Research Article
Volume 5 Issue 1 - 2023
Investigation of lead-poisoning in Patients with Opium Addiction in Baharlou Hospital in Tehran from June 2017 to June 2018
1Department of Pharmaceutical Care, Baharloo hospital, Tehran University of medical science, Tehran, Iran
2Department of Forensic medicine and toxicology, Faculty of Medicine, Tehran University of Medical sciences, Tehran, Iran
3School of Pharmacy, Tehran University of medical science (TUMS), Tehran, Iran
2Department of Forensic medicine and toxicology, Faculty of Medicine, Tehran University of Medical sciences, Tehran, Iran
3School of Pharmacy, Tehran University of medical science (TUMS), Tehran, Iran
*Corresponding Author: Behnam Behnoush, Department of Forensic medicine and toxicology, Faculty of Medicine, Tehran University of Medical sciences, Tehran, Iran.
Received: May 18, 2023; Published: May 31, 2023
Introduction
Lead can cause acute and chronic poisoning in humans [1] and acts as a toxic substance on multiple body systems [2]. Lead poisoning might result from inhalation, ingestion or skin contact with organic lead [3]. About 90-95% of the absorbed lead is stored in the cortical bones, teeth, liver, brain and kidneys. 75% of the lead is secreted then removed by the kidneys and the remainder is excreted through the digestive system and skin (sweating), or accumulated in nails and hair [4-6]. Lead poisoning typically manifests with signs and symptoms like nausea, abdominal pain, constipation, irritability, and attention deficit disorder. Also, chronic exposure to low levels of lead can increase the risk of hypertension and cognitive malfunction in adults. Although digestive tract is not the principal route by which lead is absorbed, it is considered a major route of lead entry into the body in children as well as in adults following oral ingestion of lead contaminated food [7].
Substance abuse is a major health problem in Iran [8, 9]. Opium and its derivatives are the most commonly used drugs in Iran [8]. There have been several reports on increased lead poisoning due to drug abuse, which are often associated with opium [6, 10]. Some poisoning cases with marijuana [11] and methamphetamines have also been reported [12]. In short, Opium becomes contaminated with lead mainly due to adulteration, so the substance (opium) weighs more. Other causes of contamination are lead-contaminated poppy fields or opium production tools [5, 10, 13-16].
Hence, according to the aforementioned information, determining the relationship between lead poisoning and opium addiction would be absolutely noteworthy. In this study, we have aimed to investigate the factors affecting this correlation by means of descriptive and analytical statistics. The results of this study can be applied to establishing new plans in order to avoid high rate of morbidity and mortality caused by lead poisoning.
Patients and Methods
This study was a cross-sectional study that was conducted from June 2017 to June 2018 at Baharloo Hospital, one of the main centers of toxicology in Tehran. Adults with signs and symptoms of lead poisoning, which also had high blood level of lead (i.e. Equal to or greater than 45 μg/dL), were admitted to poisoning department. Among the patients, those who were consuming opium were selected for study. A complete history of patients and their relatives were obtained and necessary tests were carried out. After omitting patients with a history of environmental or occupational lead poisoning, 50 patients with confirmed lead poisoning selected. The study and its objectives were explained to patients or their companions. Written consents about the use of their medical information were obtained. The confidentiality of the patients’ information and their privacy had been approved by ethics committee of Tehran University of Medical Sciences. The data gathering tool was a questionnaire consisting of two parts: the first part was about demographic characteristics, and the second part was a standardized questionnaire to assess the clinical status and laboratory findings of the patients. In this questionnaire, the information was completed through examination and interview with the patient or the person accompanying the patient (if the patient was not alert). The patients were treated with appropriate drug regimen. Results of Para clinical tests, course of the disease, and response to treatment were investigated. Blood levels of lead were followed up and recorded. Raw data was entered into SPSS software (version 25.0) and then analyzed. P value<0.05 were considered as statistically significant. To explore the data, descriptive statistics (mean, standard deviation, frequency and percentage) were evaluated. The T- test (independent and paired sample) was used for two-group comparison of variables. In order to assess the relationship between BLL and hemoglobin, hematocrit, creatinine, alanine transaminase, aspartate transaminase, alkaline phosphatase, duration and amount of consumed opium the Pearson correlation test was used. The studied variables were gender, age, amount and duration of opium use, abnormal laboratory results, and blood lead levels before and after treatment, gastrointestinal symptoms, hematological symptoms, neurological symptoms, renal symptoms, other symptoms, permanent complications, type of treatment, mortality, duration of admission, and patient’s condition when dismissing.
Results
In total, 50 patients were included in the study, 94% of which were male. The average age of cases was 48.3 ± 11.99 years. In this study, signs and symptoms of lead poisoning were widespread. The frequency of clinical findings, in order of importance, were gastrointestinal (96%), hematologic (80%), neurological (22%) and other findings (30%). The most common gastrointestinal findings was abdominal pain (94%) and the most common neurological findings was fatigue (46%). The mean blood lead level before treatment was not significantly affected by existence or lack of related symptoms.
Abnormal Hematological test results were detected in 80% of patients and abnormal liver tests in 22%. Renal tests were normal in all patients. The most common hematological finding was anemia (80%).
The mean blood lead level (BLL) before treatment was 91.342 μg/dL and the mean blood lead level after treatment was 34.796 μg/dL. Based on Paired Samples Test, blood lead levels alterations were significant during the time (before and after treatment) (Sig.2-tailed = 0).
According to the results of the Pearson correlation test, there was no significant correlation between the duration of opium use and blood lead levels before treatment (r = 0.235, p = 0.101). Similarly, no significant correlation between the amount of consumed opium and blood lead level before treatment was found (r = -0.59, p = 0.683).
Table 1 shows correlation between the results of laboratory tests and blood lead levels before treatment.
| Hb | Hct | Cr | ALT | AST | ALK_P | ||
| Pre-treatment BLL | Pearson Correlation | -.286* | -.337* | .181 | -.058 | .119 | .262 |
| Sig. (2-tailed) | .044 | .017 | .209 | .691 | .410 | .066 | |
| N | 50 | 50 | 50 | 50 | 50 | 50 | |
Table 1: Pearson corelation test.
Based on Pearson correlation test, there was a significant correlation between hemoglobin concentration and blood lead level before treatment (r=-0.286, p=0.044) .Also, correlation between hematocrit and blood lead level before treatment was significant (r =-0.337, p = 0.017) .No significant correlation was found between pre-treatment BLL and all of the following parameters separately: creatinine, alanine transaminase (ALT), aspartate transaminase (AST) and alkaline phosphatase.
Table 2 shows the Difference in blood lead level before and after treatment in the prescribed regimens.
| drug | Mean | Std. Deviation | t | df | Sig. (2-tailed) | ||
| EDTA | Pair 1 | Pre-treatment BLL – post-treatment BLL | 30.4560 | 13.5372 | 11.249 | 24 | .000 |
| EDTA + BAL | Pair 1 | Pre-treatment BLL – post-treatment BLL | 91.3909 | 54.5056 | 7.865 | 21 | .000 |
| D-penicillamine | Pair 1 | Pre-treatment BLL – post-treatment BLL | 18.4333 | 8.2440 | 3.873 | 2 | .061 |
Table 2: Paired Samples T Test.
According to the results of the paired sample T test, the mean blood lead level in patients undergoing EDTA and BAL + EDTA regimen had decreased significantly (Sig.2-tailed = 0). However in patients under D-penicillamine regimen no significant change in mean blood lead level was seen (Sig.2-tailed = 0.061).
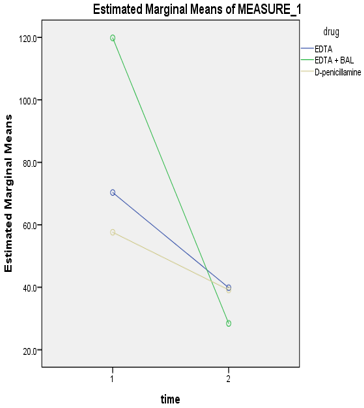
Based on the figure, the level of blood lead reduction in patients treated with the BAL + EDTA regimen was higher than other regimens. The reduction in blood lead levels in patients treated with D-penicillamine was less than two other drug regimens.
According to Pearson correlation test there was significant correlation between duration of hospitalization and blood lead level before treatment (r = 0.433, p = 0.002).
Based on independent t test, blood lead level before and after treatment was not significantly correlated with mortality. In addition, laboratory tests did not have a significant relationship with mortality.
Discussion
In this study, 50 oral opium-addicted patients, with lead poisoning, who were admitted at Baharloo Hospital in Tehran from June 2017 to June 2018 were evaluated. 47 of them (94%) were male and 3 (6%) were female, which was roughly the same sexual distribution as of Meybodi et al. (96% male) [17]. In a study by Hayatbakhsh et al. 79% [18] , Khatibi-Moghaddam et al. 87.5% [19] and in the study conducted by Amiri and Amini [20] and Froutan et al. [21] all of the patients were male. This difference may be due to the increased risk of men being addicted [21] and thus higher prevalence of addiction among men [22].
The mean age of patients in our study was 48.3 years. The mean age of the patients in most of other studies is almost the same as ours [19-21], however in some studies it is somewhat different [5, 14, 17, 23].
The average daily intake of opium in this study was 3.49 grams, which is approximately similar to the study by Salehi et al (3.03 g) [5] and almost similar to the Khatibi-Moghadam et al. (4.3 g) [19]. In current study, there was no significant relationship between daily intake of opium and blood level of lead before treatment, which was similar to that of Froutan et al.[21] and contrary to Salehi et al.[5]. It is probably due to the difference in the level of lead contamination in opium use.
The duration of opium use by patients in this study had a wide range from one year to 40 years, which was roughly the same as the study by Meybodi et al. (Between 3 months and 40 years) [17]. The average duration of opium use in the patients was 16.04 years, which is approximately the same as the study by Khatibi-Moghadam et al (17 years)[19] and the study by Froutan et al (17.5 years) [21]. In our study, no significant relationship was found between the duration of opium use and blood lead levels before treatment, which was similar to the studies by Meybodi et al.[17] and Salehi et al.[5], and contrary to the study by Khatibi-Moghadam et al.[19]. The reason for the lack of a meaningful relationship between the duration of opium use and blood lead levels before treatment may be due to inaccurate information on the exact duration of the use of lead-contaminated opium.
The mean lead level of the blood before treatment was 91 μg/dL, which is similar to the study of Hayatbakhsh et al. (91.02 μg/dL) [18] and almost the same as Farzaneh et al. (93.36 μg/dL) [24]. The difference in blood lead levels before treatment with some similar studies, could indicate a difference in the amount of opium-lead contamination in recent years.
In this study, the most common complaints and clinical symptoms were in the digestive tract (96% of patients). And the most common gastrointestinal symptoms were abdominal pain (94%), constipation (54%), anorexia (52%), nausea and vomiting (24%), gum discoloration (18%) and metal taste (14%). Similarly, the most common complaints were gastrointestinal complaints in Hayatbakhsh et al.[18] study; abdominal pain (86.9%), constipation (75.8%), anorexia (71.5%), and nausea (54.7%). In our study, the prevalence of gastrointestinal findings, especially abdominal pain, was clinically significant. Abdominal pain in these patients may be confused with the acute abdomen. Therefore, Lead poisoning to be considered as a differential diagnosis in patients with abdominal pain and consuming opium. In the study by Meybodi et al.[17] and Mokhtarifar et al.[25], patients with abdominal pain were mistaken with other diagnoses such as cholecystitis, renal colic, acute abdomen, and generalized ileus. Meybodi et al.[17] reported the predominance of gastrointestinal complaints; anorexia (96%), Constipation (88%) and nausea was reported in 56% of patients [17]. Opiates like opium, can reduce gastrointestinal motility and cause constipation, which can also increase the duration of exposure and consequently increase the absorption of lead-contaminated opium from the gastrointestinal tract. In Baker et al. study, colic abdominal pain was in 47% of patients with occupational lead poisoning [27].
In our study, the neurological symptom were in descending frequency, fatigue (46%), insomnia (18%), headache (6%), tremor (6%), seizure (6%), decreased consciousness (6%), dizziness (4%), moodiness (4%), visual impairment (2%), foot drop (2%), wrist drop (2%) and incoordination (2%). In the study of Hayatbakhsh et al., 32.7% of patients had insomnia and 3.7% of patients had peripheral neuropathy [18]. In the study by Meybodi et al., visual impairment was seen in 20% of patients and wrist drop was observed in 4% [17]. Due to irreversible neurological damage in patients with neurological symptoms, special attention is needed in the diagnosis and treatment of lead poisoning in this group of patients. Although neurological symptoms had no significant relationship with blood lead level before treatment, both patients died and also a complicated patient had neurological symptoms.
Muscle weakness was observed in 12% of patients, arthralgia in 8%, and myalgia in 2%. In Hayatbakhsh et al. study, muscle weakness had been seen in 47.4% of patients, arthralgia in 38.1%, and myalgia in 33.2% [18]. Meybodi et al. reported muscle weakness in 92% of patients and limb pain in 88% of cases [17]. Since many symptoms and signs of lead poisoning are nonspecific, patients with this symptoms and signs and risk of poisoning, including opium users, should be given priority to measure blood lead level.
In the study by Alinejad et al. [15] the most common complaints were abdominal pain with anemia and neurologic complaints [10]. Karrari et al. reported that most common complaints were abdominal pain, arthralgia and myalgia in their study [26]. In Baker et al. study, forearm extensor muscle weakness was in 17%, and encephalopathy was reported in 2.8% of patients with occupational lead poisoning [27].
The gum discoloration (lead line) was seen in 18% of patients, which was almost the same as the study by Froutan et al. (20%) [21].
Anemia was observed in 80% of patients and basophilic stippling was seen in 10%. All patients with basophilic stippling had anemia. The mean hemoglobin concentration in this study was 10.604 g/dL, which was approximately the same as the mean of hemoglobin in the study by Meybodi et al. (10.5g/dL) [17]. In our study, there was significant correlation between hemoglobin concentration and blood lead level before treatment, which was the same as the study by Hayatbakhsh et al. [18]. The possibility of the existence of chronic diseases and lack of care and malnutrition in drug dependent patients may be involved in their anemia. In the study by Baker et al., Anemia was reported in 38.5% of patients with occupational lead poisoning which is much less than our study and similar studies [27].
Liver function abnormalities were observed in 22% of patients. ALT was increased in 18% of patients and AST increased in 16%. Both enzymes increased in 12% of patients. Lead poisoning can lead to liver damage and increased liver enzymes, but it is also important to consider the possibility of misuse of other substances, such as alcohol, and other liver diseases, such as the type of hepatitis in the drug users there is also the possibility of contamination of other metals in opium. ALT increased by 36% and AST increased in 42.2% of the patients in the study by Hayatbakhsh et al. [18].
In this study, there was no increase in serum creatinine in any patient, as in the study of Froutan et al. [21]. The average duration of complaints in the patients was 22.42 days. In Meybodi et al., The average length of complaints was 28.1 days[17].
The reduction in blood lead levels in patients treated with the BAL + EDTA regimen was higher than the other regimens, and this was lower in patients treated with D-penicillamine than in the other two regimens. Due to the fact that in patients treated with D-penicillamine were more treatment on an outpatient basis and outside the hospital, there was no full assurance of regular drug use and that may reduce the blood lead level is much less than in the other groups.
The most important limitation of our study was the lack of control group. Also, since the increase in blood levels of lead in opium users depends on the amount of opium contamination with lead and we were not able to analyze the patient's opium samples from the lead content, Additionally, we could not establish a close relationship between the severity of symptoms and the amount of lead consumed. Opium analysis of patients is recommended for future studies. Also, we were not able to accurately determine the length of time in which patients had consumed lead-contaminated opium. In addition to lead, there may be other contaminants in opium that require the attention and identification of existing impurities for appropriate therapeutic measures and needs further studies. It is recommended that a study be conducted on oral opium addicts without lead poisoning and oral opium addicts with lead poisoning. A similar study is suggested in comparison with occupational lead poisoning. Also it is recommended that a similar research be carried out over a longer period and with a larger sample size in the future.
Conclusion
Based on the findings of this study, the prevalence of lead poisoning is obviously higher in oral opium addicts. Consequently, oral use of lead-contaminated opium can cause lead poisoning.
Regarding the high incidence of gastrointestinal symptoms, especially abdominal pain, it is recommended that lead poisoning in opium consumers with gastrointestinal symptoms should be always considered.
The high prevalence of anemia in these patients is an indication of evaluation for lead toxicity in anemic opium addict patients.
Due to non-specific signs and symptoms of lead poisoning, each opium consumer with non-specific symptoms should consider lead poisoning as a differential diagnosis.
The reduction in blood lead levels in patients treated with the BAL + EDTA regimen was higher than other drug regimens and in severe lead poisoning this regimen is recommended.
References
- Azizi, M., F.J.T.i.j.o.o. Azizi, and e. medicine, (2010). Lead poisoning in the world and Iran. Int J Occup Environ Med. 1(2): 81-7.
- Goldfrank's Toxicologic Emergencies. 9 ed. (2011).
- Karrari, P., O. Mehrpour, and M.J.D.J.o.P.S. Abdollahi, (2012). A systematic review on status of lead pollution and toxicity in Iran; Guidance for preventive measures. Daru. 20(1): p. 2.
- Algora, M., et al. (1989). Lead poisoning due to drug addiction: a new source of poisoning with clinical interest and important epidemiological consequences. in Anales de medicina interna (Madrid, Spain: 1984) 6.9: 483-5.
- Salehi, H., et al., (2009). Comparison of serum lead level in oral opium addicts with healthy control group. Arch Iran Med 12(6): 555-8.
- Velez, L. and E. O'Connell, Heavy metals. (2013). Rosen's Emergency Medicine: Concepts and Clinical Practice. Philadelphia, PA: Elsevier Mosby.
- Abbas, A.Z., et al., report of a case of abdominal pain and increased transaminases caused by lead poisoning.
- Mokri, A., (2002). Brief overview of the status of drug abuse in Iran.
- Faranoush, et al., (2009). Investigation of lead contamination and some factors related to it in children aged 6-11 in Semnan city. 2003. 4(3): p. 79-86.
- Chia, B., et al., (1973). Lead poisoning from contaminated opium. 1(5849): p. 354.
- Busse, F., et al., (2008). Lead poisoning due to adulterated marijuana. N Engl J Med 358(15): p. 1641-1642.
- Allcott, J.V., R.A. Barnhart, and L.A.J.J. Mooney, (1987). Acute lead poisoning in two users of illicit methamphetamine. JAMA 258(4): p. 510-511.
- Abbasi, M.M.H., et al., (2010). Lead Serum Levels in Opium-Dependent Individuals. Addict Health. 1(2).
- Aghaee-Afshar, M., et al., (2008). Presence of lead in opium. 11(5): p. 553-4.
- Alinejad, S., et al., (2018). Clinical aspects of opium adulterated with lead in Iran: a review. Basic Clin Pharmacol Toxicol 122(1): p. 56-64.
- Khoshgovar, M., (2016). Lead poisoning with substances; Diagnosis and treatment %J Persian Quarterly Journal of Addiction.3(No. 12-13): p. 55-57.
- Meybodi, F.A., et al., (2012). Oral opium: an unusual cause of lead poisoning. Singapore Med J 53(6): p. 395-7.
- Hayatbakhsh, M.M., et al., (2017). Lead poisoning among opium users in Iran: an emerging health hazard. Substance Abuse Treatment, Prevention, and Policy 12(1): p. 43.
- Khatibi-Moghadam, H., et al., (2016). Comparison of serum and urine lead levels in opium addicts with healthy control group. 35(8): p. 861-865.
- Amiri, M. and R.J.I.R.C.M.J. Amini. (2012). A comparison of blood-lead level (BLL) in opium-dependant addicts with healthy control group using the graphite furnace/atomic absorption spectroscopy (GF-AAS) followed by chemometric analysis. Iran Red Crescent Med J. 14(8): p. 488.
- Froutan, H., et al., (2011). Lead toxicity: a probable cause of abdominal pain in drug abusers. 25(1): p. 16-20.
- Nikfarjam, A., et al., (2016). National population size estimation of illicit drug users through the network scale-up method in 2013 in Iran. Int J Drug Policy 31: 147-152.
- Soltaninejad, K., A. Flückiger, and S.J.J.o.S.U. (2011). Shadnia, Opium addiction and lead poisoning. 16(3): p. 208-212.
- Farzaneh, E., et al., (2017). Lead Toxicity among Oral Opium Addicts with Abdominal Pain: A Case Series of 17 Cases. 11(2).
- Mokhtarifar, A., et al., (2013). Cholestasis and seizure due to lead toxicity: a case report. Hepat Mon 13(11).
- Karrari, P., et al., (2013). Pattern of illicit drug use in patients referred to addiction treatment centres in Birjand, Eastern Iran. J Pak Med Assoc. 63(6): p. 711-6.
- Baker, E., et al., (1979). Occupational lead poisoning in the United States: clinical and biochemical findings related to blood lead levels. 36(4): p. 314-322.
Citation: Nafiseh Alizadeh, Mojdeh Farshadi, Mansoureh Fotouhi and Behnam Behnoush. (2023). Investigation of lead-poisoning in Patients with Opium Addiction in Baharlou Hospital in Tehran from June 2017 to June 2018. Journal of Pharmacy and Drug Development 5(1).
Copyright: © 2023 Behnam Behnoush. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.