Case Report
Volume 5 Issue 1 - 2023
Transnasal Endoscopic Repair of Unilateral Choanal Atresia Using Cross-over Flap Technique: A Case Report
1MS (ENT) Senior resident Department of ENT and Head-Neck surgery Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar Dehradun
2MS (ENT) Professor & Head Department of ENT and Head-Neck Surgery Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar Dehradun
3MD (pathology) Professor Department of Pathology Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar Dehradun, 248001, Uttarakhand, INDIA
2MS (ENT) Professor & Head Department of ENT and Head-Neck Surgery Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar Dehradun
3MD (pathology) Professor Department of Pathology Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar Dehradun, 248001, Uttarakhand, INDIA
*Corresponding Author: Dr. Apoorva Kumar Pandey, (MS. ENT) Professor & Head Department of ENT and Head-Neck surgery SGRR Institute of Medical & Health Sciences, Dehradun, 248001, Uttarakhand, India.
Received: May 24, 2023; Published: June 05, 2023
Abstract
This case report describes the presentation, diagnosis and management of a patient with unilateral choanal atresia. Unilateral choanal atresia is a rare congenital anomaly characterized by the partial or complete obstruction of one nasal passage due to the abnormal development of the posterior nasal choanae. It can result in symptoms such as nasal obstruction, difficulty breathing and recurrent sinus infection. Timely diagnosis and appropriate surgical intervention are essential for relieving symptoms and restoring normal nasal airflow.
Introduction
Choanal atresia is a congenital anomaly characterized by the partial or complete blockage of the nasal passages due to abnormal development of the posterior nasal choanae. This results in obstruction to airflow through the nasal cavities, which can lead to respiratory distress and feeding difficulties, particularly in newborns. Choanal atresia is a relatively rare condition, occurring in approximately 1 in 7000 to 8000 live births. [1] Choanal atresia can be unilateral, affecting one nasal passage, or bilateral, affecting both passages. Unilateral Choanal atresia is more common, mostly involving the left side and is more commonly observed in females. [2] Unilateral Choanal atresia mostly remains asymptomatic as compared to bilateral, which is generally more severe and can result in life-threatening respiratory distress shortly after birth. The exact cause of Choanal atresia remains unclear, but is believed to result from a combination of genetic and environmental factors. The condition can occur in isolation or in association with other congenital syndromes, such as CHARGE syndrome and Treacher-Collins syndrome.
Case Report
A 9-year-old male presented to our OPD with complaints of left-sided nasal obstruction and profuse mucoid discharge from the left nasal cavity since childhood.
Clinical findings
On anterior rhinoscopy, there was hypertrophy of the inferior turbinate on the right side with discharge seen in the left nasal cavity. The left nasal cavity was roomier as compared to the right nasal cavity. Cold spatula test and catheter test confirmed the complete obstruction of the left-sided nasal cavity. Findings were confirmed using 0° endoscope. Left-sided nasopharynx could not be visualized because of obstruction (? Membranous).
On anterior rhinoscopy, there was hypertrophy of the inferior turbinate on the right side with discharge seen in the left nasal cavity. The left nasal cavity was roomier as compared to the right nasal cavity. Cold spatula test and catheter test confirmed the complete obstruction of the left-sided nasal cavity. Findings were confirmed using 0° endoscope. Left-sided nasopharynx could not be visualized because of obstruction (? Membranous).
Diagnostic assessment
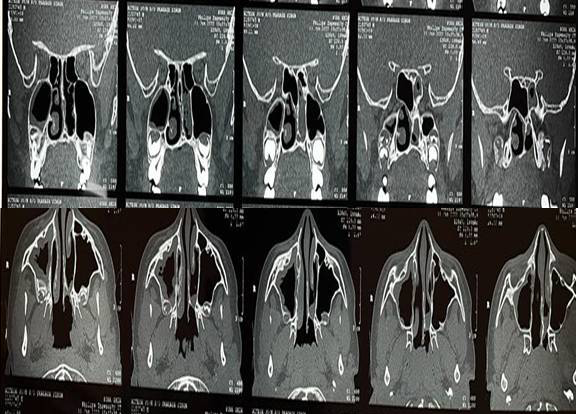
Computed tomography (CT) scan of paranasal sinuses was done, which revealed bony narrowing of the left posterior nasal cavity with posterior membrane resulting in left choanal obstruction (Figure no 1). Findings were consistent with left choanal atresia. There was also mild to moderate mucosal thickening seen in bilateral maxillary sinuses with atrophy of the left nasal turbinate.
Computed tomography (CT) scan of paranasal sinuses was done, which revealed bony narrowing of the left posterior nasal cavity with posterior membrane resulting in left choanal obstruction (Figure no 1). Findings were consistent with left choanal atresia. There was also mild to moderate mucosal thickening seen in bilateral maxillary sinuses with atrophy of the left nasal turbinate.
Therapeutic intervention
The patient underwent transnasal endoscopic repair of Choanal atresia using a cross-over flap technique under general anesthesia. Obstruction was found to be of the bony type, which was punctured and enlarged. Exposed bone was draped using both superior and inferior-based flaps. The superior flap was raised on the blocked side and the inferior-based flap was raised on the patent right side. The superior-based flap covered the raw superior bony area whereas the inferior-based flap covered the inferior raw bony area (figure no 2 [a-f]). Both nasal cavities were packed with merocel packs under antibiotic cover, which was removed on the 5th postoperative day.
The patient underwent transnasal endoscopic repair of Choanal atresia using a cross-over flap technique under general anesthesia. Obstruction was found to be of the bony type, which was punctured and enlarged. Exposed bone was draped using both superior and inferior-based flaps. The superior flap was raised on the blocked side and the inferior-based flap was raised on the patent right side. The superior-based flap covered the raw superior bony area whereas the inferior-based flap covered the inferior raw bony area (figure no 2 [a-f]). Both nasal cavities were packed with merocel packs under antibiotic cover, which was removed on the 5th postoperative day.
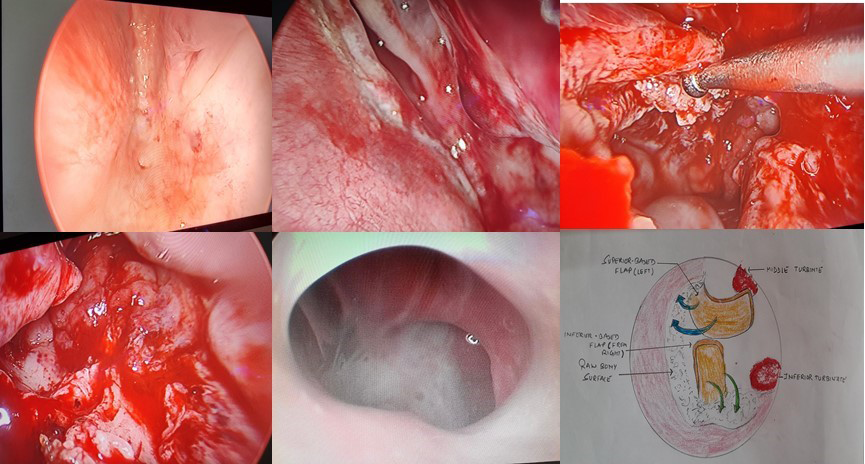
Figure 2: a) endoscopic picture showing left choanal atresia. b) showing the creation of a superior-based flap on the left side using electro-cautery. c) probe showing the superior-based flap. d) picture showing superior flap covering raw superior bony part and inferior flap from right side covering raw inferior bony part. e) at the 6th month postoperatively, the endoscopic picture shows patent cavities on both sides. f) showing a diagrammatic representation of the creation of flaps on both sides, thus covering superior and inferior raw bony surfaces.
Follow-up and outcome
The patient was discharged on the 7th postoperative day and was instructed not to blow the nose. The patient was called for suction clearance of the nose every week for a month. The final evaluation was done at the 6th month post-operatively which revealed patent nasal cavities on both sides. There was no evidence of restenosis on further follow-ups till now.
The patient was discharged on the 7th postoperative day and was instructed not to blow the nose. The patient was called for suction clearance of the nose every week for a month. The final evaluation was done at the 6th month post-operatively which revealed patent nasal cavities on both sides. There was no evidence of restenosis on further follow-ups till now.
Discussion
Description of Choanal atresia was first given by Roederer in 1755. For the first time in 1854, it was managed surgically by Emmert. [3] Hengerer and Strome described four main embryological factors that can lead to Choanal atresia, which include (1) Persistent buccopharyngeal membrane (2) Persistent bucconasal membrane; (3) Presence of mesoderm at an abnormal location in the choanal region (4) Altered migration of neural crest cells leading to misdirected mesodermal flow in the facial processes. [4] Initially, the atretic plate causing obstruction was believed to be 10% cartilaginous and 90% bony in nature. Because of recent advancements in imaging techniques, the atretic plate is now believed to be bony-cartilaginous in nature in 70% and purely bony in 30 % of malformations. Bilateral choanal atresia is a very dangerous condition in neonates as they are obligate nasal breathers leading to severe respiratory distress and cyanosis thus making it a medical emergency requiring urgent surgical intervention. On the other hand, unilateral choanal atresia patients usually remain asymptomatic earlier but present with complaints of long-standing unilateral nasal obstruction or rhinorrhoea later in life, so are often diagnosed and treated for the same surgically at that point of time.
Diagnosis of choanal atresia can be made clinically which was earlier confirmed using choanography but now computed tomography is considered to be the investigation of choice for confirming the diagnosis. [5]. Choanal atresia can only be managed surgically. Various surgical approaches can be used for the repair of choanal atresia which includes trans-palatal, trans-antral, trans-septal, and trans-nasal approach. The trans-palatal approach provides a wide surgical field but complications like bleeding, defective growth of palate and jaw bone are more common with it. [6,7] The trans-antral approach is no longer used nowadays because of the complications associated with it. The trans-septal approach allows appropriate correction of septal deviations and mucosal flap preservation. It is recommended approach for unilateral choanal atresia cases (Age > 8 years). [8] The trans-nasal endoscopic approach is now the most commonly used and preferred approach for the repair of choanal atresia. The advantages of this approach being its safe, quick and provides excellent visualization of the nasal cavity, and avoids any bone growth retardation. [9,10] But this approach has disadvantages too like prolonged surgery time, bleeding, infection, bony palatal defect, synechiae formation, restenosis and long recovery time. In our case, there was unilateral choanal atresia of the left side where we used a trans-nasal endoscopic approach for its repair using a cross-over flap technique and an excellent result was obtained.
Conclusion
Choanal atresia is a rare congenital anomaly that requires prompt recognition and appropriate management to ensure adequate ventilation and feeding in affected infants. Multidisciplinary management is essential for successful treatment and prevention of complications. Trans-nasal endoscopic repair has shown to be an effective surgical technique for restoring nasal patency. Long-term follow-up is necessary to monitor the patient’s condition and address any potential issues that may arise.
References
- Schwartz MS, Savetsky L. (1986). Choanal atresia: clinical features,surgical approach, and long-term follow-up. Laryngoscope. 96: 1335–39.
- Leclerc JE, Fearon B. (1987). Choanal atresia and associated anomalies. Int J Pediatr Otorhinolaryngol. 13: 265-272.
- Evans, JNG, Machachlan, RF. (1971). Choanal atresia. J LaryngolOtol. 85:903–30.
- Hengerer AS, Strome M. (1982). Choanal Atresia: a new embryologic theory and its influence on surgical management. Laryngoscope. 92: 913-21.
- Crockett DM, Healy GB, McGillt J, et al. (1997). Computed tomography in the evaluation of choanal atresia in infants and children. Laryngoscope. 97: 174-83.
- Kwong KM. (2015). Current updates on choanal atresia. Front Pediatr. 3: 1-6
- da Fontoura Rey Bergonse G, Carneiro AF, Vassoler TM. (2005). Choanal atresia: analysis of 16 cases --- the experience of HRAC-USP from 2000 to 2004. Braz J Otorhinolaryngol. 71: 730-3.
- Hall WJ, Watanabe T, Kenan PD, Baylin G. (1982). Trans-septal repair of unilateral choanal atresia. Arch Otolaryngol. 108: 659-61.
- Carter JM, Lawlor C, Guarisco JL. (2014). The efficacy of mitomycin and stenting in choanal atresia repair: a 20 year experience. Int J Pediatr Otorhinolaryngol. 78: 307–11.
- Llorente JL, Lopez F, Morato M, Suarez V, Coca A, Suarez C, etal. (2013). Endoscopic treatment of choanal atresia. Acta Otorrinolaringol Esp. 64: 389–95.
Citation: Sahil Mogla, Apoorva Kumar Pandey and Aparna Bhardwaj. (2023). Transnasal Endoscopic Repair of Unilateral Choanal Atresia Using Cross-over Flap Technique: A Case Report. Journal of Otolaryngology - Head and Neck Diseases 5(1).
Copyright: © 2023 Apoorva Kumar Pandey. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.