Case Report
Volume 6 Issue 1 - 2024
Spontaneous CSF Fistula and Ethmoidal Meningoencephalocele. How to Act.
Department of ENT, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain
*Corresponding Author: Dr. Mayte Pinilla Urraca, Department of ENT and Head-Neck surgery Hospital Puerta de Hierro, Majadahonda, Madrid, Spain.
Received: March 01, 2024; Published: March 09, 2024
Abstract
This case report describes the presentation, diagnosis and management of a patient with an ethmoidal meningoencephalocele. A transethmoidal encephalocele is a rare entity within skull base encephaloceles. Typical symptoms are nonspecific and consist on nasal obstruction, clear rhinorrhea or even, they can present as an intracranial complication. Early diagnosis and treatment are essential in this case to avoid serious intracranial complications, with endoscopic approach being the gold standard.
Keywords: Meningoencephalocele; Ethmoidal; Endoscopic nasosinusal surgery; Intracranial hypertension
Abbreviations: CSF: Cerebrospinal Fluid Leaks; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; ESS: Endoscopic Nasosinusal Surgery
Introduction
Skull base meningoencephaloceles in adult patients are rare entities, occurring in the context of cranioencephalic trauma, iatrogenic injury or spontaneously [1]. Transethmoidal encephaloceles, as in the present case, comprise only 1-3% of cases, being a very rare location, generally of congenital origin, and may be associated with other craniofacial anomalies. [2]
The clinical presentation consists of nasal obstruction, rhinoliquorrhea, recurrent meningitis, epileptic seizures or neurological deficits [3]. The role of idiopathic intracranial hypertension has been described as a predisposing factor for the development of spontaneous encephaloceles at the base of the skull [1,4]. The management of this uncommon and rarely known pathology should be based on a multidisciplinary team of neurosurgeons and otolaryngologists. Given the possibility of fatal complications such as meningitis, pneumocephalus and brain abscess, surgical intervention is almost always required, with an endonasal endoscopic approach as the elective treatment, enabling a wide exposure of the skull base [5].
Case Report
We present the clinical case of a 64-year-old man with no relevant medical history, who reported left nasal congestion and clear fluid emission from his left nostril for the last 4 months, with no history of cranial trauma or other symptoms. He provided the result of a nasal fluid analysis at another clinic, with Beta2 transferrin positive of CSF. An endoscopic examination showed fluid emission at the level of the left middle meatus, a large unciform and a hypertrophic left middle turbinate. CT and MRI were requested as imaging studies (Figure 1), which reported a probable ethmoidal encephalocele, causing deformation of the left medial orbital wall, as well as the presence of an empty sella turcica and indirect signs of cerebral hyperpressure.
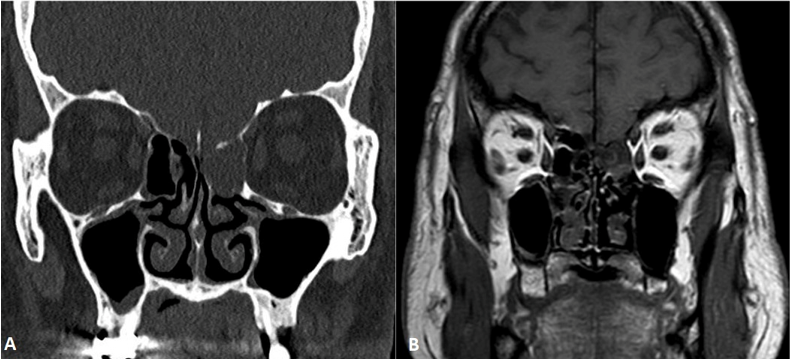
Figure 1: Coronal CT (A) and MRI slices (B). There is a defect in the roof of the left cribriform plate with herniation of brain content.
In view of these findings, the case was discussed in collaboration with the Neurosurgery Department and it was decided to perform surgery via endonasal approach, after lumbar puncture for the administration of intrathecal fluorescein to facilitate the vision of the fistula area and subsequently leave the lumbar drainage, with monitoring by the Neurosurgery Department to facilitate closure and prevent recurrence of the fistula. Prior to surgery, the patient was referred to the Preventive Medicine Service for pneumococcal vaccination.
An Endoscopic Nasosinusal Surgery (ESS) approach was performed with thermal reduction using bipolar forceps and resection of the meningoencephalocele in the left ethmoidal fovea and closure of the bony defect in 4 layers: periumbilical fat, haemostatic adhesive matrix, middle turbinate mucosa and biological sealant (Figure 2). The patient recovered well after the procedure, with closure of the drainage 5 days after surgery and surveillance for two more days, with no further incidents, and was discharged one week after surgery. After one year of follow-up, the patient is asymptomatic.
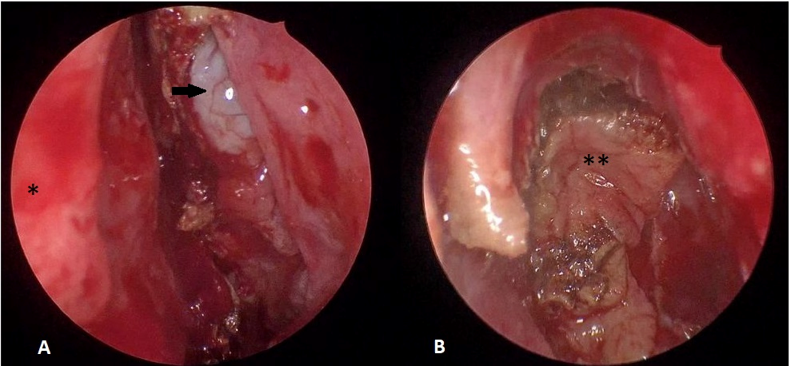
Figure 2: A. Intraoperative endoscopic image of ethmoidal encephalocele of the left nostril. B. Image after complete resection of the lesion and closure of the skull base defect, located in the ethmoid fovea. Septum (*). Encephalocele (→). Middle turbinate mucosa on defect (**).
Discussion
Encephaloceles of the anterior skull base may cause significant morbidity and mortality, so repair of the defect is essential if CSF leakage or meningitis occurs.
In contrast to patients with traumatic or postsurgical CSF leaks, patients with spontaneous encephaloceles and CSF leaks usually have broadly attenuated skull bases with large defects, probably because of fluctuations in their CSF pressure. Idiophatic empty sella syndrome like in this case, represent a milder form of intracranial hypertension. For these reasons, the placement of a lumbar drain during the initial perioperative period is recommended.
Successful endoscopic repair of these lesions allows the otolaryngologist to treat most of these defects without the morbidity of intracranial procedures. The main objective of surgical management is to resect the herniated non-functional brain parenchyma within the sac and reconstruct the skull base defect using materials such as abdominal fat, temporal aponeurosis, fascia lata, middle turbinate mucosa, biological glues or nasal pedicle flaps for closure [5,6]. In this case, once the meningoencephalocele was resected, a multilayer closure was performed using autologous periumbilical fat grafts, middle turbinate mucosa, fibrinogen and thrombin matrix and biological sealant.
In the published literature there are few reports of ethmoidal meningoencephaloceles in adults. Hallak et al [6] propose the endoscopic approach and treatment of a transethmoidal meningoencephalocele, in which middle turbinate mucosa is used as closure material, with good results and no recurrence. Another study [7] describes management by open approach, with favourable results, although it involves greater morbidity, and has currently been replaced by elective endoscopic management.
Rawal et al [8] report one of the largest series of cases of endoscopic repair of meningoencephaloceles according to location, with an 88% success rate after the first surgery, being the most frequent location in their series the ethmoid sinus, and using free mucosal graft in most cases, followed by abdominal fat and the use of the pedicled nasoseptal flaps. On the other hand, several retrospective studies [2,9] of congenital encephaloceles in childhood describe different endoscopic approaches depending on the location of the lesion in this population, with safe and effective results.
Conclusion
Spontaneous transethmoidal meningoencephaloceles are rare entities, in which factors such as CSF hyperpressure must be considered. The transnasal endoscopic approach has been shown to allow a successfull approach with low morbidity, even in large cases [10].
Multilayer reconstruction of the skull base defect provides solid and durable support. Control of intracranial hyperpressure [1,3,4] is essential to prevent recurrence, by placing a lumbar drain postoperatively or ventricle- peritoneal drain in the case of long-term recurrences.
References
- Kreatsoulas DC, Shah VS, Otto BA, Carrau RL, Prevedello DM, Hardesty DA. (2020). Surgical outcomes of the endonasal endoscopic approach within a standardized management protocol for repair of spontaneous cerebrospinal fluid rhinorrhea. J Neurosurg. 134(3): 780-786.
- Thompson HM, Schlosser RJ, McCarty Walsh E, Cho DY, Grayson JW, Karnezis TT, Miller PL. Woodworth BA. (2020). Current management of congenital anterior cranial base encephaloceles. Int J Pediatr Otorhinolaryngol. 131: 109868.
- Schlosser RJ, Bolger WE. (2002). Management of multiple spontaneous nasal meningoencephaloceles. Laryngoscope. 112(6): 980-5.
- Teachey W, Grayson J, Cho DY, Riley KO, Woodworth BA. (2017). Intervention for elevated intracranial pressure improves success rate after repair of spontaneous cerebrospinal fluid leaks. Laryngoscope. 127(9): 2011-2016.
- Nyquist GG, Anand VK, Mehra S, Kacker A, Schwartz TH. (2010). Endoscopic endonasal repair of anterior skull base non-traumatic cerebrospinal fluid leaks, meningoceles, and encephaloceles. J Neurosurg. 113(5): 961-6.
- Hallak B, Kurzbuch AR, Fournier J, et al. (2020). Spontaneous transethmoidal meningoencephalocele presenting in the form of recurrent unilateral nasal discharge: discussion of the diagnosis and endoscopic surgical management. BMJ Case Reports CP 13: e234703.
- Kubo A, Sakata K, Maegawa J, Yamamoto I. (2005). Transethmoidal meningoencephalocele in an elderly woman. Case report. Neurol Med Chir (Tokyo). 45(6): 322-6.
- Rawal RB, Sreenath SB, Ebert CS Jr, Huang BY, Dugar DR, Ewend MG, Sasaki-Adams D, Senior BA, Zanation AM. (2015). Endoscopic sinonasal meningoencephalocele repair: a 13-year experience with stratification by defect and reconstruction type. Otolaryngol Head Neck Surg. 152(2): 361-8.
- Castelnuovo P, Bignami M, Pistochini A, Battaglia P, Locatelli D, Dallan I. (2009). Endoscopic endonasal management of encephaloceles in children: an eight-year experience. Int J Pediatr Otorhinolaryngol. 73(8): 1132-6.
- López Arbolay O, Rojas Manresa J, González González J, Bretón Rosario JL. (2012). Gigant transethmoidal meningoencephalocele operated by full endonasal endoscopic approach: case report. Case Rep Med. 763259.
Citation: Elena Martin Bejerano, Antonio Martinez Ruiz- Coello, Beatriz Arellano Rodriguez and Mayte Pinilla Urraca. (2024). Spontaneous CSF Fistula and Ethmoidal Meningoencephalocele. How to Act. Journal of Otolaryngology - Head and Neck Diseases 6(1). DOI: 10.5281/zenodo.10799711
Copyright: © 2024 Mayte Pinilla Urraca. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
