Case Report
Volume 6 Issue 1 - 2024
Spindle Cell Lipoma of the Posterior Nasal Floor: A Case Report and Review
1Rutgers, Robert Wood Johnson Medical School, New Brunswick, NJ
2Coastal Ear, Nose, and Throat, Neptune, NJ
3Hackensack Meridian School of Medicine, Nutley, NJ
2Coastal Ear, Nose, and Throat, Neptune, NJ
3Hackensack Meridian School of Medicine, Nutley, NJ
*Corresponding Author: Dr. Josef Shargorodsky, Hackensack Meridian Medical School Jersey Shore University Medical Center, United States.
Received: March 22, 2024; Published: April 08, 2024
Abstract
A spindle cell lipoma is a benign, lipomatous neoplasm that typically arises within the subcutaneous tissue on the posterior neck or shoulder of older men. We report a case of a highly unusual presentation of a spindle cell lipoma in a female initially presenting with chronic nasal congestion non-responsive to pharmacological therapy. Computed tomography of the sinuses revealed bilateral pansinus mild to moderate mucosal thickening, right septal deviation and a large polypoid mass arising from the left posterior nasal cavity and filling the nasopharynx and much of the bilateral posterior nasal cavity. Final pathology of the excised mass obtained during endoscopic sinus surgery demonstrated a spindle cell lipoma. To date, there is generally limited literature documenting spindle cell lipomas involving the nasal or nasopharyngeal mucosa, and this is the first reported case of such a tumor arising from the posterior nasal floor.
Introduction
A spindle cell lipoma is a rare variant of lipoma. This benign neoplasm has a predilection for men over the age of forty-five [1]. A spindle cell lipoma most commonly arises in the subcutaneous tissue of the shoulder and posterior neck [1]. Histologically, spindle cell lipomas can be identified and differentiated from liposarcomas by the presence of mature adipocytes, collagen, and proliferated spindle cells[1]. Review of literature reveals rare instances of spindle cell lipomas arising in atypical locations, including the oropharynx, nasopharynx [2] face [3], scalp [4], lower extremities [5] and subungal [6]. Since the initial discovery of spindle cell lipomas in 1975, there have no cases documenting a nasal floor spindle cell lipoma.
Case Report
A 66-year-old female with a history of hypertension, osteoporosis and type 2 diabetes mellitus initially presented with chronic nasal congestion, mid facial pressure, post-nasal drip, and sore throat. She reported progressive symptoms with mouth-breathing developing over a period of two to three years. She initially presented to an allergist and underwent allergy testing, demonstrating allergies to all outdoor allergen classes. She was treated with topical steroids, topical and systemic antihistamines, and leukotriene inhibitors with no improvement in symptomatology. A sinus computed tomography was performed, showing bilateral pansinus mild to moderate mucosal thickening, rightward septal deviation, and a large polypoid mass filling the bilateral posterior nasal cavity and most of the nasopharynx (Figure 1). On fiberoptic nasal endoscopy performed in our office, a smooth polypoid mass was visible, filling the entire posterior left nasal cavity, most of the nasopharynx, and extending into the posterior aspect of the right nasal cavity. She was taken to the operating room for excision of the mass along with associated endoscopic sinus surgery. The polypoid lesion was truncated from its attachment to the posterior nasal floor but was too big for transnasal removal and was therefore removed transorally (Figure 2).
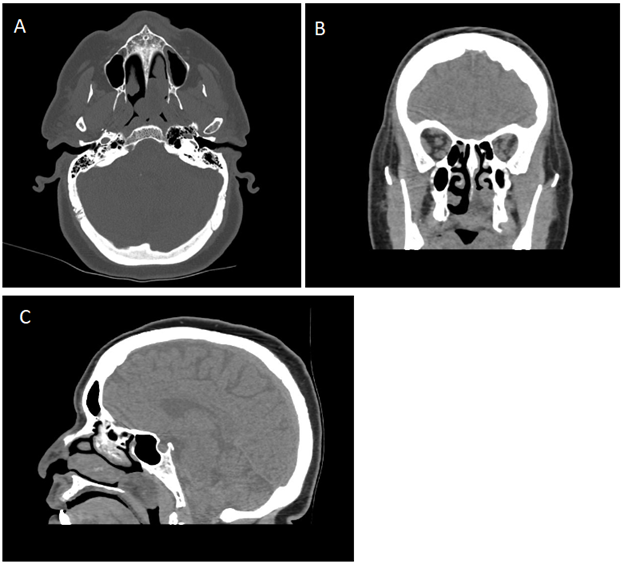
Figure 1: Preoperative radiographs of the left posterior nasal cavity mass. A. An axial film with bone windows shows an oval shaped posterior nasal cavity mass extending into the nasopharynx with no evidence of bony destruction or invasion. B. A representative coronal image of the tumor demonstrates it filling the left posterior nasal cavity down to the floor of the nose. C. A sagittal image of the tumor demonstrates it filling the posterior nasal cavity along the floor as well as extending into and filling much of the nasopharynx.
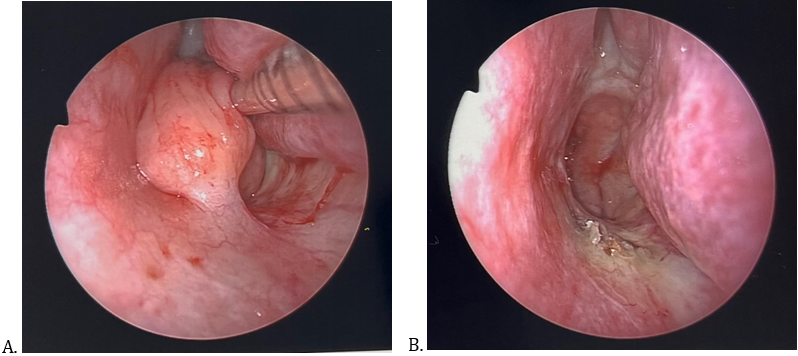
Figure 2: Intraoperative endoscopic images taken before and after left posterior nasal cavity spindle cell lipoma resection. A. Well circumscribed smooth tumor filling the posterior left nasal cavity and extending into the nasopharynx. It can be seen being pushed off the posterior aspect of the inferior turbinate. A thick stalk connects it to the nasal floor mucosa. B. A clean posterior nasal cavity and nasopharynx following resection of the lipoma. All of the mucosa is unaffected and preserved except for the mucosa adjacent to the nasal floor tumor attachment site.
This was sent to pathology and the initial frozen-section intraoperative report proved benign. Final pathological analysis revealed a 4.0 x 3.2 x 2.2 cm polypoid mass with subepithelium demonstrating a hypocellular proliferation of bland spindled to ovoid cells embedded in myxoid matrix with prominent intermixed ropy collagen fibers. There were numerous adipocytes throughout and numerous stromal mast cells. Immunostains showed that the proliferation was negative for SMA, Erg, and CD31 with no nuclear expression of beta-catenin, ruling out other benign and malignant sinonasal neoplasms. The findings were all consistent with a diagnosis of spindle cell lipoma (Figure 3). The patient underwent successful surgery, with routine postoperative recovery The patient underwent multiple routine postoperative visits, with no signs of recurrence 3 months postoperatively (Figure 4).
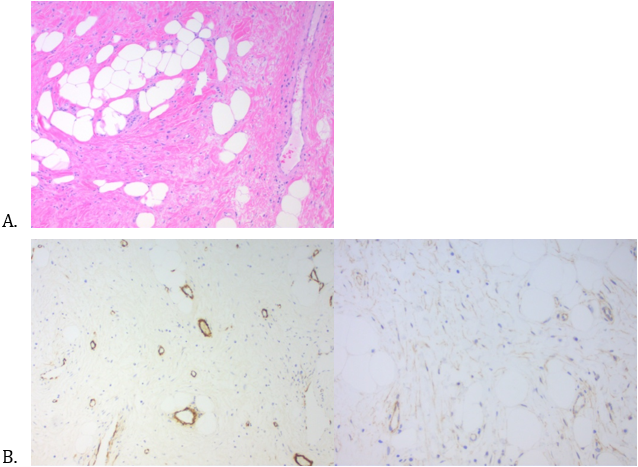
Figure 3: Pathology slide images of the mass. A. An H & E stain of the lesion shows benign sinonasal epithelium with areas of squamous metaplasia. The subepithelium demonstrates a hypocellular proliferation of bland spindled to ovoid cells embedded in myxoid matrix with prominent intermixed ropy collagen fibers. There are numerous adipocytes throughout as well as prominent thick-walled blood vessels and numerous stromal mast cells. B. Immunostains show the proliferation to be negative for SMA, Erg, and CD31 with no nuclear expression of beta-catenin.
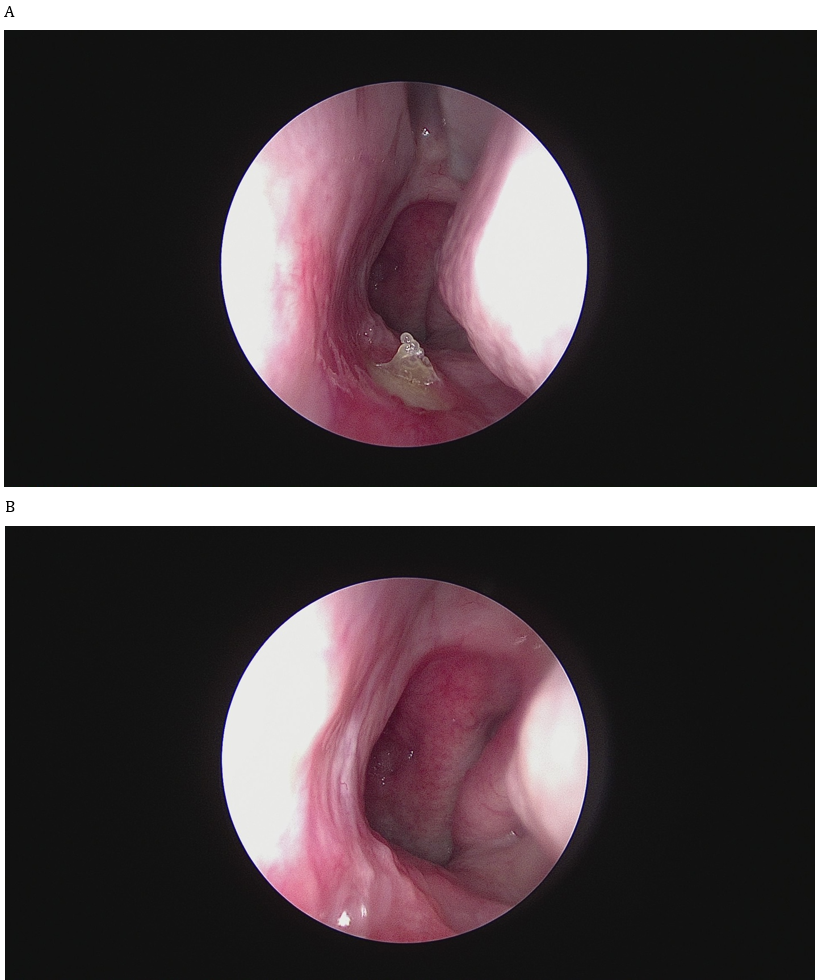
Figure 4: Postoperative follow up endoscopic views of the lipoma excision site. A. One week postoperative image shows an area of exposed bone at the site of lipoma excision at the posteiror nasal floor, with surrounding healing mucosa. B. Three months postoperative image demonstrates well healed mucosa with no evidence of residual disease.
Discussion
In 1975, Ezinger and Harvey were the first to delineate a spindle cell lipoma as a separate entity within adipocyte pathology. Accounting for 1.5% of adipocyte neoplasms [7], spindle cell lipomas can be differentiated from malignant pathologies from their histological findings and clinical presentation. Spindle cell lipomas demonstrate a predilection for the male gender and age greater than forty-five years old [1]. These lipomas characteristically present as a painless, slow-growing8 subcutaneous mass on the shoulder and posterior neck [1]. In the original investigation, this neoplasm was shown to be benign with low chance of recurrence [1]. Surgical excision is the treatment of choice.
Spindle cell lipomas may be incorrectly assessed as a well-differentiated liposarcoma/atypical spindle cell lipoma when presented in an infrequently encountered location [9]. Histopathological examination proves paramount in the diagnosis, as a spindle cell lipoma demonstrates characteristic findings on histology. On histology, a spindle cell lipoma can be identified by presence of mature adipocytes, collagen, and proliferated spindle cells [1]. Spindle cell lipomas can be further identified by diffuse expression of CD34 on immunohistology [10].
Rarely, spindle cell lipomas diverge from their typical presentation on the posterior neck and shoulder of adult men and arise in unusual locations. A literature review of documented respiratory spindle cell lipomas by Reid et al identified 24 cases from 1975 to March 2018. Excluding the oral cavity and oropharynx, the larynx accounted for the most spindle cell lipomas within the respiratory tract [2]. Of the twenty-four cases, two reports involved the nasopharynx and two involved the nasal cavity [2]. Another literature review of thirty-three cases of spindle cell/pleomorphic lipomas from 2000 to 2014 involving the face revealed the nose was the most common location, representing nine out of the thirty-three cases [3]. In those cases involving the nose, the spindle cell varied in depth, ranging from subcutaneous to dermal [3]. From the time of initial discovery of spindle cell lipomas forty-eight years ago, there have only been a few documented cases of nasal spindle cell lipomas.
A clinical diagnosis of spindle cell lipoma is less apparent when presented in a nonclassical manner. It has been suggested that pathologists may be hesitant to diagnosis a spindle cell lipoma when presented in such scenarios [5]. Radiological imaging offers little aid in diagnosis, as spindle cell lipomas have variable appearance and may be difficult to differentiate from a malignancy [11]. Variations in the fat to spindle cell ratio creates a wide spectrum of findings on imaging [12].
In this case, a spindle cell lipoma was not highly suspected. Although our patient’s age is within the typical range of a spindle cell lipoma, her female gender and anatomic location of the mass are rare occurrences for a spindle cell lipoma. Given the polypoid-like presentation on nasal endoscopy, a nasal polyp was the favored differential. Nasal polyps arise from the mucous membranes of the nose and paranasal sinuses [13] and are the most common benign neoplasm in the nasal cavity [14].
In summary, spindle cell lipomas are a variant of lipomas that seldomly originate in anatomic locations other than the shoulder and posterior neck. The propensity for this neoplasm to arise in older men has been well documented throughout the years. This case demonstrates an atypical presentation of a spindle cell lipoma involving a woman and nasal mucosa. Although rare, this case demonstrates the possibility of a nasal spindle cell lipoma as a potential etiology for an obstructive nasal cavity mass.
References
- Ezinger F, Harvey D. Spindle cell lipoma. Harefuah. 1979; 96 (10): 1852-1859.
- Reid J, Wehrli B, Sowerby LJ. (2019). Spindle Cell Lipomas of the Respiratory Tract: A Case Report and Comprehensive Literature Review. Ann Otol Rhinol Laryngol. 128(11).
- Cheah A, Billings S, Goldblum J, Hornick J, Uddin N, Rubin B. (2015). Spindle cell/pleomorphic lipomas of the face: An under-recognized diagnosis. Histopathology. 66(3).
- Haas AF, Fromer ES, Bricca GM. (1999). Spindle cell lipoma of the scalp: A case report and review. Dermatologic Surg. 25(1).
- Ud Din N, Zhang P, Sukov WR, et al. (2016). Spindle cell lipomas arising at atypical locations. Am J Clin Pathol. 146(4): 487-495.
- Subungual spindle cell lipoma: Case report. J Am Acad Dermatol. (2013); 68(4).
- FLETCHER CDM, MARTIN?BATES E. (1987). Spindle cell lipoma: a clinicopathological study with some original observations. Histopathology. 11(8): 803-817.
- Kubin DE, Lantto U, Lindgren O, Tasanen K. (2021). A Rare, Recurrent Spindle Cell Lipoma of the Nose. Acta Derm Venereol. 101(10).
- Azar SS, Buen F, Chia JJ, et al. (2021). Spindle Cell Lipoma Arising from the Supraglottis: A Case Report and Review of the Literature. Head Neck Pathol. 15(4).
- Templeton SF, Solomon AR. (1996). Spindle cell lipoma is strongly CD34 positive. An immunohistochemical study. J Cutan Pathol. 23(6).
- Jelinek JS, Wu A, Wallace M, et al. (2020). Imaging of spindle cell lipoma. Clin Radiol. 75(5): 396.e15-396.e21.
- Bancroft LW, Kransdorf MJ, Peterson JJ, Sundaram M, Murphey MD, O’Connor MI. (2003). Imaging Characteristics of Spindle Cell Lipoma. Am J Roentgenol. 181(5).
- Kalpana KMK, Mahadeva KC. (2013). Polypoidal lesions in the nasal cavity. J Clin Diagnostic Res. 7(6).
- Shirazi N, Bist SS, Selvi TN, Harsh M. (2015). Spectrum of sinonasal tumors: A 10-year experience at a tertiary care Hospital in North India. Oman Med J. 30(6).
Citation: Kokinakos, Konstandina, DiGiorgio, Cameron and Shargorodsky Josef. (2024). Spindle Cell Lipoma of the Posterior Nasal Floor: A Case Report and Review. Journal of Medical Research and Case Reports 6(1). DOI: 10.5281/zenodo.10960115
Copyright: © 2024 Josef Shargorodsky. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
