Research Article
Volume 6 Issue 1 - 2024
Evaluation the Appropriateness of Geriatrics’ Medications by Using STOPP/START and Beer’s Criteria in Tertiary Care Center in Saudi Arabia
1Hend H Metwali, Pharm D, Internal Medicine Clinical Pharmacist, Pharmaceutical Care Department at King Abdulaziz Medical City, Saudi Arabia- Jeddah
2Ahmed Y Mayet, professor/ Consultant Clinical Pharmacist/ Internal Medicine, King Saud University Medical City, Saudi Arabia- Riyadh
3Dr Khalid Alayed, Assistant professor, department of medicine, College of Medicine, King Saud University, Saudi Arabia-Riyadh
2Ahmed Y Mayet, professor/ Consultant Clinical Pharmacist/ Internal Medicine, King Saud University Medical City, Saudi Arabia- Riyadh
3Dr Khalid Alayed, Assistant professor, department of medicine, College of Medicine, King Saud University, Saudi Arabia-Riyadh
*Corresponding Author: Metwali H, Pharm D, Internal Medicine Clinical Pharmacist, Pharmaceutical Care Department at King Abdullah International Medical Research Center / King Saud bin Abdulaziz University for Health Sciences, King Abdulaziz Medical City –Jeddah Saudi Arabia.
Published: November 30, 2024
Background: Inappropriate prescribing of medications in the geriatric population causes serious consequences. It increases mortality, mortality, and cost. In addition, it results in polypharmacy, severe adverse drug reactions, drug-drug interactions, and poor adherence. Our study outcome is to identify and assess the prevalence of potentially inappropriate medications (PIMs), potentially omitted medications (POMs) and polypharmacy during hospital admission using the screening tools of older people’s prescriptions (STOPP) / screening tool to alert to right treatment (START) and The American Geriatrics Society (AGS) Beers Criteria (AGS Beers Criteria)
Methods: We conducted a prospective cohort study in patients aged ≥65 years who were admitted under internal medicine services from April until October 2021. The STOPP/START and AGS Beer's criteria were applied to the patient's clinical profile and concurrent medications list, and PIMs and POMs were recorded. Data were analyzed using SPSS 26.0 version statistical software. Descriptive statistics described the quantitative and categorical variables. Pearson's Chi-square test observed the association between categorical study variables and outcome variables.
Results: A total of 339 patients were evaluated, 60.9% were females, and 60% were > 75 years of age. The main reasons for the hospitalization were urinary tract infection 26%, acute kidney injury 20.8%, pneumonia 15%, and stroke 12.5%. We recorded 291 PIMs by STOPP, 168 PIMs by AGS Beer's, and 406 POMs by START criteria. The bivariate analysis shows no statistically significant association between age groups, gender, number of reasons for admission, and PIMs. Out of the 3 study variables, only gender was statistically significantly associated with categories of POM, in which a higher proportion (14.8%) female subjects required >4 POM when compared with 5.1% male subjects, whereas 53.2% male subjects required 3 to 4 POM when compared with 46.1% of female subjects (p=0.010). The prevalence of polypharmacy was 82.2%. Among all recorded PIMs, proton pump inhibitors were the most common drug and were used in 26.8% of patients, followed by anti-platelets 4.5%, antipsychotics 4%. While the most common POMs were recorded with vitamin-D and calcium supplements (25.6%) in bed-bound and osteoporotic patients, followed by angiotensin-converting enzyme inhibitors in heart failure and coronary arteries diseases (21%); and Acetylcholinesterase inhibitor in dementia (13.8%).
Conclusion: PIMs, POMs, and polypharmacy were prevalent among our geriatric population. It requires further assessment to see the impact of our health care outcomes. Standard criteria like STOPP/START or AGS Beer's should be implemented before prescribing medications in geriatrics to improve prescribing practice in these settings.
Keywords: STOPP/START; AGS Beer’s; Geriatrics; Potentially inappropriate medications; Potentially omitted medications
Background
Geriatrics experience multiple comorbidities that requires multiple medications which may cause serious adverse drug reaction (ADRs), drug-drug interactions and adherence issues. Also, geriatrics are not always adhere to medications prescribed to them. Optimization of drug therapy is an important part in prescribing a medication for this population. Potential inappropriate medication (PIM) prescribed to geriatrics is a worldwide medical problem; increases the incidence of ADRs are the serious consequences. Geriatric population are very sensitive to some medications which may increase the risk of serious ADRs like falls, hypotension, hypoglycemia or cognitive impairment, all lead to significant increase in morbidity, mortality and overall medical costs. Most of pre-marketing drug studies are not include geriatric patients; the approved doses may not be appropriate for this group of patients that makes prescribing medications for them more challenging due to their altered pharmacokinetics and pharmacodynamics condition. Also in geriatrics, due to their low muscle mass, serum creatinine levels may not be adequate to reflect exact renal function and drug dosing can be challenging and potential dangerous. There are many different ways for recognizing PIM; it can be based on clinical judgment, specific criteria that build by experts’ agreement, or created lists of medications that should not be used.
STOPP/START criteria both were firstly published in 2008 (1) then had been updated in 2014 (2). It is commonly used in Europe to identify PIMs and POMs. STOPP/START criteria have been established and demonstrated in patients aged 65 or more in purpose of focusing on PIMs and potential prescribing omissions (PPOs). The main objective of the STOPP criteria is to diminish medication related ADRs by avoiding PIMs occurrence. The aim of the START criteria is to reduce the incidence of therapeutic failures by focusing on PPOs and promoting appropriate medication prescribing if no contraindication is available. Nineteen European geriatric pharmacotherapy experts from 13 different countries were contribute in reviewing and updating the new STOPP/START criteria, 114 criteria were included after two Delphi validation rounds, 80 criteria under STOPP list and 34 criteria under START list (2). Both criteria are used for evaluating the appropriateness of prescribed medications in geriatrics patients. Many published studies assured the effectiveness of STOPP/START criteria in reducing PIM, polypharmacy and serious ADEs, causing fewer falls, and lowering medication costs. While the AGS Beers Criteria are commonly used by clinicians and healthcare administrators in United States to identify PIMs. This criteria established firstly in 2011, and get updates each three years. It is a list of PIMs that are recommended to be avoided in elderly people in most circumstances or under specific situations, such as in certain diseases or conditions.
A systemic review and meta-analysis published in 2019 by Bader Alqahtani, et al, they studied the prevalence and risk factors of falls in patients aged more than or equal 65 who were living in the Gulf Cooperation Council countries. The study highlights that, the prevalence of falls in geriatrics in those countries are 45%. The risk factors that associated with falls were age, female sex, low educational level and number of medications. (3) GerontoNET ADR risk score has been used for hospitalized geriatric patients to facilitate recognizing those at high risk of ADRs occurrence. A study published in September, 2016 by Amy Copperthwait, et al, assessed the relations between high GerontoNET ADR risk score and incidence of ADRs. The study concluded that the number of comorbidities and prescribed medications are significant contributors to an increased risk score. The study concluded that GerontoNet score is useful for clinicians who not trained in geriatric medicine to identify ADRs risk in their patients. (4) There are limited number of clinicians who trained in geriatric medicine, especially in Gulf countries and few geriatricians are practicing in hospital setting.
There are two different prospective studies by Gallagher P, et al and Hamilton H, et al comparing between AGS Beers criteria and STOPP criteria in identifying PIM and related ADEs in hospitalized geriatric patients. They found both criteria were overlapped in multiple areas. Both criteria were focus on the higher risk of ADEs in geriatrics with the use of long acting benzodiazepines, tricyclic antidepressants, anticholinergic drugs, and non–cyclooxygenase 2–selective nonsteroidal anti-inflammatory drugs. STOPP criteria consider medication duplication in one class unlike AGS Beers. Both studies concluded that STOPP recognize a significantly higher percentage of geriatrics who requiring hospital admission because of ADEs than did the AGS Beers criteria (5,6) Another single blind cluster randomized trial done in tertiary hospital in Ireland in 2016 including 700 patients. The study primary outcome is to determine if the use of STOPP/ START criteria will decrease the ADRs during hospital admission and the secondary outcomes were median length of stay (LOS) and 28-day total medication cost. It found that 21% ADRs occurred in control arm while 12% in intervention arm (the ARR = 9.3%, with NNT= 11). This study concluded that STOPP/ SRART criteria is markedly decrease the incidence of ADRs during hospital admission. The median LOS in the hospital was equal eight days in two arms. While the median cost of patient medication was markedly lower in the intervention arm than in the control one. (7)
The research idea promotes improvement the elderly health in the society which is return increases their life of expectancy and improve their quality of life and this is one of the objectives that falls under having a vibrant society which is one of the three main pearls in Kingdom’s vision, 2030. In addition to that, all previous studies that published in Saudi Arabia were using AGS Beers Criteria in evaluating the PIM in geriatric patients. We conducted this study to identify and assess the prevalence of PIMs, POMs and polypharmacy among our geriatric patients during their hospital admission by using the STOPP/START and AGS Beer's criteria and to recognize the risk factors that frequently associated with recorded PIMs.
Methods
It is a prospective cohort study that conducted on all patients aged 65 years and over who admitted under internal medicine services during the study period (from April until October 2021) at King Saud University Medical City (KSUMC), is a tertiary care academic medical center with decades of experience in multi-facility and multi-disciplinary administration. The hospital capacity is for 800 to 1200 beds and admit approximately 45,966 patients every year. All patients’ information were collected from each patient’s admission note from hospital system (esiHi) upon admission to emergency department. Standard demographic details, main clinical reason for hospital admission, patients’ medical comorbidities, concurrent and home medications (including oral, intravenous, and inhaled medications), biochemistry laboratory and diagnostic tests were collected. Every morning, the primary researcher check the patient who admitted during the last 24 hours under internal medicine services, and identified the older patient who candidate for recruitment into the study. Patient were classified based on their age as following: ≤ 75 and > 75 years. No written informed consent was required for this study, according to Institutional Review Board (IRB) recommendation. Patients younger than 65years old, admission directly to the intensive care unit or patient who referred to a service other than internal medicine services and palliative care patients were excluded.
The STOPP/START and AGS Beer's criteria were applied to the patient's clinical profile and concurrent medications list at a single time point during 48 hours of admission, and the identified PIMs and POMs were recorded in the collection sheet for reach patient. The study assessed all STOPP/START criteria except for START criteria I (vaccination), because the difficulties in retrieving the information from patient chart as some patient received them in another hospital. Polypharmacy defined as numeric count of prescribed medications more than or equal to five. Data was reviewed and confirm independently by two of the authors, with disagreements resolved by a third author. (1 physician and 2 clinical pharmacist or 3 clinical pharmacist). The study prioritized the respect for the dignity of research participants and ensured to protect of research participants’ privacy and provide adequate level of confidentiality to the research data. The study was approved by the IRB of (KSUMC), Riyadh, Saudi Arabia (project No. E-21-5938).
Statistical analysis
Data were analyzed using SPSS 26.0 version statistical software (IBM Inc., Chicago, USA). Descriptive statistics (mean, standard deviation, frequencies and percentages) were used to describe the quantitative and categorical variables. Pearson’s Chi-square test was used to observe the association between categorical study variables (age groups, gender, reasons of admission) and outcome variables (PIMs and POMs by STOPP/START criteria, polypharmacy, and PIMs by AGS Beers criteria). A p-value of <=0.05 was used to report the statistical significance of results.
Data were analyzed using SPSS 26.0 version statistical software (IBM Inc., Chicago, USA). Descriptive statistics (mean, standard deviation, frequencies and percentages) were used to describe the quantitative and categorical variables. Pearson’s Chi-square test was used to observe the association between categorical study variables (age groups, gender, reasons of admission) and outcome variables (PIMs and POMs by STOPP/START criteria, polypharmacy, and PIMs by AGS Beers criteria). A p-value of <=0.05 was used to report the statistical significance of results.
Results
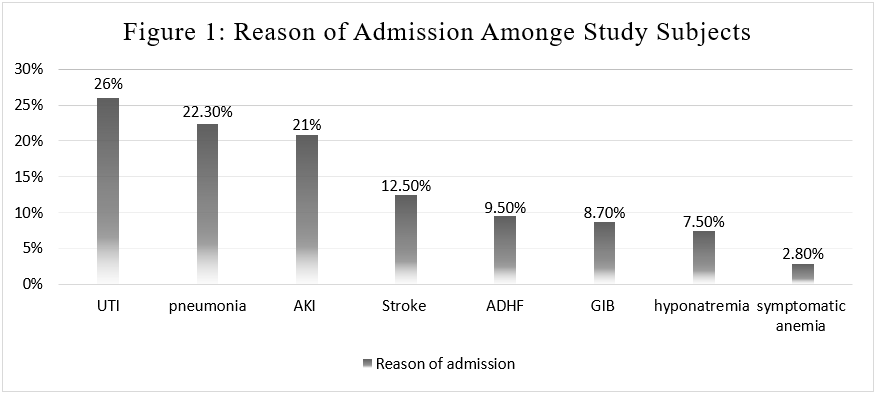
The study included total of 399 subjects, 60.9% were females. The mean of age was 78.16 years (SD= 8.8) and about 60% of them were older than 75 years. Total of eight reasons of admission were recorded as following: urinary tract infection (UTI) 26% (n = 104), pneumonia 22.3% (n= 89), acute kidney injury (AKI) 20.8% (n= 83), stroke 12.5% (n= 50), acute decompensated heart failure (ADHF) 9.5% (n= 38), hyponatremia 7.5% (n=30), symptomatic anemia 2.8% (n=11) and gastrointestinal bleeding (GIB) 2.5% (n= 10). (Figure 1) About 65% of study subjects had only one reason of admission, 28.1% of them had two reasons of admission and only 6.3% of them three reasons of admission. (Table 1)
| Characteristics | No. (%) |
| Age groups: | |
| <=75 years | 159(39.8) |
| >75 years | 240(60.2) |
| Gender: | |
| Male | 156(39.1) |
| Female | 243(60.9) |
| Reason for admission: | |
| UTI | 104 (26) |
| Pneumonia | 89 (22.3) |
| AKI | 83 (20.8) |
| Stroke | 50 (12.5) |
| ADHF | 38 (9.5) |
| Hyponatremia | 30 (7.5) |
| Symptomatic anemia | 11 (2.8) |
| GIB | 10 (2.5) |
| Number of Reasons: | |
| 1 | 262(65.7) |
| 2 | 112(28.1) |
| 3 | 25(6.3) |
Table 1: Basic Demographic and clinical characteristics of study subjects (n=399).
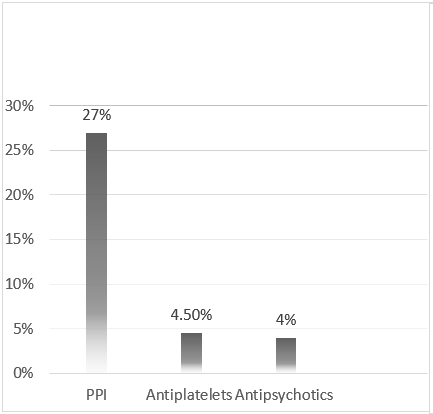
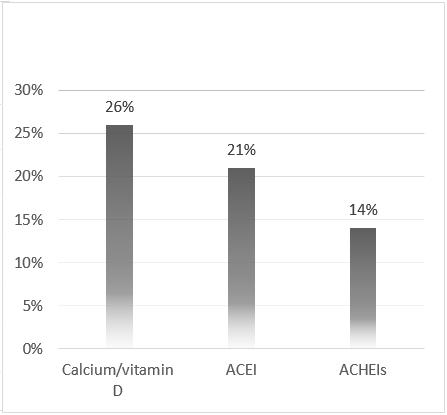
The recorded PIMs by using STOPP/START criteria was obtained in 52.1% (n= 208) of the study subjects who need to avoid at least 1 to 2 medications, and 3.8% need to avoid more than 2 medications. However, POMs were found in 48.9% (n=195) of the study subjects who need to start 3 to 4 medications, followed by 40.1% (n=160) required to start 1 to 2 medications. On the other hand, PIMs was observed in 38.6% of study subjects who required to avoid 1 to 2 medications by using AGS Beers criteria. The prevalence of Polypharmacy in our study subjects was 82.2%. (Table 2) The most common recorded PIMs among study subjects were with proton pump inhibitor (PPIs) (27%) followed by antiplatelets (4.5%) then antipsychotics (4%). (Figure 2) While the most common recorded POMs were with calcium and vitamin-D supplement (26%), followed by angiotensin converting enzyme inhibitor (ACEI) and Acetylcholinesterase inhibitor (AChEIs) (21% and 14%, respectively). (Figure 3)
| Variables | N (%) |
| PIMs by STOPP (n = 291): | |
| 0 | 176(44.1) |
| 1 to 2 | 208(52.1) |
| >2 | 15(3.8) |
| PIMs by Beer’s (n= 168): | |
| 0 | 245(61.4) |
| 1 to 2 | 154(38.6) |
| POMs by START (n= 406): | |
| 1 to 2 | 160(40.1) |
| 3 to 4 | 195(48.9) |
| >4 | 44(11.0) |
Table 2: Distribution of outcome variables among the study subjects.
The bivariate analysis shows no statistically significant association between age groups, gender number of reasons for admission and PIMs by using both STOPP and AGS Beer’s criteria. (Table 3, 4) Out of the 3 study variables, only gender was statistically significantly associated with POMs, in which higher proportion (14.8%) female subjects required >4 medications need to start when compared with 5.1% male subjects, whereas 53.2% male subjects required 3 to 4 medications need to start when compared with 46.1% of female subjects (p=0.010). (Table 5) The prevalence of polypharmacy and recorded PIMs by AGS Beers criteria were not statistically significantly associated with age groups, gender and number of admission reasons. (Table 6)
| Study variables | PIMs by STOPP (%) | Χ2-value | p-value | ||
| 0 | 1 to 2 | >2 | |||
| Age groups | |||||
| <=75 years | 60(37.7) | 92(57.9) | 7(4.4) | 4.391 | 0.111 |
| > 75 years | 116(48.3) | 116(48.3) | 8(3.3) | ||
| Gender | |||||
| Male | 65(41.7) | 84(53.8) | 7(4.5) | ||
| Female | 111(45.7) | 124(51.0) | 8(3.3) | 0.85 | 0.653 |
| No. of Reasons for admission | |||||
| 1 | 124(47.3) | 131(50.0) | 7(2.7) | 5.37 | 0.251 |
| 2 | 42(37.5) | 64(57.1) | 6(5.4) | ||
| 3 | 10(40.0) | 13(52.0) | 2(8.0) | ||
Table 3: Association between the Study variables and PIMs by STOPP criteria.
| Study variables | PIMs by Beer’s (%) | Χ2-value | p-value | |
| 0 | 1 to 2 | |||
| Age groups | ||||
| <=75 years | 94(59.1) | 65(40.9) | 0.58 | 0.446 |
| >75 years | 151(62.9) | 89(37.1) | ||
| Gender | ||||
| Male | 87(55.8) | 69(44.2) | 3.43 | 0.064 |
| Female | 158(65.0) | 85(35.0) | ||
| No. of Reasons for admission | ||||
| 1 | 165(63.0) | 97(37.0) | 1.20 | 0.548 |
| 2 | 64(57.1) | 48(42.9) | ||
| 3 | 16(64.0) | 9(36.0) | ||
Table 4: Association between the Study variables and PIMs by Beer’s criteria.
| Study variables | POMs by START (%) | Χ2-value | p-value | ||
| 1 to2 | 3 to 4 | >4 | |||
| Age groups | |||||
| <=75 years | 72(45.3) | 70(44.0) | 17(10.7) | 3.068 | 0.216 |
| >75 years | 88(36.7) | 125(52.1) | 27(11.3) | ||
| Gender | |||||
| Male | 65(41.7) | 83(53.2) | 8(5.1) | 9.22 | 0.010 |
| Female | 95(39.1) | 112(46.1) | 36(14.8) | ||
| No. of Reasons for admission | |||||
| 1 | 109(41.6) | 125(47.7) | 28(10.7) | 6.09 | 0.192 |
| 2 | 46(41.1) | 52(46.4) | 14(12.5) | ||
| 3 | 5(20.0) | 18(72.0) | 2(8.0) | ||
Table 5: Association between the Study variables and POMs by START criteria.
| Study variables | Polypharmacy (%) | Χ2-value | p-value | |
| Yes | No | |||
| Age groups | ||||
| <=75 years | 135(84.9) | 24(15.1) | 1.317 | 0.251 |
| >75 years | 193(80.4) | 47(19.6) | ||
| Gender | ||||
| Male | 128(82.1) | 28(17.9) | ||
| Female | 200(82.3) | 43(17.7) | 0.004 | 0.949 |
| No. of Reasons for admission | ||||
| 1 | 215(82.1) | 47(17.9) | ||
| 2 | 90(80.4) | 22(19.6) | 1.905 | 0.386 |
| 3 | 23(92.0) | 2(8.0) | ||
Table 6: Association between the Study variables and Polypharmacy.
| Age groups | PIMs by Beer’s criteria | PIMs by STOPP criteria (%) | Total | Kappa Statistic | p-value | |
| 0 | >=1 | |||||
| <=75 | 0 | 60(63.8) | 34(36.2) | 94(100) | 0.591 | <0.0001 |
| >=1 | 0(0.0) | 65(100) | 65(100) | |||
| Total | 60(37.7) | 99(62.3) | 159(100) | |||
| >75 | 0 | 115(76.2) | 36(23.8) | 151(100) | 0.694 | <0.0001 |
| >1 | 1(1.1) | 88(98.9) | 89(100) | |||
| Total | 116(48.3) | 124(51.7) | 240(100) | |||
Table 7: Agreement between Beer’s and STOPP criteria for PIMs in study participants’ age groups.
| Gender | PIMs by Beer’s criteria | PIMs by STOPP criteria (%) | Total | Kappa Statistic | p-value | |
| 0 | >=1 | |||||
| Male | 0 | 65(74.7) | 22(25.3) | 87(100) | 0.723 | <0.0001 |
| >=1 | 0(0.0) | 69(100) | 68(100) | |||
| Total | 65(41.7) | 91(58.3) | 156(100) | |||
| Female | 0 | 110(69.6) | 48(30.4) | 158(100) | 0.607 | <0.0001 |
| >1 | 1(1.2) | 84(98.8) | 85(100) | |||
| Total | 111(45.7) | 132(54.3) | 243(100) | |||
Table 8: Agreement between Beer’s and STOPP criteria for PIMs in study participants’ gender.
| No. of reasons for admission | PIMs by Beer’s criteria | PIM by STOPP criteria | Total | Kappa Statistic | p-value | |
| 0 | >=1 | |||||
| 1 | 0 | 123(74.5) | 42(25.5) | 165(100) | 0.677 | <0.0001 |
| >=1 | 1(1.0) | 9699.0) | 97(100) | |||
| Total | 124(47.3) | 138((52.7) | 262(100) | |||
| 2 | 0 | 42(65.6) | 22(34.4) | 64(100) | 0.621 | <0.0001 |
| >1 | 0(0.0) | 48(100) | 48(100) | |||
| Total | 42(37.5) | 70(62.5) | 112(100) | |||
| 3 | 0 | 10(62.5) | 6(37.5) | 16(100) | 0.545 | 0.002 |
| >1 | 0(0.0) | 9(100) | 9(100) | |||
| Total | 10(40.0) | 15(60.0) | 25(100) | |||
Table 9: Agreement between Beer’s and STOPP criteria for PIMs in relation to the number of reasons for admission.
Discussion
The objectives of our study was to identify and assess the prevalence of PIMs, POMs and polypharmacy in geriatric patients in an inpatient setting via using the STOPP/START and AGS Beer's criteria then to recognize the risk factors that frequently associated with recorded PIMs. Up to our knowledge, there are no previous published studies that comparing between STOPP/START and Beers Criteria in Saudi Arabia. In addition to that, this study was prospectively conducted in one of the biggest educational tertiary hospitals in Saudi Arabia which is consider a strength points for our study.
52% of study subjects found to have at least one medication need to avoid (PIMs) by using STOPP criteria, while 38.6% by using AGS Beers criteria. Based on our data, STOPP criteria identified higher percentage of PIMs than Beers criteria. A study published by Márcio G. et al, in 2015 is contradicting our findings, they concluded that, the Beers criteria (2012) identified higher number of PIMs than the STOPP criteria. (8) In contrast, Diana Ching, et al, presented a poster in RISE, 2016, and she determined that there is significant overlap between both criteria although they found that five STOPP and two START criteria were not available in Beers criteria. [9]
One of the common reason of recorded PIM in this study was ploypharmacy, which was found in 82.2% of study subjects. Another reason were multiple comorbidities, advance age, poorly controlled chronic conditions, and functional impairment. All mentioned factors are responsible for increase the risk of ADR, drug-drug interaction and falls which lead to disability and frailty.
The percentage of the study subjects who need to start 3 to 4 medications (48.9%) was higher than the study subjects who need to start 1 to 2 medications (40.1%). The most common reason of recorded POM in this study was patient’s home-medications omission upon admission with no obvious contraindication was documented in patients’ chart to discontinue these medications during hospitalization.
The predominant PIMs was recorded with PPIs, most of study subjects were on PPI as a part of their home medications and some of them were started during hospital admission as stress ulcer prophylaxis. Those population who was on PPIs as a part of their home medication, had no previous or current history of GIB, peptic ulcer disease (PUD) nor gastrointestinal reflux disease (GERD) were documented in their chart. PPIs are well known to cause osteopenia/ osteoporosis due to decrease calcium absorption which will leads to increase risk of falls and hospitalization. However, the frequent POMs was obtained with calcium and vitamin-D supplement. This POMs was found in patients with positive history of immobility, falls, fractures, osteopenia and osteoporosis.
This study as many previous studies showed high prevalence of PIMs in geriatrics population during hospital admission. Patient counseling, medication reconciliation, electronic health system alert for PIMs order and educational sessions for prescriber about the safe alternative for the recorded PIMs is crucial to minimize all types of medical errors in this population. Applying a criteria like STOPP/START or Beers is recommended to improve medications dispensing process and minimize ADRs, drug- drug interactions and polypharmacy. Well established geriatric multidisciplinary team included (physician, pharmacist and nurse) is necessary to inspect the possible causes the leads to that high prevalence and to develop a structured action plan to improve the compliance to the applied criteria with periodic assessment to healthcare providers adherence to that criteria in inpatient settings.
Conclusion
PIMs, POMs, and polypharmacy were prevalent among our geriatric population. It requires further assessment to see the impact of our health care outcomes. Standard criteria like STOPP/START or AGS Beer's should be implemented before prescribing medications in geriatrics to improve prescribing practice in these settings.
References
- Gallagher P, et al, (2008). STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther ; 46: 72–83.
- O'Mahony D, (2014 ). STOPP/START criteria for potentially inappropriate prescribing in older people: version 2, Age Ageing. 2015; 44(2):213. Epub 2014 Oct 16.
- Bader A.Alqahtani, (2019). Prevalence of falls among older adults in the Gulf Cooperation Council countries: A systematic review and meta-analysis, Archives of gerontology and geriatrics, Volume 83, July–August, Pages 169-174.
- Amy Copperthwaite, et al, {2016}. 139 Application of the Gerontonet ADR Risk Score to Assess the Risk of Adverse Drug Reactions in Patients Over 65 Year, Age and Ageing, Volume 45, Issue suppl_2, September, Pages ii13–ii56.
- Gallagher P, O'Mahony D, (2008). STOPP (Screening Tool of Older Persons' potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers' criteria. Age Ageing. 37(6):673. Epub 2008 Oct 1
- Hamilton H, et al, (2011). potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med. 171(11):1013.
- Marie N. O’Connor, et al, (2016). Prevention of Hospital-Acquired Adverse Drug Reactions in Older People Using Screening Tool of Older Persons’ Prescriptions and Screening Tool to Alert to Right Treatment Criteria: A Cluster Randomized Controlled Trial, J Am Geriatr Soc, Aug;64(8):1558-66.c6
- Márcio Galvão Oliveira, et al, (2015). A comparison of the Beers and STOPP criteria for identifying the use of potentially inappropriate medications among elderly patients in primary care, Journal of Evaluation in Clinical Practice 21 320–325 © 2015.
- Diana Ching, (2016), A Comparison of the STOPP/START Criteria and the Beers Criteria for the U.S. Nursing Home Population (poster), Research Innovation and Scholarship Expo (RISE), Northeastern University.
Citation: Metwali H, Mayet A and Alayed K. (2024). Evaluation the Appropriateness of Geriatrics’ Medications by Using STOPP/START and Beer’s Criteria in Tertiary Care Center in Saudi Arabia. Journal of Pharmacy and Drug Development 6(1). DOi: 10.5281/zenodo.14252773
Copyright: © 2024 Metwali H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.