Case Report
Volume 2 Issue 1 - 2020
A Rare Case of Acute Sheehan’s Syndrome in a Young Lady with Severe Acute Symptomatic Hyponatremia following PPH
1Associate Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
2Associate Professor, Endocrinology, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
2Associate Professor, Endocrinology, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
*Corresponding Author: Dr. Richmond Ronald Gomes,Associate Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh.
Received: August 18, 2020; Published: August 28, 2020
Abstract
Sheehan’s syndrome or necrosis of pituitary gland is a rare complication of severe postpartum hemorrhage, initially described in 1937. It may cause hypopituitarism immediately or several years later, depending on the degree of tissue destruction. Sheehan’s syndrome though rare is still one of the commonest causes of hypopituitarism in developing countries like ours. We present a case of young lady with this syndrome who presented on 7th day postpartum after normal vaginal delivery with resistant acute severe symptomatic hyponatremia which was complicated by postpartum hemorrhage. She was diagnosed as Sheehan’s syndrome by clinical manifestations, laboratory tests, and magnetic resonance imaging.
Keywords: Sheehan’s syndrome; Severe postpartum hemorrhage; Hypopituitarism
Introduction
Sheehan’s syndrome which was originally described by Sheehan’s in 1937, occurs as a result of ischemic necrosis of pituitary gland due to severe postpartum haemorrhage [1]. The prevalence of Sheehan’s syndrome in 1965 was estimated to be 100- 200/100,000 women [2]. Its frequency is decreasing worldwide and it is a rare cause of hypopituitarism in developed countries owing to advances in obstetric care. It may cause hypopituitarism either immediately or after a delay of several years, depending on the degree of tissue destruction [3-5]. However, the pathogenesis of Sheehan’s syndrome is still uncertain. Enlargement of pituitary gland, autoimmunity, small sella size, and disseminated intravascular coagulation (DIC) have been considered as important factors in the pathogenesis of Sheehan’s syndrome. The clinical manifestation of Sheehan’s syndrome varied from nonspecific symptoms like weakness, anemia, and fatigue to severe pituitary dysfunction resulting in coma and even death. Medical history of postpartum hemorrhage, failure to lactate, and cessation of menses are helpful clues to the diagnosis [6]. Early diagnosis and adequate medical treatment are crucial to reduce morbidity and mortality of the disease.
Case Presentation
A 28-year-old woman (gravida 1, para 0) gave birth to a healthy female infant through normal vaginal delivery at 38th weeks of gestation by midwife at home 2 days back. The patient had no notable medical or family history and had not experienced problems during the course of her pregnancy. She developed a massive hemorrhage at the time of delivery and transferred to the gynecology and Obstetrics department our hospital for emergency treatment. Here she was diagnosed as a case of hypovolemic shock secondary to massive post-partum hemorrhage due to retained placenta. After admission she was resuscitated with isotonic fluid, six units of whole blood and uterotonic therapy. After being hemodynamically stable, she was discharged on 4th day of her hospitalization. On the next day, she again presented in the A&E department of our hospital with the complaints of headache for 12 hours with vomiting for several times.
On query, the headache was mild in nature & associated with several episodes of vomiting, but not associated with fever, photophobia, phonophobia, any visual impairment. She has no previous history of migraine or head trauma. On general examination, she was hemodynamically stable with BP 90/60 mm of H with no postural drop, bedside RBS was 4.0 mmol/l. On Nervous system examination, she was oriented regarding time, place or person with GCS 15/15. All other systematic examinations including detailed neurological examinations including fundoscopy revealed no abnormalities. On Investigation, hemogram liver function tests, serum creatinine, all were normal but her serum electrolytes revealed sodium 111 mmol/l, potassium & chloride were within the normal range. As there were no signs of severe hyponatremia e.g: neurological involvement, we started her with isotonic normal saline (0.9% NaCl) rather than hypertonic normal saline (3% NaCl). Despite giving sodium chloride replacement, on her 2nd day of hospitalization, she developed a single episode of generalized tonic clonic seizure and became comatose. This time, repeat neurological examination revealed altered sensorium with GCS 9/15. She wasn’t oriented to time, place & person. But she lacked signs of meningeal irritation.
Her motor & sensory examinations revealed no abnormalities. Repeat Serum electrolytes revealed Sodium 98 mmol/l with normal potassium and chloride. Then, immediately we started bolus hypertonic normal saline (3% NaCl) and Inj. Fosphenytoin. At this point, our suspicion was hyponatremia due to adrenal Insufficiency, so we advised basal cortisol and serum ACTH which revealed low basal cortisol 2.9 mcg/dl (normal 3.7-19.4 mcg/dl) and ACTH-
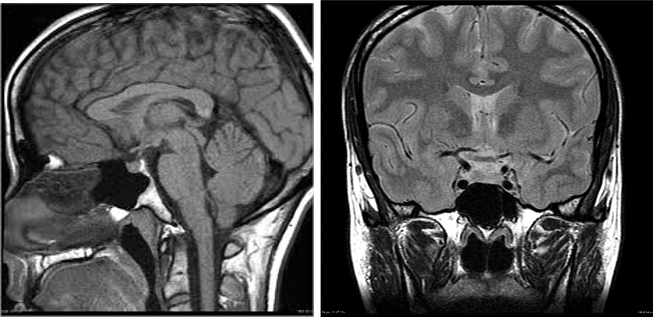
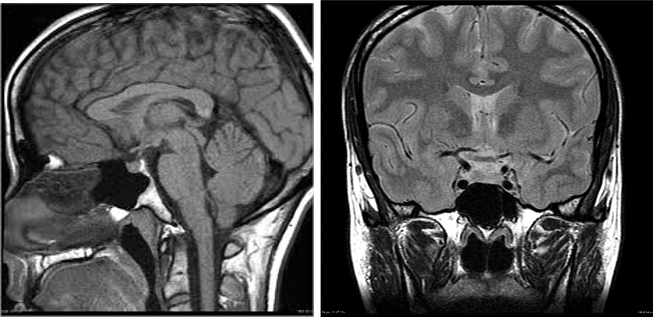
Figure 1 and 2: MRI of brain sagittal and coronal section respectively, T1 weighted image, showing normal pituitary and normal sella trucica. There is no evidence of hemorrhage, intracranial mass, or aneurysm.
As the patient had severe PPH, hypotension, agalactia, low normal blood sugar & glucocorticoid responsive hyponatremia, she was diagnosed as a case of a case of panhypopituitarism 2° to acute Sheehan’s Syndrome following severe post-partum hemorrhage (PPH). She started recovering & regained her sensorium, so we switched to daily physiological oral dose of dexamethasone. On 9th day of her admission, she was discharged with normal blood pressure and normal blood sugar. Dexamethasone was planned to be continued lifelong. 2 weeks later, on further follow up, she remained conscious, oriented with normal blood pressure. Random blood sugar was 6.8 mmol/L. S. electrolyte was normal with sodium 138 mmol/L, K 3.9 mmol/L.A thyroid profile workup was kept in plan on her next visits (1 month later and so on) to see the further development of hypothyroidism.
Discussion
Sheehan’s syndrome or adenohypophyseal ischemic necrosis occurs following hypoperfusion as a result of ischemic pituitary necrosis due to severe postpartum hemorrhage [7-10]. Through improved management of hemodynamic complications, its incidence has gradually declined over time. Although the exact incidence is unknown and it rarely occurs in modern obstetric practices, Sheehan’s syndrome still must be considered in cases of PPH. Only a small proportion of patients with Sheehan’s syndrome may have a sudden onset of severe hypopituitarism immediately after delivery, whereas most patients have mild illness and they have not been diagnosed for a long time so that they are not treated appropriately [11]. Gei-Guardia et al. reported the average time between the previous obstetric event and diagnosis of Sheehan’s syndrome was 13 years in a study of 60 patients [12]. Early diagnosis and treatment are crucial for the patients with Sheehan’s syndrome especially for the patients with severe postpartum hemorrhage. Symptoms that first occur within 6 weeks postpartum are defined as acute Sheehan’s syndrome as in this report.
The diagnosis can be made reliably in the presence of lactational failure, prolonged amenorrhea and hypoglycaemic crises [13]. However, other signs of adenohypophysal insufficiency are often delayed and subtle leading to the diagnosis being missed. In some cases the pituitary necrosis is only partial and the syndrome can present in atypical and incomplete forms further complicating the diagnostic procedure [14]. Hypopituitarism has several possible etiologies. Apart from adenohypophysal necrosis, other causes are quoted: tumoral, immunological, iatrogenic, traumatic,infectious and genetic [15]. The MRI scan is the investigation of choice, but there is little data illustrating postpartum hypophyseal necrosis in the acute phase. In case of hypophyseal necrosis, the early MRI highlights a pituitary gland of reduced size with segments of hypersignal in T1 and T2 and hyposignal without contrast. Later, the MRI shows an empty sella turcica following pituitary atrophy. Endocrine investigations during the acute phase of hypophyseal necroses are less well documented [16]. Corticotropin insufficiency could suggest the concept of low plasmatic cortisol, just as urinary free cortisol and ACTH would be low. Thyroid hormone levels are low.
The basic blood level of growth hormone would be low [17]. Prolactin levels are important because they are physiologically very high at the end of pregnancy and return to normal approximately 6 weeks postpartum in women who do not breastfeed. An early drop in prolactin levels would therefore suggest adenohypophyseal insufficiency. Once the diagnosis is established, treatment aims to correct life threatening endocrine imbalance: hypoglycaemia and adrenal insufficiency being the most urgent, meriting treatment even in anticipation of laboratory confirmation. Complete hormonal substitution aims to restore normal function in the thyroid, adrenal and ovarian axes. Subsequent pregnancies are achieved using ovarian stimulation techniques [18].
Our case presented with headache, vomiting life-threatening seizure and altered sensorium as the first symptoms. Our literature review revealed that such marked and abrupt onset in Sheehan’s syndrome are rare. The primary causes of postpartum seizures include eclampsia, cerebral ischemic changes, cerebral hemorrhage, cerebral venous sinus thrombosis, reversible cerebral vasoconstriction syndrome, epilepsy, and hypoglycemia [19]. None of the imaging results in our case revealed any brain disorders, and because the laboratory investigations revealed hyponatremia and following low hormonal levels, we reasonably concluded that our final diagnosis was acute Sheehan’s syndrome with the loss of general pituitary function.
Only a few studies have discussed acute Sheehan’s syndrome, and we found no literature review on this topic. Therefore, we performed a PubMed/Medline and Google Scholar search of the English literature between January 1990 and May 2014, using the key words “acute” or “early” and “Sheehan syndrome” or “Sheehan’s syndrome.” Searching with the keywords mentioned above, 52 articles were identified. We read these articles and selected those cases with patients whose symptoms first occurred within 6 weeks postpartum; this identified 19 suitable reports (21 cases including our case). Nineteen full texts of articles were read by the authors. Twenty cases of acute Sheehan’s syndrome were published in international peer-reviewed literature. Of the identified cases, 17 described the amount of postpartum bleeding. Most patients suffered a massive hemorrhage; however, in one case, a PPH of approximately 500 mL caused acute Sheehan’s syndrome [20]. These results suggested that most cases of acute Sheehan’s syndrome occurred after PPH, which is well known for traditional Sheehan’s syndrome. The Hb levels were mentioned in 12 cases, all of which experienced a moderate to severe decrease in Hb (approximately 3.0–8.8 g/dL).
These results suggested that anemia is a reason for acute Sheehan’s syndrome. However, some cases were not associated with either PPH or anemia. It is difficult to discuss the relationship between hypotension and acute Sheehan’s syndrome because the definition of shock was unclear in the previous reports. However, 12 of the 21 cases had experienced hypotension below 90 mmHg, which suggested that hypotension is a risk factor for acute Sheehan’s syndrome. Dejager et al. reported an interesting case showing severe hypotension because of an epidural anesthesia causing acute Sheehan’s syndrome; this study revealed that only hypotension may be the cause of acute Sheehan’s syndrome [21]. PPH, anemia, and hypotension may decrease the blood flow to the pituitary and lead to necrosis of the gland. To prevent acute Sheehan’s syndrome, the obstetrician should strive to prevent anemia and hypotension in the treatment of PPH.
The first signs were reported within 3 days, 4–10 days, and 11–20 days postpartum in 6, 10, and 5 cases, respectively. Sixteen of 21 patients experienced the first signs within 10 days postpartum. Therefore, the obstetrician should be particularly vigilant for this condition during this time period. The first signs were hyponatremia because of adrenal insufficiency in 12 cases, diabetes insipidus in 4, and hypothyroidism in 2, and panhypopituitarism in 3. Notably, the length of time after delivery until the first sign was noted varied depending on the cause. Adrenal insufficiency presented at a median of 7.9 days (14 h–19 days), diabetes insipidus at 4 days (1–7 days), hypothyroidism at 18 days (16–20 days), and panhypopituitarism at 9 days (4–17 days). Although the reasons for postpartum headache vary and may be difficult to diagnose accurately, acute Sheehan’s syndrome is one possible cause. In our literature review, 6 of 21 patients reported severe headache on the day of delivery. There was no correlation between the presence of headache and the onset of signs indicating acute Sheehan’s syndrome. The presence of severe headache on the day of delivery may indicate intracranial hemorrhage, but if that can be ruled out, the obstetrician should remain alert for the possible onset of acute Sheehan’s syndrome.
MRI evidence of acute Sheehan’s syndrome was reported in 13 cases. Early radiologic findings within postpartum day 20 were reported in 11 cases. In our case, the MRI findings were normal on postpartum day 15 (7 days after the seizure). Two studies reported that the MRI scans were normal on postpartum day 6; in addition, another study reported that normal scans were obtained on day 19 [22-24]. Bunch et al., Kaplun et al. and Sasaki et al. reported an enlarged pituitary gland with an abnormal signal on the T1-weighted pre-contrast images on postpartum day 10, day 10 and day 6, respectively [9 25,26]. Anfuso et al. described MRI findings from postpartum day 8 that showed an abnormal lack of pituitary gland enhancement [20]. Although the data was limited, in four of eleven cases, there were insignificant findings because of acute Sheehan’s syndrome on the MRI within postpartum 20 days. A large intrasellar mass with superior extension, an enlarged pituitary gland with an abnormal signal and an abnormal lack of pituitary gland enhancement were reported as early radiologic findings of acute Sheehan’s syndrome.
Pregnancy after acute Sheehan’s syndrome has not been reported. Whether the patient needs an induction of ovulation or not depends on the severity of this condition. If the patient did not have menstrual cycles because of hypopituitarism, the patient may need an induction of ovulation to establish a pregnancy. Our patient had no menstrual cycles; therefore, the patient received hMG-hCG treatment and established a pregnancy. A study of a large number of pregnancies in hypopituitarism has not been reported. The largest number of cases was reported by Kübler et al. who reviewed pregnancy management in women with hypopituitarism [27]. Based on the analysis of 31 pregnancies in 27 women, they concluded that women with hypopituitarism were at an increased risk of obstetrical complications; postpartum hemorrhage occurred in 8.7%, transverse lie occurred in 16, and 42.4% of the newborns who were small for gestational age. Fortunately, our patient had no obstetrical complications other than the postdate delivery.
The postdate delivery was probably not because of the loss of general pituitary function because a review reported no increase in the rate of postdate deliveries in women with hypopituitarism [27]. In addition, animal data has shown that the delivery proceeded normally in oxytocin-deficient mice [28]. However, because there have been few reported cases of pregnancy with generalized hypopituitarism, many such cases will be need to be studied to obtain more human data.
Conclusion
Postpartum pituitary necrosis is a known complication but is now rarely seen. Even if postpartum hemorrhage has been well managed, this complication cannot be excluded. It is necessary to consider this diagnosis in all patients having presented with cardiovascular collapse during childbirth, whatever the cause and in the presence of classical signs of pituitary insufficiency. If not diagnosed early, it could cause increased morbidity and mortality.
References
- Sheehan HI. (1937). Postpartum necrosis of the anterior pituitary. Journal of Pathology and Bacteriology. 45:189-214.
- Sheehan HI. (1965). The frequency of postpartum hypopituitarism. Journal of Obstetrics& Gynaecology of British Common Wealth. 72:103-14.
- B. A. Laway, S. A. Mir, M. I. Bashir, J. R. Bhat, J. Samoon, and A. H. Zargar, (2011). “Prevalence of hematological abnormalities in patients with Sheehan's syndrome: response to replacement of glucocorticoids and thyroxine,” Pituitary, vol. 14, no. 1, pp. 39–43.
- D. Gokalp, A. Tuzcu, M. Bahceci et al., (2011). “Analysis of thrombophilic genetic mutations in patients with Sheehan's syndrome: is thrombophilia responsible for the pathogenesis of Sheehan's syndrome?” Pituitary, vol. 14, no. 2, pp. 168–173.
- M. Sert, T. Tetiker, S. Kirim, and M. Kocak, (2003). “Clinical report of 28 patients with Sheehan's syndrome,” Endocrine Journal, vol. 50, no. 3, pp. 297–301.
- C. Shivaprasad, (2011). “Sheehan's syndrome: newer advances,” Indian Journal of Endocrinology and Metabolism, vol. 15, supplement 3, pp. S203–S207.
- Y. S. Lee and S. S. Moon, “A case of sheehan's syndrome that manifested as bilateral ptosis,” Journal of Korean Medical Science, vol. 26, no. 4, pp. 580–582.
- H. Tessnow and J. D. Wilson, (2011). “The changing face of Sheehan's syndrome,” American Journal of the Medical Sciences, vol. 340, no. 5, pp. 402–406, 2010.
- J. Kaplun, C. Fratila, A. Ferenczi et al., (2008). “Sequential pituitary MR imaging in Sheehan syndrome: report of 2 cases,” American Journal of Neuroradiology, vol. 29, no. 5, pp. 941–943.
- Pasa, A. Altintas, C. Tumer et al., (2010). “Prothrombin time, activated thromboplastin time, fibrinogen and D-Dimer levels and von-willebrand activity of patients with Sheehan's syndrome and the effect of hormone replacement therapy on these factors,” Uluslararasi Hematoloji-Onkoloji Dergisi, vol. 20, no. 4, pp. 212–219.
- F. Kele?timur, (2003). “Sheehan's syndrome,” Pituitary, vol. 6, no. 4, pp. 181–188.
- O. Gei-Guardia, E. Soto-Herrera, A. Gei-Brealey, and C. K. Chih Hao, (2011). “Sheehan syndrome in Costa Rica: clinical experience with 60 cases,” Endocrine Practice, vol. 17, no. 3, pp. 337–344.
- Assan R. (1984). Urgences métaboliques et endocriniennes. In: Kleinknecht D, editor. Principes de réanimation médicales. 3e éd. Paris: Flammarion médecine sciences. pp. 292–326.
- Merger R, Levy J, Melchior J. 4e édition. Paris: Masson; (1974). Précis d'obstétrique; pp. 321–31.
- Perraudin V, Lefebvre H, Kuhn JM. (1992). Insuffisance antéhypophysaire. Encycl Méd chi (Paris), Endocrinologie-Nutrition 10-019-A-10. 1–12.
- Molitch ME. (1998). Pituitary diseases in pregnancy. Semin Perinatol. 22:457–70.
- Jialal I, Naidoo C, Norman RJ, Rajput MC, Omar MA, Joubert SM. (1984). Pituitary function in sheehan's syndrome. Obstet Gynecol. 63:15–9.
- Olivennes F, Harmas A, Frydman R. (1998). L'induction de l'ovulation: strategies thérapeutiques Réalités en Gynécologie. Obstétrique. 28:19–21.
- Edlow JA, Caplan LR, O'Brien K, Tibbles CD. (2013). Diagnosis of acute neurological emergencies in pregnant and post-partum women. Lancet Neurol. 12:175–185.
- Anfuso S, Patrelli TS, Soncini E, Chiodera P, Fadda GM, Nardelli GB. (2009). A case report of Sheehan’s syndrome with acute onset, hyponatremia and severe anemia. Acta Biomed. 80:73–76.
- Dejager S, Gerber S, Foubert L, Turpin G. (1998). Sheehan’s syndrome: differential diagnosis in the acute phase. J Intern Med. 244:261–266
- Munz W, Seufert R, Knapstein PG, Pollow K. (2004). Early postpartum hyponatremia in a patient with transient Sheehan’s syndrome. Exp Clin Endocrinol Diabetes. 112:278–280. doi: 10.1055/s-2004-817976.
- Wang SY, Hsu SR, Su SL, Tu ST. (2005). Sheehan's syndrome presenting with early postpartum congestive heart failure. J Chin Med Assoc. 68:386–391.
- Kumar S, Burrows D, Dang S, Simmons D. (2011). Sheehan syndrome presenting as central diabetes insipidus: a rare presentation of an uncommon disorder. Endocr Pract. 17:108–114.
- Bunch TJ, Dunn WF, Basu A, Gosman RI. (2002). Hyponatremia and hypoglycemia in acute Sheehan’s syndrome. Gynecol Endocrinol. 16:419–423.
- Sasaki S, Fujisawa I, Ishihara T, Tahara Y, Kazuma M, Fujiwara Y, et al. (2014). A novel hook-shaped enhancement on contrast-enhanced sagittal magnetic resonance image in acute Sheehan’s syndrome: a case report. Endocr J. 61:71–76.
- Kubler K, Klingmuller D, Gembruch U, Merz WM. (2009). High-risk pregnancy management in women with hypopituitarism. J Perinatol. 29:89–95.
- Nishimori K, Young LJ, Guo Q, Wang Z, Insel TR, Matzuk MM. (1996). Oxytocin is required for nursing but is not essential for parturition or reproductive behavior. Proc Natl Acad Sci U S A. 93:11699–11704.
Citation: Richmond Ronald Gomes and Moin Shahid. (2020). A Rare Case of Acute Sheehan’s Syndrome in a Young Lady with Severe Acute Symptomatic Hyponatremia following PPH. Archives of Endocrinology and Diabetes 2(1).
Copyright: © 2020 Richmond Ronald Gomes. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
