Case Report
Volume 4 Issue 1 - 2022
Clinical Characteristics and Outcomes among Patients Undergoing Laparoscopic Cholecystectomy at European Gaza Hospital: A Retrospective Cross-sectional Study
1Surgery Department, European Gaza Hospital, Ministry of Health, Gaza, Palestine
*Corresponding Author: Rami Aljbour, Surgery Department, European Gaza Hospital, Ministry of Health, Gaza, Palestine.
Received: November 27, 2022; Published: December 03, 2022
Abstract
Objective: To spot light on the clinical characteristics and outcomes of patients undergoing laparoscopic cholecystectomy at European Gaza Hospital.
Methods: A descriptive, correlational retrospective design was employed for this study. Since this study aims to assess clinical characteristics and surgical outcomes among patients undergoing laparoscopic cholecystectomy at a single point of time, this is the most appropriate design. This enables the researcher to measure the effect and the outcome at a single point of time. This study design gives reliable results with short time and less effort. The study was conducted at the surgery department at the European Gaza Hospital. Patients were recruited retrospectively during the period from January to October 2022.
Results: All cases included in the current study were electively managed and the preoperative hospital stay was one day among all patients, which is the day prior to the surgery. The duration after operation ranged from two to four days with most patients being discharged during 48 hours after the operation. There were 17 patients had a history of previous hospitalization (24.3%). Most of patients had ASA score of 1 or 2. Most of patients underwent the surgery due to complicated gallbladder stone and chronic cholecystitis. The mean time of surgery was 95 + 20 minutes with median duration of 90 minutes. There were 22 patients had a history of jaundice (31.4%). None of the patients received blood transfusion following the surgery. All patients received preoperative antibiotic prophylaxis. None of the patients were admitted to the ICU following the surgery and none of the patients’ surgeries was converted to open.
Conclusion: The current study showed the retrospective analysis of 70 laparoscopic cholecystectomy cases at European Gaza Hospital. Study results showed that all patients were electively surgically managed with laparoscopic approach. Patients had no complications, short hospitalization following the surgery and good surgical outcome at two weeks follow up. Most of study participants were females and from middle age group. None of participants were admitted to ICU or received blood after the surgery. All of patients had preoperative antibiotic prophylaxis. Good outcomes noticed in the current study is owing to the safe approach during the surgery and reflects good surgeons’ experience.
Keywords: Laparoscopic; Cholecystectomy; Surgery; Clinical outcome; Gaza
Introduction
Laparoscopic cholecystectomy is the gold standard for treating cholelithiasis, and it is successful and safe for many patients with symptomatic gallbladder stone disorders [1]. Previously conducted at a rate of between 5 and 7 lakhs annually [2], it has already surpassed even the commonest of all other operations in the United States. Benefits of laparoscopic cholecystectomy include faster recovery of bowel function, less postoperative discomfort, improved cosmetics, a shorter hospital stay, quicker return to full activity, and lower total cost [3,4]. The goal of this research is to identify risk variables associated with challenging laparoscopic cholecystectomy.
Laparoscopic cholecystectomy has largely replaced open cholecystectomy as the go-to procedure for treating cholelithiasis symptoms [5]. This is because laparoscopic cholecystectomy is a less invasive operation, meaning it causes less discomfort and allows for a quicker recovery. Laparoscopic cholecystectomy has been the gold standard for treating symptomatic gallstones since it was pioneered in 1989, however part of the planned LC requires conversion for various reasons [6].
The most effective therapy for gallstone symptoms is laparoscopic cholecystectomy (LC). There is decreased risk of surgical site infection (SSI) with LC [7] compared to open cholecystectomy (OC) [8]. In addition to OC, other factors have been linked to an increased risk of surgical site infection after cholecystectomy, such as the patient's age, the patient's gender, the duration of the surgical procedure, the number of surgical procedures the patient is undergoing, the severity of the patient's underlying medical condition, and the type of surgery being performed [8-11]. One study found that infection rates following cholecystectomy ranged from 1% to 14% [8,12].
Gallbladder disease is the most prevalent reason for abdominal surgery in the elderly [13, 14], and it is a prominent cause of hospital admission for acute abdomen in adults. The surgeon may need to switch to an open operation if using LC poses too many risks. However, the chance of conversion during LC for acute cholecystitis is greater than during an elective surgery [15]. Male gender, advanced age, prior endoscopic retrograde cholangiopancreatography (ERCP), a palpable gallbladder, elevated C-reactive protein (CRP) and white blood cell count (WBCC), gangrenous inflammation, and the experience of the operating surgeon have all been linked to an increased risk of conversion for patients undergoing LC for acute cholecystitis [16–19]. The rates of conversion and complications were not affected by conservative treatment with antibiotics and postponing the surgery until after the acute period [20]. There are greater difficulties, further surgeries, and longer hospital stays for patients who need a conversion [16].
When preparing for the cholecystectomy and determining who will carry it out, it is crucial to take into account any potential risk factors for conversion or difficulties. The complication risk for LC is lower among experienced surgeons than among trainees, according to research [17]. It is also crucial to educate the patient about the surgery and its potential risks.
Gallbladder disease is among the leading causes for hospital admission for acute abdomen among adults and the most common indication for abdominal surgery in the elderly. There are two options for the surgery according to the facility and surgeons experience; laparoscopic and open cholecystectomy. As surgery advances during the recent years, most centers perform laparoscopic cholecystectomy since it is associated with fewer complications when compared to open cholecystectomy [7]. Thus, this study aimed to assess the clinical characteristics and surgical outcomes among patients undergoing laparoscopic cholecystectomy at European Gaza Hospital.
Methods
Study Design
A descriptive, correlational retrospective design was employed for this study. Since this study aims to assess clinical characteristics and surgical outcomes among patients undergoing laparoscopic cholecystectomy at a single point of time, this is the most appropriate design. This enables the researcher to measure the effect and the outcome at a single point of time. This study design gives reliable results with short time and less effort.
A descriptive, correlational retrospective design was employed for this study. Since this study aims to assess clinical characteristics and surgical outcomes among patients undergoing laparoscopic cholecystectomy at a single point of time, this is the most appropriate design. This enables the researcher to measure the effect and the outcome at a single point of time. This study design gives reliable results with short time and less effort.
Study Setting
The study was conducted at the surgery department at the European Gaza Hospital. Patients were recruited retrospectively during the period from January to October 2022.
The study was conducted at the surgery department at the European Gaza Hospital. Patients were recruited retrospectively during the period from January to October 2022.
Participants
Participants in this study were patients admitted to the department following laparoscopic cholecystectomy. All study participants (patients) were above 18 years of age.
Participants in this study were patients admitted to the department following laparoscopic cholecystectomy. All study participants (patients) were above 18 years of age.
Sample and sampling
Since the study was a cross sectional study during a short period of time. Convenient non-probability sample was selected according to the availability of data in the patients’ records. Thus, the study included only adult patients admitted to the department during the study period.
Since the study was a cross sectional study during a short period of time. Convenient non-probability sample was selected according to the availability of data in the patients’ records. Thus, the study included only adult patients admitted to the department during the study period.
Data collection
Data was collected from patients’ medical records from the archive department
Data was collected from patients’ medical records from the archive department
Instruments
The data was collected using self-designed questionnaire based on latest literature. Study questionnaire contained three domains. First, characteristics of study participants. Second, assessment of surgical outcomes. Third, operative grading system, but this section was not filled due to the lack of data in patients’ records.
The data was collected using self-designed questionnaire based on latest literature. Study questionnaire contained three domains. First, characteristics of study participants. Second, assessment of surgical outcomes. Third, operative grading system, but this section was not filled due to the lack of data in patients’ records.
Statistical Analysis
Data obtained from questionnaire were entered and analyzed using SPSS program version 23 computer software. Sociodemographic data are presented using descriptive statistics as means, median, percentages and standard deviation. Independent T test and one-way Anova are used to show statistical significance among participants characteristics. Chi square test is used to show relationship between categorical variables.
Data obtained from questionnaire were entered and analyzed using SPSS program version 23 computer software. Sociodemographic data are presented using descriptive statistics as means, median, percentages and standard deviation. Independent T test and one-way Anova are used to show statistical significance among participants characteristics. Chi square test is used to show relationship between categorical variables.
Permission and ethical considerations
An approved permission was gained from Ministry of Health and Hospital Director to collect quantitative data from patients’ records. There was no need for informed consent since data was collected from medical records.
An approved permission was gained from Ministry of Health and Hospital Director to collect quantitative data from patients’ records. There was no need for informed consent since data was collected from medical records.
Results
Baseline characteristics
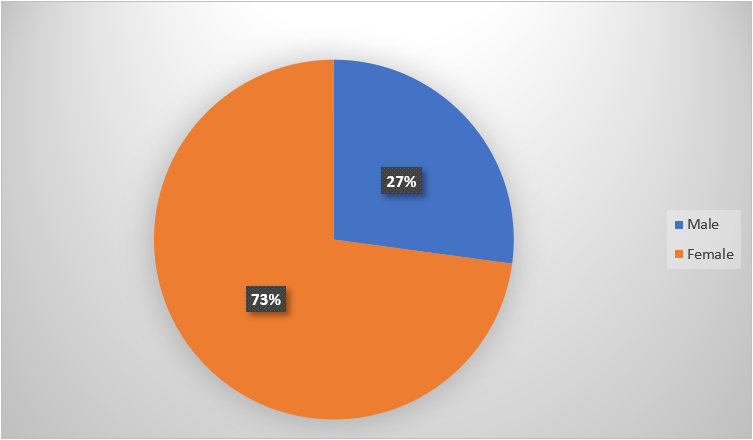
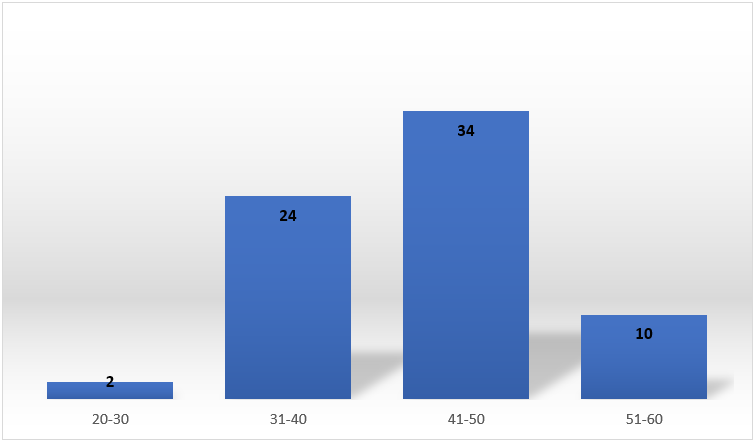
The study included 70 patients in which among them were 51 females (72.8%) and the rest were males. Patients’ age ranged from 20 to older than 60, with most frequent age groups were 41-50 (n= 34, 48.6%) and 31-40 (n= 24, 34.3%). Figure 1 and 2 shows frequency of participants gender and age groups included in the study respectively.
The study included 70 patients in which among them were 51 females (72.8%) and the rest were males. Patients’ age ranged from 20 to older than 60, with most frequent age groups were 41-50 (n= 34, 48.6%) and 31-40 (n= 24, 34.3%). Figure 1 and 2 shows frequency of participants gender and age groups included in the study respectively.
There were 7 patients who were smokers (10%) in which all of them were male patients. In addition, there were 16 patients had comorbid conditions such as diabetes (n= 5), hypertension (n= 9) and COPD (n= 2). These patients were on regular medications to manage their conditions. Most of patients had normal body mass index (18.5-24.9 kg/m2) (n= 41, 58.6%) (Table 1).
All cases included in the current study were electively managed and the preoperative hospital stay was one day among all patients, which is the day prior to the surgery. The duration after operation ranged from two to four days with most patients being discharged during 48 hours after the operation. There were 17 patients had a history of previous hospitalization (24.3%). Most of patients had ASA score of 1 or 2. Most of patients underwent the surgery due to complicated gallbladder stone and chronic cholecystitis.
| Variable | Frequency | Percent | |
| Comorbid condition | Diabetes Mellitus | 5 | 7.1% |
| Hypertension | 9 | 12.8% | |
| COPD | 2 | 2.8% | |
| Body Mass Index | 18.5 – 24.9 | 41 | 58.6% |
| 25 – 29.9 | 19 | 27.2% | |
| 30 – 34.9 | 10 | 14.2% | |
| History of jaundice | 22 | 31.4% | |
Table 1: Patients characteristics.
The mean time of surgery was 95 + 20 minutes with median duration of 90 minutes. There were 22 patients had a history of jaundice (31.4%). None of the patients received blood transfusion following the surgery. All patients received preoperative antibiotic prophylaxis. None of the patients were admitted to the ICU following the surgery and none of the patients’ surgeries was converted to open.
Discussion
Acute calculous cholecystitis treatment has standardized on LC. The risks of postoperative sequelae, particularly bile duct damage, and the likelihood of requiring a conversion to open cholecystectomy highlight the primary concerns about safety and practicality. The variables associated with conversion and complications after surgery were the primary focus of our research [18].
Independent preoperative risk factors for conversion were age more than 65 years, diabetes, and CRP greater than 150 mg/l. The multivariate analysis accounted for both preoperative and intraoperative observations, including serious inflammatory complications such as gangrene of the gallbladder and an abscess found by the surgeon [18]. However, this research [18] did not find a significant relationship between diabetes and CRP levels higher than 150 mg/l, which may be indicative of a link between diabetes and the development of gangrene and an abscess that result in elevated CRP levels. Studies have shown that both diabetes and gangrene enhance the likelihood of developing gangrenous cholecystitis [19-25]. However, recognizing gangrene and an abscess before surgery might be challenging, thus CRP levels and a history of diabetes may be more useful in evaluating the complexity of the intended treatment [18].
Other studies [20-26] have also shown that advanced age, diabetes, and CRP are risk factors for transformation. It has been hypothesized that older age is associated with a more extensive history of gallbladder illness, with symptoms being ignored or delayed in seeking treatment [20, 26]. In addition to a male gender and a history of abdominal surgery, [26] research has also connected them to conversion. Only seven patients (8.3%) were converted because of adhesions from prior operations; however, neither a history of abdominal surgeries nor male gender were considered risk factors in this analysis [18]. In the univariate analysis, the presence of an assistant was linked to a higher chance of conversion, most likely because assistants are often called in to help with the most difficult procedures. Therefore, we did not take the helper's presence into account as a possible conversion risk [18].
Conservative therapy followed by delayed cholecystectomy is discouraged in favor of early cholecystectomy [22, 27]. When to do a cholecystectomy to reduce the risk of complications and conversion is a topic of ongoing discussion [18]. Studies have shown that performing a cholecystectomy as soon as scheduling permits yields the same results in conversion and complications as surgery performed within 48 hours of admission [28, 29], while others have found that performing the procedure within 5 days of admission reduces the complication rate. Even in cases of acute cholecystitis when symptoms began more than 72 hours before hospital admission, a recent randomized study indicated that early LC leads in decreased morbidity and hospital stay compared to delayed cholecystectomy [30].
However, research did not find any connection between the length of time between admission and surgery or the overall duration of symptoms with conversion or complications [18]. Potentially at play here is a selection bias brought on by the earlier surgical intervention given to individuals whose conditions were clinically more severe. In addition, older individuals with several comorbidities may have had a more difficult time recognizing the beginning of symptoms. Antibiotic treatment was started soon after a diagnosis of cholecystitis was made, which may have helped to prevent further damage to the bile ducts. The lowest conversion rate was seen in those who arrived at the hospital less than 24 hours after the beginning of symptoms, suggesting that the absence of therapy for cholecystitis is more important than any potential delay in care. It's also feasible that the inflammatory response develops at an individual pace, with no apparent effect of passing time [18].
Independent risk variables for complications were age over 65, male gender, renal impairment, and open cholecystectomy as the final surgical procedure [18]. Compared to the 9-20% reported by previous research [20, 21], the total complication rate of 18.0% is within the expected range. In contrast to LC, the rate of complications following conversion was much greater. Given that older age, diabetes, and more advanced infection were all linked to conversion, it's plausible that they also lead to greater postoperative problems [18]. Additionally, switching to open surgery increased the risk of wound problems such as infection and rupture [18]. Other investigations on acute cholecystitis [20, 21, 25] have identified age, male gender, and gangrene as risk factors for sequelae. Age, male gender, and conversion have all been identified as risk factors for complications in studies of individuals undergoing both elective and emergency surgery [31, 32].
One percent of all cholecystectomies in this research resulted in bile duct damage (BDI), with open cholecystectomies having a BDI risk of 4.8% [18]. However, all bile duct lesions were treated endoscopically, and the vast majority were of Strasberg categorization type A [33]. The fact that no BDIs occurred in patients who got LC is reassuring evidence of the safety of LC, but it may also be attributable to the fact that all potentially dangerous procedures were changed to safer ones. Our relatively high conversion rate backs up this theory [18]. Other research [34-36] has shown BDI rates of 0.62–0.9% in LC and 0.38–1.24% in OC. Acute cholecystitis has been associated with a higher incidence of BDI than elective cholecystectomy [37], although the results of these investigations were inconsistent.
Although it was hypothesized that as LC grew more widespread, BDI rates would drop, this has not been the case so far, according to certain research [38]. There are also findings that show the reverse tendency, that BDI injuries are more likely following OC, which raises concerns about whether or not surgeons-in-training are acquiring the proper technique for OC in the laparoscopic age [35]. Although patients with more severe inflammation are more likely to be selected for conversion or direct OC, this does not rule out the possibility that patients whose surgeries are completed as open procedures are at risk for BDI due to inflamed, rupture-prone tissues rather than inadequate surgical technique [18]. When comparing the outcomes of general surgeons with cholecystectomy specialists, several studies have shown that the latter had a lower complication rate overall [19]. While we did not find such a link in our research, it is possible that the assignment of more clinically complex patients to experts skewed the results. Since patients should always be given the best treatment possible, conducting prospective randomized studies is inherently immoral [18].
The mortality rate in [18] (1.3% vs. 0.7%-1.1% in prior studies [20, 39]) was considerably higher. Patients who had fatal complications in this analysis were clinically classified as high-risk surgical patients due to the presence of several co-morbidities. Other than cholecystectomy, treatments for severe acute cholecystitis include antibiotics and interval cholecystectomy, or the use of percutaneous transhepatic cholecystostomy (PTHC), which may be followed by cholecystectomy. Interval cholecystectomy and PTHC have not yet been studied for their effects on subsets of high-risk surgical patients. In the Netherlands, researchers have begun a randomized controlled experiment to examine the efficacy of LC and PTHC in high-risk patients [18, 40].
Conclusion
The current study showed the retrospective analysis of 70 laparoscopic cholecystectomy cases at European Gaza Hospital. Study results showed that all patients were electively surgically managed with laparoscopic approach. Patients had no complications, short hospitalization following the surgery and good surgical outcome at two weeks follow up. Most of study participants were females and from middle age group. None of participants were admitted to ICU or received blood after the surgery. All of patients had preoperative antibiotic prophylaxis. Good outcomes noticed in the current study is owing to the safe approach during the surgery and reflects good surgeons’ experience.
References
- Torres K., Szuka?a M., Torres A., Pietrzyk ?., Maciejewski R. (2015). Assessment of the correlation between gender, age, body mass index and the severity of postoperative pain, nausea and vomiting in patients undergoing laparoscopic cholecystectomy. Pol. Merkur. Lek. 39 (229): 9-13.
- Lowndes Bethany, Thiels Cornelius A., Habermann Elizabeth B., Bingener Juliane, Hallbeck Susan, Yu Denny. (2016). Impact of patient factors on operative duration during laparoscopic cholecystectomy: evaluation from the National Surgical Quality Improvement Program database. Am. J. Surg. 212(2):289–296.
- George Bazoua M.D., Tilston MB Michael P. BS (2014). Male gender impact on the outcome of laparoscopic cholecystectomy. JSLS. 18(1): 50-54.
- Kassa1 Vijay. Sangeeta Nimbalka. (2017). Clinico-radiological assessment for prediction of difficult laparoscopic cholecystectomy. MedPulse– nternational Medical Journal. 4(Issue 2): 268–271.
- Atmaram D.C.1, Lakshman K. (2011). Predictive factors for conversion of laparoscopic cholecystectomy. 73(6):423-426.
- Bethany L., Cornelius A., Thiels D.O., Elizabeth B. Habermann.; Julia. (2016). Impact of patient factors on operative duration during laparoscopic cholecystectomy: evaluation from the National Surgical Quality Improvement Program database. Am. J. Surg. 212(2): 289-296.
- Duman K, Sezer KH, Yilmaz F, Akin ML. (2013). The clinical outcome of traditional laparoscopic Cholecystectomy. Gaziantep Med J; 19:35-9.
- Richards C, Edwards J, Culver D, Emori TG, Tolson J, Gaynes R. (2013). Does using a laparoscopic approach to cholecystectomy decrease the risk of surgical site infection? Ann Surg; 237:358-62.
- Rotermann M. (2014). Infection after cholecystectomy, hysterectomy or appendectomy. Health Rep; 15:11-23.
- Fahrner R, Malinka T, Klasen J, Candinas D, Beldi G. (2014). Additional surgical procedure is a risk factor for surgical site infections after laparoscopic cholecystectomy. Langenbecks Arch Surg. 399:595-9.
- Mu Y, Edwards JR, Horan TC, Berrios-Torres S, Fridkin SK. (2011). Improving risk-adjusted measures of surgical site infection for the national healthcare safety network. Infect Control Hosp Epidemiol. 32:970-86.
- den Hoed PT, Boelhouwer RU, Veen HF, Hop WC, Bruining HA. (2018). Infections and bacteriological data after laparoscopic and open gallbladder surgery. J Hosp Infect; 39:27-37.
- Miettinen P, Pasanen P, Lahtinen J, Alhava E. (2016). Acute abdominal pain in adults. Ann Chir Gynaecol. 85:5-9.
- Ukkonen M, Kivivuori A, Rantanen T, Paajanen H. (2015). Emergency Abdominal Operations in the Elderly: A Multivariate Regression Analysis of 430 Consecutive Patients with Acute Abdomen. World J Surg. 39:2854-61.
- Giger UF, Michel J-M, Opitz I, Th Inderbitzin D, Kocher T, Krahenbuhl L. (2016). Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 203:723-8.
- Dominguez LC, Rivera A, Bermudez C, Herrera W. (2011). Analysis of factors for conversion of laparoscopic to open cholecystectomy: a prospective study of 703 patients with acute cholecystitis. Cir Esp. 89: 300-6.
- Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. (2016). Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 93:844-53.
- Terho PM, Leppäniemi AK, Mentula PJ. (2016). Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World journal of emergency surgery. Dec;11(1):1-9.
- Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. ? ( 2016). Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 93:844-53.
- Wevers KP, van Westreenen HL, Patijn GA. (2013). Laparoscopic cholecystectomy in acute cholecystitis: C-reactive protein level combined with age predicts conversion. Surg Laparosc Endosc Percutan Tech. 23:163-6.
- Eldar S, Sabo E, Nash E, Abrahamson J, Matter I. (2017). Laparoscopic Cholecystectomy for Acute Cholecystitis: Prospective Trial. World J Surg. 21:540–5.
- Gutt CN, Encke J, Koninger J, Harnoss J-C, Weigand K, Kipfmuller K, et al. (2013). Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. 258:385-93.
- Dindo D, Demartines N, Clavien P-A. (2014). Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205-13.
- Bourikian S, Anand RJ, Aboutanos M, Wolfe LG, Ferrada P. (2015). Risk factors for acute gangrenous cholecystitis in emergency general surgery patients. Am J Surg.; 210:730-3.
- Ganapathi AM, Speicher PJ, Englum BR, Perez A, Tyler DS, Zani S. (2015). Gangrenous cholecystitis: a contemporary review. J Surg Res. 197:18-24.
- Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ. (2015). Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc. 19:905-9.
- Lo CM, Liu CL, Fan ST, Lai EC, Wong J. (2018). Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 227:461-7.
- Banz V, Gsponer T, Candinas D, Guller U. (2011). Population-based analysis of 4113 patients with acute cholecystitis: defining the optimal time-point for laparoscopic cholecystectomy. Ann Surg. 254:964-70.
- Chandler CF, Lane JS, Ferguson P, Thompson JE, Ashley SW. (2010). Prospective evaluation of early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Am Surg. 66:896-900.
- Roulin D, Saadi A, Di Mare L, Demartines N, Halkic N.? (2016). Early Versus Delayed Cholecystectomy for Acute Cholecystitis, Are the 72 hours Still the Rule? A Randomized Trial Ann Surg. 264:717-22.
- Murphy MM, Ng S-C, Simons JP, Csikesz NG, Shah SA, Tseng JF. (2010). Predictors of Major Complications after Laparoscopic Cholecystectomy: Surgeon, Hospital, or Patient? J Am Coll Surg. 211: 73-80.
- Roslyn JJ, Binns GS, Hughes EF, Saunders-Kirkwood K, Zinner MJ, Cates JA. (2013). Open cholecystectomy. A contemporary analysis of 42,474 patients. Ann Surg. 218:129-37.
- Strasberg SM, Hertl M, Soper NJ. (2015). An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 180:101-25.
- Diamantis T, Tsigris C, Kiriakopoulos A, Papalambros E, Bramis J, Michail P, et al. ? ( 2015). Bile duct injuries associated with laparoscopic and open cholecystectomy: an 11-year experience in one institute. Surg Today.; 35:841-5.
- Karvonen J, Salminen P, Grönroos JM. (2011). Bile duct injuries during open and laparoscopic cholecystectomy in the laparoscopic era: alarming trends. Surg Endosc. 25: 2906-10.
- Viste A, Horn A, Ovrebo K, Christensen B, Angelsen J-H, Hoem D. (2015). Bile duct injuries following laparoscopic cholecystectomy. Scand J Surg. 104: 233-7.
- Tornqvist B, Waage A, Zheng Z, Ye W, Nilsson M. (2016). Severity of Acute Cholecystitis and Risk of Iatrogenic Bile Duct Injury During Cholecystectomy, a Population-Based Case-Control Study. World J Surg. 40: 1060-7.
- Slater K, Strong RW, Wall DR, Lynch SV. (2012). Iatrogenic bile duct injury: the scourge of laparoscopic cholecystectomy. ANZ J Surg. 72: 83-8.
- Scollay JM, Mullen R, McPhillips G, Thompson AM. (2011). Mortality associated with the treatment of gallstone disease: a 10-year contemporary national experience. World J Surg. 35: 643-7.
- Kortram K, van Ramshorst B, Bollen TL, Besselink MGH, Gouma DJ, Karsten T, et al. (2012). Acute cholecystitis in high-risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy (CHOCOLATE trial): study protocol for a randomized controlled trial. Trials. 13:7.
Citation: Rami Aljbour and Alaa Abu Elsebah. (2022). Clinical Characteristics and Outcomes among Patients Undergoing Laparoscopic Cholecystectomy at European Gaza Hospital: A Retrospective Cross-sectional Study. Journal of Medical Research and Case Reports 4(1). DOI: 10.5281/zenodo.7398229
Copyright: © 2022 Rami Aljbour. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.