Case Report
Volume 2 Issue 5 - 2020
A Case of Leiomyosarcoma of the Urinary Bladder in a 35-Year-Old Male
1Department of Surgery, Mater Dei Hospital, Msida MSD 2090, Malta
2Department of Urology, Mater Dei Hospital, Msida MSD 2090, Malta
2Department of Urology, Mater Dei Hospital, Msida MSD 2090, Malta
*Corresponding Author: Isaac Balzan, Department of Surgery, Mater Dei Hospital, Msida MSD 2090, Malta.
Received: November 26, 2020; Published: December 14, 2020
Abstract
Leiomyosarcoma of the bladder is a rare malignancy, generally affecting elderly males. It has significant associated morbidity and mortality and there is a lack of literature regarding this aggressive tumour. This article reports the case of a bladder leiomyosarcoma in a 35-year-old Caucasian male who was successfully treated. Management involves a combination of chemotherapy, radiotherapy and surgical resection. Radical cystectomy with wide resection margins is considered as the gold-standard but has several implications on patient quality of life. More conservative surgical approaches are arising with similar outcomes and improved quality of life. The aim of this article is to highlight the important features of bladder leiomyosarcoma and its possible incidence in younger patients. This article also aims to accentuate the several treatment options and the current gold-standards in care.
Keywords: Leiomyosarcoma; Bladder
Abbreviations: CT IVU: Computed tomography intravenous urogram; TURBT: Trans-urethral resection of bladder tumour; STUMP: Smooth muscle tumour of uncertain malignant potential
Introduction
Leiomyosarcoma of the urinary bladder is a rare malignancy, generally affecting elderly males. It has significant associated morbidity and mortality and there is a lack of literature regarding this aggressive tumour. This article reports the case of a bladder leiomyosarcoma in a 35-year-old Caucasian male who was treated with robot assisted partial cystectomy. At the time of writing this article, the patient had no signs of recurrence and was experiencing a good quality of life.
Report
35 year-old, previously healthy gentleman who presented to the accident and emergency department complaining of a two day history of urinary frequency, dysuria and occasional gross haematuria, associated lower abdominal and suprapubic pain. A urine sample submitted for microscopy and culture cultivated no bacteria. At accident and emergency he was hypertensive and physical examination revealed suprapubic tenderness but was otherwise unremarkable.
Contrast enhanced CT imaging performed on showed a left sided, lobulated mass within the urinary bladder, measuring 51x60mm in size. No enlarged lymph nodes, free fluid or upper urinary tract lesions were seen. The mass appeared to be arising from within the wall rather than the urothelium and seemed to be in contact with the sigmoid colon, with no fat plane between the two structures.
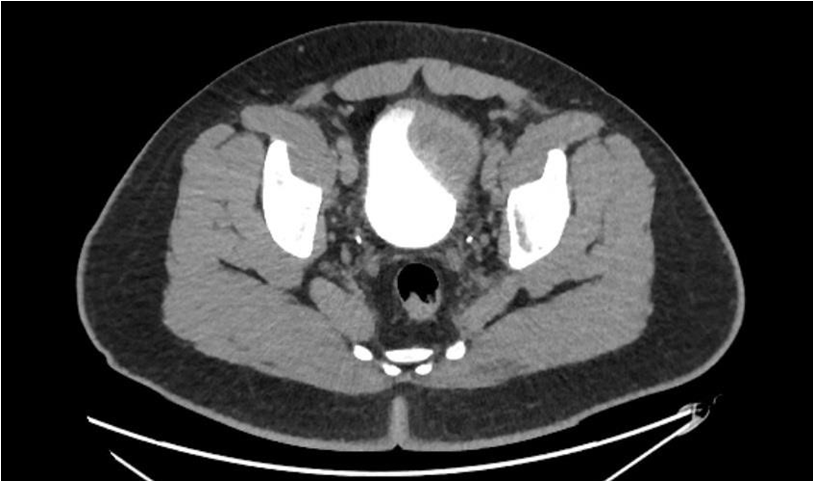
Figure 1: Section from a CT IVU performed on this patient showing a large mass measuring 5.1 x 6.0 cm in the left anterolateral wall of the urinary bladder.
The patient underwent a rigid cystoscopy which confirmed a soft extrinsic mass and loop resection biopsy was performed. Initial histology from said biopsy was inconclusive due to abundant necrotic tissue. A colonoscopy was performed up to the caecum and was unremarkable. An ultrasound contrast study concluded that there was a likely mesenchymal tumour in the submucosa of the urinary bladder wall but it had no definite features of haemangioma.
An MRI of the pelvis was performed to better characterise the lesion and it concluded that the left-sided urinary bladder wall tumour was seen to involve the whole thickness of the bladder wall and projected into the bladder lumen but did not extend into the extra vesical tissues. There were no pathological pelvic bone lesions or pelvic sidewall lymphadenopathy. A PET scan was performed to rule out any metastasis and found no evidence of abnormal tracer accumulation concluding no evidence of extra-vescical pathology.
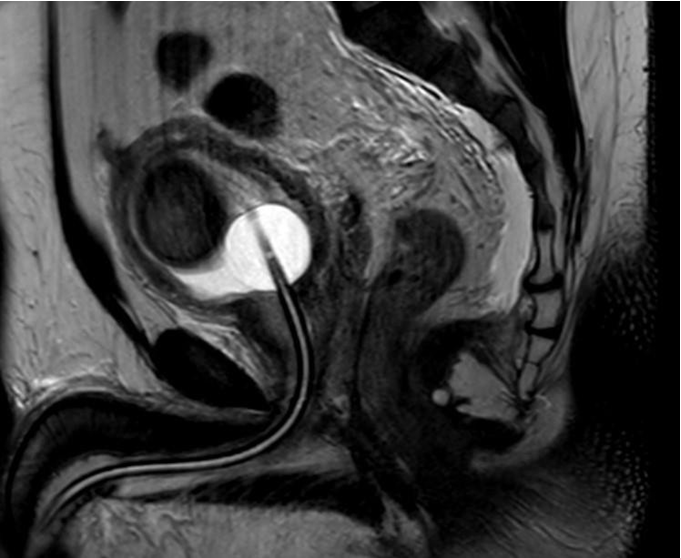
Figure 2: T2 Weighted MR scan showing the described bladder wall lesion and catheter inserted in the urinary bladder.
The patient underwent an uncomplicated trans-urethral resection of bladder tumour (TURBT) where larger resection biopsies were taken. Histology showed thickened fascicles of detrusor muscle, with large areas of coagulative, ischaemic-type necrosis and no evidence of atypia in the viable muscle tissue, suggestive of Leiomyoma with profuse ischaemic necrosis. Due to the nature of the specimen, a leiomyosarcoma could not be excluded with certainty and excision of the lesion was recommended.
The patient was referred to a specialist robotic centre where he underwent a Robot assisted laparoscopic partial cystectomy and pelvic lymph node dissection. Sections from the bladder showed an ulcerated, well- circumscribed, smooth muscle lesion with diffuse necrosis and calcifications that seemed to be of ischaemic type. The lesional cells had abundant eosinophilic cytoplasm and blunt looking nuclei, however scattered, larger, more plump nuclei were noted as well. The lesion appeared to arise at the level of the muscularis propria. No mitotic activity was seen within the tumour. There was congestion and mild chronic inflammation in the lamina propria, but the overlying epithelium was unremarkable with no evidence of CIS or urothelial carcinoma. Inked margins were clear and resection margins showed no tumour. All the resected lymph nodes showed no evidence of metastatic malignancy.
Based on these findings, a preliminary diagnosis of smooth muscle tumour with clear margins was made. The case was sent for expert second opinion and findings were in keeping with the above, supporting the diagnosis of a benign smooth muscle lesion (leiomyoma). However, in view of the extensive necrosis, this may not have been representative of the entire lesion. Therefore, it was suggested to manage this lesion as a smooth muscle tumour of uncertain malignant potential (STUMP).
The patient was followed up closely at surgical outpatients and was doing well. He underwent repeat MRI, CT and rigid cystoscopy and a small, asymptomatic pelvic lymphocoele was noted and managed conservatively. Bladder volume was measure at 500cc and the patient described a good quality of life. Further follow up is planned at the time of writing.
Discussion
Leiomyosarcomas are the commonest form of malignant mesenchymal tumours [1] with an incidence of around 15% of all newly diagnosed sarcomas. Leiomyosarcoma is also the most frequently occurring sarcoma of the urinary bladder but makes up less than 1% of bladder malignancies [2]. The incidence of leiomyosarcomas increases with age and they occur mostly between 70 and 80 years [3]. Male to female ratio varies; generally, there seems to be a slight male predominance [4] with some studies showing ratios of 2:1[1]. An increased incidence has also been shown in women of reproductive age and in patients undergoing pelvic irradiation or systemic chemotherapy [5].
Bladder leiomyosarcoma usually arises in the vertex of the bladder (50%) and in the lateral wall (25%). It is scarcely found in the trigone [6]. The most prevalent symptoms at presentation are haematuria, frequency and dysuria [7].
Leiomyosarcomas typically present and firm greyish nodules [5] and exhibit intersecting, sharply marginated fascicles of spindle cells with abundant eosinophilic cytoplasm and elongated, hyperchromatic nuclei with varying degrees of coagulative necrosis. They can be classified as high or low grade and there is no concrete evidence that the benign leiomyoma can undergo malignant change to become leiomyosarcoma [8].
Overall prognosis is poor as they are highly aggressive tumours and few, less than 15%, are picked up early on [9]. Treatment depends on the staging at presentation but includes chemotherapy, radiotherapy and resection surgery. The gold standard for treatment is surgical resection, aiming for a clear resection margin, this being the best prognostic indicator. Chemoradiotherapy can be used to compliment surgery particularly in advanced cases or those with metastasis [9, 10]. Various surgical techniques can be applied; radical cystectomy (including excision of the seminal vesicles and prostate in men and cervix and vaginal cuff in women) with wide margins is generally considered as the gold-standard and results in adequate negative margin rates and low recurrence rates. However, this procedure has a significant negative impact on patient quality of life [4].
Another option available for some candidates, such as those not fit for major surgery, inoperable tumours or small submucosal tumours, is transurethral resection of bladder tumour (TURBT) which can be combined with adjuvant chemoradiotherapy or photocoagulation. The long-term outcome for this option is inferior to resection [11]. Partial resection, i.e. partial cystectomy has emerged as an alternative option. It was previously considered inferior to radical cystectomy in terms of outcome but, with ever progressing and improving surgical techniques, it is now believed to offer similar results and may be a preferable option particularly because it spares some functionality [12]. A study by Knoedler et al. showed similar results in terms of outcome when comparing partial cystectomy with radical cystectomy, with no difference between the two in 10-year distant recurrence free survival and cancer survival in general [12]. This has been further accentuated by the advent of robotic surgery but, because of its relatively recent introduction, there is a lack of data regarding long-term outcomes.
In a series by Golombos et al. [13] on robot-assisted partial cystectomy, they showed a decreased length of stay, with the median duration being 1 day and lower morbidity and complication rates with only 6.9% of patients developing in-patient complications. Through this technique they were also able to remove an average of 12 nodes at pelvic lymph node dissection; more than the adequate threshold of 10 which is commonly cited in radical cystectomy literature [14].
Conclusion
Bladder leiomyosarcomas are an aggressive form of tumours with significant impact on the morbidity and mortality of affected patients. The current gold-standard treatment options which involve surgical resection also carry significant implications to the patient’s survival and quality of life. However, ongoing advances in surgical practice are providing alternative options and early studies suggest similar survival results and better quality of life. Due to the recent introduction of robotic surgery, there is a lack of data regarding long-term outcomes and further research is required in the future to be able to properly compare and draw accurate conclusion regarding the best treatment for this disease.
Conflict of Interest
There are no conflict of interest to be declared for this article.
There are no conflict of interest to be declared for this article.
Acknowledgement
With special thanks to my co-authors and supervisor for their guidance and contributions to this article.
With special thanks to my co-authors and supervisor for their guidance and contributions to this article.
References
- Lee TK, Miyamoto H, Osunkoya AO, Guo CC, Weiss SW, Epstein JI. (2010). Smooth muscle neoplasms of the urinary bladder: a clinicopathologic study of 51 cases. Am J Surg Pathol. Apr; 34 (4):502–9.
- George S, Serrano C, Hensley ML, Ray-Coquard I. (2018). Soft Tissue and Uterine Leiomyosarcoma. J Clin Oncol Off J Am Soc Clin Oncol. 10; 36 (2):144–50.
- Miettinen MM, editor. (2016). Modern soft tissue pathology: tumors and non-neoplastic conditions. Second edition. Cambridge, United Kingdom: Cambridge University Press; 1062 p.
- Martin SA, Sears DL, Sebo TJ, Lohse CM, Cheville JC. (2002). Smooth muscle neoplasms of the urinary bladder: a clinicopathologic comparison of leiomyoma and leiomyosarcoma. Am J Surg Pathol. Mar;26 (3):292–300.
- Xu Y-F, Wang G-C, Zheng J-H, Peng B. (2011). Partial cystectomy: Is it a reliable option for the treatment of bladder leiomyosarcoma? Can Urol Assoc J J Assoc Urol Can. Feb; 5 (1):E11-13.
- Dahm P, Gschwend JE. (2003). Malignant non-urothelial neoplasms of the urinary bladder: a review. Eur Urol. Dec; 44 (6):672–81.
- Rosser CJ, Slaton JW, Izawa JI, Levy LB, Dinney CPN. (2003). Clinical presentation and outcome of high-grade urinary bladder leiomyosarcoma in adults. Urology. Jun; 61 (6):1151–5.
- Goldblum JR, Folpe AL, Weiss SW. (2019). Enzinger & weiss’s soft tissue tumors. 7th ed. Philadelphia: Elsevier. ISBN: 978-0-323-61096-4.
- Labanaris AP, Zugor V, Meyer B, Nützel R, Helmus S, Labanaris PG, et al. (2008). Urinary bladder leiomyosarcoma in adults. Int Urol Nephrol. 40(2):311–6.
- Spiess PE, Kassouf W, Steinberg JR, Tuziak T, Hernandez M, Tibbs RF, et al. (2007). Review of the M.D. Anderson experience in the treatment of bladder sarcoma. Urol Oncol. Feb; 25(1):38–45.
- De Berardinis E, Giulianelli R, Zarrelli G, De Santis C, Ginepri A, Gentile BC, et al. (1997). Leiomyosarcoma of urinary bladder: personal experience in 3 cases over a 10-year period. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol. Feb; 69 Suppl 1:73–80.
- Knoedler JJ, Boorjian SA, Kim SP, Weight CJ, Thapa P, Tarrell RF, et al. (2012). Does partial cystectomy compromise oncologic outcomes for patients with bladder cancer compared to radical cystectomy? A matched case-control analysis. J Urol. Oct; 188 (4):1115–9.
- Golombos DM, O’Malley P, Lewicki P, Stone BV, Scherr DS. (2017). Robot-assisted partial cystectomy: perioperative outcomes and early oncological efficacy. BJU Int. Jan; 119 (1):128–34.
- Bochner BH, Herr HW, Reuter VE. (2001). Impact of separate versus en bloc pelvic lymph node dissection on the number of lymph nodes retrieved in cystectomy specimens. J Urol. Dec; 166 (6):2295–6.
Citation: Isaac Balzan, Gerald Busuttil, John Sciberras and Keith Pace. (2020). A Case of Leiomyosarcoma of the Urinary Bladder in a 35- Year-Old Male. Journal of Medical Research and Case Reports 2(5).
DOI: 10.5281/zenodo.4325587
DOI: 10.5281/zenodo.4325587
Copyright: © 2020 Isaac Balzan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
