surface of the implant, to synthesize abasement membrane as well as hemi-desmosomes and establish an epithelial barrierthat presents features common to the junctional epithelium.
In addition, normal connective tissue forms under the junctional epithelium andattaches to the surface of the implant.
Table: 02
There is no vascular plexus near the implants that could compensate the absence of the one of the periodontal ligaments.
Vascularization
The vascularization of the peri-implant soft tissues has only one source, those of the supra periosteal vessels of the external face of the alveolar wall. (Lindhe J et Al; periodontol2000 ?1998; 17: 47: 54).
The vascularization of the peri-implant soft tissues has only one source, those of the supra periosteal vessels of the external face of the alveolar wall. (Lindhe J et Al; periodontol2000 ?1998; 17: 47: 54).
Sometimes, and despite all the practitioner's attention to preserving the health of the implants placed, some patients even if they do not have any general disease may have inflammatory or infectious damage around the implant, this is the "periimplantitis “. Is the presence of an active pariodonal disease a risk for implants? To verify this hypothesis, the authors that carried out some microbiological studies tested by DNA probe the presence of 7 periodontogenic bacteria (Aa; Pg; Pi; Fn; Ec; Td; Cr), at periodontal sites affected by gingivitis or periodontitis, and peri-implant sites of peri-implantitis, present together in the same mouth of patients.
International scientific journal : P. Seunanèche.
Our study focused on the microbiological study in 9 patients with a total of 21 peri-Implants.
Our study focused on the microbiological study in 9 patients with a total of 21 peri-Implants.
Peri-Implantitis
1-Definition
Mombelli 1987: irreversible bacterial injury "peri-implantitis could be a site-specificinfection with ecosystems similar to periodontal disease"
Léonard 1992: Peri-implantitis is induced and develops according to the same mechanisms as periodontal disease.
Lindhe and Meyle 2008 (diagnosis of peri-implant diseases in consensus report EWOP).
Mombelli 1987: irreversible bacterial injury "peri-implantitis could be a site-specificinfection with ecosystems similar to periodontal disease"
Léonard 1992: Peri-implantitis is induced and develops according to the same mechanisms as periodontal disease.
Lindhe and Meyle 2008 (diagnosis of peri-implant diseases in consensus report EWOP).
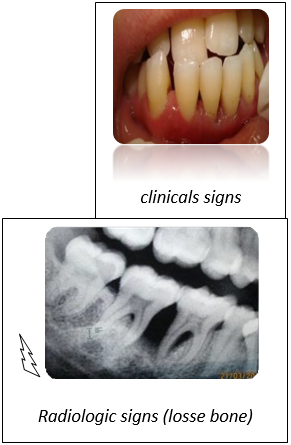
III-2: Clinical aspects of periodontitis associated with peri-implantitis:
The following clinical signs are found in all cases:
- marginal redness and edema
- bleeding on probing clinical signs
_ Increased pocket depth
_ Mobility as late sign
The following clinical signs are found in all cases:
- marginal redness and edema
- bleeding on probing clinical signs
_ Increased pocket depth
_ Mobility as late sign
_ Symmetrical and deep bone lysis with a
vertical aspect (alveolysis).
vertical aspect (alveolysis).
Aesthetic and especially biomechanical considerations oblige the practitioner to look for an ideal implant axis by omitting the microbial factor which risks compromising the stability of the implant: P. Seunanèche
In the anterior sector, horizontal bone loss requires the implementation of a heavier operating protocol (bone graft, membrane, etc.). The technique of "separation osseous”, which consists in dividing the bony crest in order to move a bony side vestibular, seems to offer the advantage of being simple without extending the time.
In the anterior sector, horizontal bone loss requires the implementation of a heavier operating protocol (bone graft, membrane, etc.). The technique of "separation osseous”, which consists in dividing the bony crest in order to move a bony side vestibular, seems to offer the advantage of being simple without extending the time.
Pathophysiological concepts of peri-implantitis
_Mechanical concepts
_Infectious concepts
_Mechanical concepts
_Infectious concepts
The implant is probably less tolerant than natural teeth. Alloufi, Bissada N; Ficara A; Faddoul F; (clinical assessment of péri-implant tissus inpatient with varing severity of chronic periodontitis. Clinic implant Relat Res 2009mard 11(11: 37-40)
Mechanical concepts
- No correlation IMPLANT/Root
- Peri-implant gingivitis
- Role of surface finish
- Role of occlusion
Infectious concept
- Implant = toothroot
- Mucositis
- Peri-implantitis
There is a direct correlation between the presence of microorganisms and the occurrence of peri-implantitis.
Peri-implantitis are associated with the presence of Gram- anaerobic bacteria according to (Léonard et al -1999; Renvert et al 2007).
Bacteriological studies were entrusted to the Pasteur Institute, an anaerobic laboratory of Dr Merad from samples taken from patients with implants for 5 to 10years and suffering from peri-implantitis have shown similar results according to the table mentioned below.
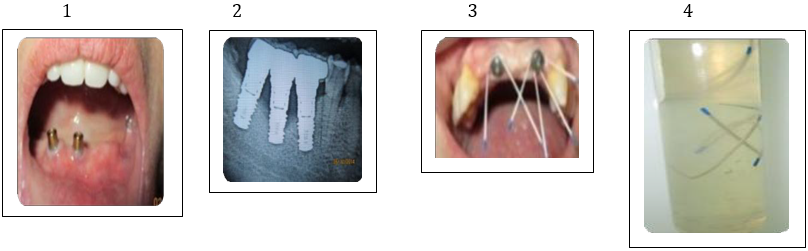
- Periimplantitis (clinical view)
- Periimplantitis (Radiological view)
- Absorbent paper cone
- Immersion of the cones in the transport medium
Results
Bacterial composition compared to the results of Papantaou in 1996:
Spirochetes and Rods (Papantaou1996); Pasteur 2014
Spirochetes and Rods (Papantaou1996); Pasteur 2014
| Bactéries | Papa Ntaou 1996 | Pasteur 2014 |
| Aa : Agregatiebacter. Actinomyces .comitans | X | - |
| Ec:Eikenella corrodens | X | X |
| Pi:Prevotella intermedia | X | X |
| Fn:Fusobacterium nucléatum | X | X |
| Pg : Porphyromonas gingivalis | X | X |
Preventions and treatments of peri-implantitis
Prevention:
All prevention aims to avoid peri-implant involvement such as:
Prevention:
All prevention aims to avoid peri-implant involvement such as:
- Clinical monitoring
- Radiological monitoring
- Reduction of factors favoring peri-implantitis.
IV-1: The Clinical surveillance consists of:
- Descaling +++
- Ensure that the following criteria are maintained at all times
- Non-inflammatory gingiva
- Pain-free survey
- No pocket
- No bleeding
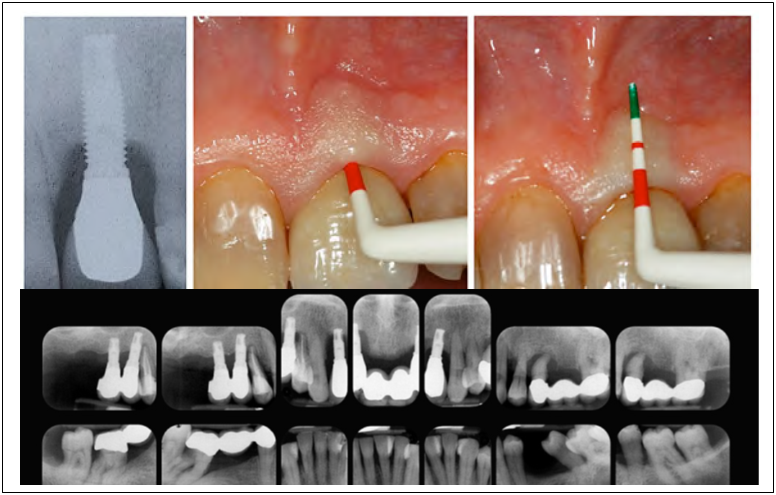
IV-2: Radiological monitoring:
- Repeated standard retro-alveolar images
- Panoramic shots
- Scanner (Beam cone)
IV-3: Factors favoring peri-implantitis
IV- 3-1: Presence of keratinized gingiva (either by free graft or adjustment afterwards).
IV- 3-2: Tobacco
IV- 3-3: the microbial flora (present before the placement of implants eg: anterior Aggressive periodontitis)
IV- 3-1: Presence of keratinized gingiva (either by free graft or adjustment afterwards).
IV- 3-2: Tobacco
IV- 3-3: the microbial flora (present before the placement of implants eg: anterior Aggressive periodontitis)
IV- 3-4: Surface condition
IV- 3-5: Diameter of the implant (incompatible with the occlusal force exerted
IV- 3-6: General condition (we only took healthy patients) according to our inclusion criteria.
3-1- The keratinized gingiva gives the superficial periodontium better resistance during food deflection.
3-2 - Tobacco: after Bruyn 94; 9% primary failure in the smoker, 1% in the non-smoker in the maxilla, no effect in the mandible.
3-3 -Microbial flora:
IV- 3-5: Diameter of the implant (incompatible with the occlusal force exerted
IV- 3-6: General condition (we only took healthy patients) according to our inclusion criteria.
3-1- The keratinized gingiva gives the superficial periodontium better resistance during food deflection.
3-2 - Tobacco: after Bruyn 94; 9% primary failure in the smoker, 1% in the non-smoker in the maxilla, no effect in the mandible.
3-3 -Microbial flora:
Bacteriological examination carried out under the same conditions as that carried out in the cases of patients with aggressive periodontitis revealed the presence of gram-anaerobic bacteria, with a predominant presence of Porphyromonas Gingivalis(PG).
3-4 / Surface finish: pure titanium
There are therefore early complications such as those occurring following traumatic surgery, and late complications due to a microbiological factor.
3-4 / Surface finish: pure titanium
There are therefore early complications such as those occurring following traumatic surgery, and late complications due to a microbiological factor.
V_ peri-implantites treatment
As part of our work, we have therefore only cared for patients with peri-implantitis, who despite preventive therapies such as:
-Choice of implant
-surface treatment
-plaque control
-control of the occlusion, presented to our consultation with clinical signs of inflammation, which justified our non-surgical treatment given the limited access to the lesion and the significant tissue penetration of the inflammation.
We followed the therapeutic approach of Mombelli 1952 which advocated descaling at that time.
- professional irrigation:
-to Clorhexidine O, 12%
- Metronidazole (flagyl) 1000 mg / day / 10 days
- patient irrigation (personal) = CHX (0.2%)
As part of our work, we have therefore only cared for patients with peri-implantitis, who despite preventive therapies such as:
-Choice of implant
-surface treatment
-plaque control
-control of the occlusion, presented to our consultation with clinical signs of inflammation, which justified our non-surgical treatment given the limited access to the lesion and the significant tissue penetration of the inflammation.
We followed the therapeutic approach of Mombelli 1952 which advocated descaling at that time.
- professional irrigation:
-to Clorhexidine O, 12%
- Metronidazole (flagyl) 1000 mg / day / 10 days
- patient irrigation (personal) = CHX (0.2%)
We have completely banned the use of:
-sonic or ultrasonic scaller
-steel curettes
-the air polisher for hydroxyapatite
-acid fluorides
-We used with care
-Titanium curettes
-Air polisher on titanium surfaces
We have privileged:
- toothbrushes
- interdental brushes
- plastic curettes
- rubber cups
- ATS: CHX at 0.12%
An occlusal analysis was performed if necessary:
-Occlusal equilibration
-Removing extensions
-Parafunction control
-Revision of the prosthetic design and in the most complex cases, surgery.
-sonic or ultrasonic scaller
-steel curettes
-the air polisher for hydroxyapatite
-acid fluorides
-We used with care
-Titanium curettes
-Air polisher on titanium surfaces
We have privileged:
- toothbrushes
- interdental brushes
- plastic curettes
- rubber cups
- ATS: CHX at 0.12%
An occlusal analysis was performed if necessary:
-Occlusal equilibration
-Removing extensions
-Parafunction control
-Revision of the prosthetic design and in the most complex cases, surgery.
Vi- Maintenance
Maintenance was the highlight of the management of péri-implantitis using non-surgical means. In the same way as Aggressive périodontitis, péri-implantitis was the subject of sub-gingival irrigation around pockets whose depth was located 3 to 4 mm using micropipettes. Regarding the benefit of maintenance in preventing loss of attachment around implants, only a few long-term studies have been published. The studies in which the maintenances are the closest (intervals of 3 to 6 months), after 18years of maintenance.
Maintenance was the highlight of the management of péri-implantitis using non-surgical means. In the same way as Aggressive périodontitis, péri-implantitis was the subject of sub-gingival irrigation around pockets whose depth was located 3 to 4 mm using micropipettes. Regarding the benefit of maintenance in preventing loss of attachment around implants, only a few long-term studies have been published. The studies in which the maintenances are the closest (intervals of 3 to 6 months), after 18years of maintenance.
Despite rigorous and correct patients monitoring, it would therefore appear that the prevalence and loss of attachment is more pronounced around implants than around teeth. It is therefore essential that implanted patients are included in an effective maintenance program.
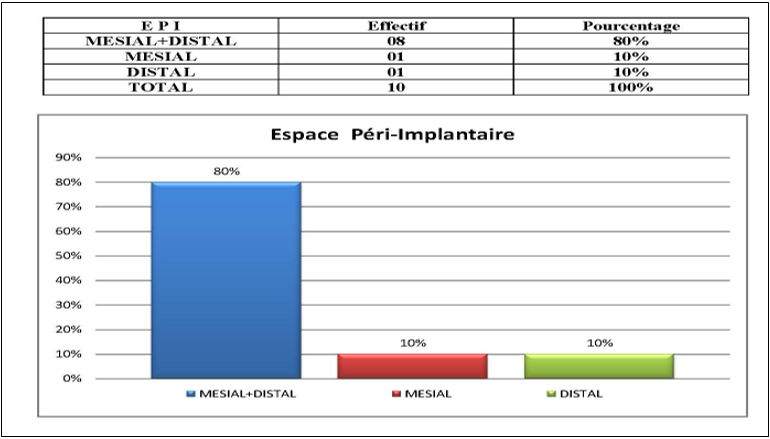
Peri-implantitis is measured radiologically by the increase in peri-implant space,visible on the radio mesial or distally to the implants. 80% of the patients who werepart of our study presented these images.
Diagnostic radiologique et clinique des péri-implantites
Séverine VINCENT-BUGNAS(NICE)
Séverine VINCENT-BUGNAS(NICE)
Conclusion
The concepts of "preventive extraction" are not supported by the literature, which motivated us more to put forward the interest of the non-surgical therapy, because the means of preventing peri-implantitis is to keep the teeth in place. maximum, even in cases of advanced periodontitis.
References
- Mombelli (1987). Treatment of péri-implantites by local delivery of tetracycline International Association for Dental rReseach (ADR) Waschinton 5- April 2000.
- Lindhe. J: texbook of clinical Périodontology, edi. Copenhagen; Munkgaard (1984): 303 -304.
- Renvert, S Badersten, A., Nilvéus,R&Egel-Berg.J (1981). Healing after treatment of périodontal intraosseous defects. Comparatif study of clinical methods journal of clinical periodontology 8, 357 -399.
Citation: F Saoudi F Chu Benimessous, Bouziane.d(oran), H Mahchouche and F Alloun. (2022). Aggressive Periodontitis: Source of Peri-implant Infectious Tissues which Solution We Try to Adapt? Journal of Oral Care and Dentistry 4(1). DOI: 10.5281/zenodo.6402139
Copyright: © 2022 Saoudi Fadila. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.